Information
Journal Policies
ARC Journal of Immunology and Vaccines
Volume-1 Issue-1, 2016
Summary
Spondylodiscitis is a disease which defined as osteomyelitis of vertebral bodies and infection of intervertebral disc. Spondylodiscitis constitute approximately 3-5% of all cases of osteomyelitis. Spondylodiscitis are classified as pyogenic, granulomatous (tuberculosis, brucellosis, fungal-factor) and parasitic infections aetiologically. Tuberculosis is one of the most common reason of spinal infections in the worldwide. It constitutes up to 9-46% of cases in developed countries. Tuberculosis spondylodiscitis constitutes only 2% of all tuberculosis cases. Vertebral tuberculosis is most common type of skeletal tuberculosis. It is seen in more than 50% rates in bone and joint tuberculosis cases. When compared to other pyogenic discitis, it is an important cause of morbidity due to cause severe tissue destruction. In this study, we present a case who have tuberculosis spondylodiscitis and an accompanying psoas abscess.
2.KEYWORDS
3.INTRODUCTION
4.CASE
5.DISCUSSION
6.REFERENCES
AUTHOR DETAILS
Muge OZGULER1, Mehmet OZDEN2
1Elazıg Educational and Research Hospital Infectious Diseases and Clinical Microbiology Departmant, Elazıg, Turkey.
2Fırat University Medical Faculty Infectious Diseases and Clinical Microbiology Departmant, Elazıg, Turkey.
[email protected]
KEYWORDS
Discitis; Tuberculosis; Psoas Abscess
INTRODUCTION
Spondylodiscitis is defined as infectious involvement of vertebral corpus with intervertebral discs. The disease creates 3-5% of all tuberculosis cases (1). In developing countries, the incidence of disease is 4-24 million patients per year (2-5). Spinal infections are classified according to the etiology as pyogenic granulomatous (Tuberculosis, Brucellosis, fungal-factor) and parasitic.
Although the etiology of spondylodiscitis includes a lot of microorganisms, mono-microbial bacterial infections are extremely common. S. aureus is the most common microorganism in non-tuberculosis cases. It is seen with rate of 20-84%. Brucella constitutes 21-48% of spinal infections in endemic areas (6).
The tuberculosis is one of the most common causes of spinal infection in the world wide. It constitutes 9-46 % of cases in developed countries. Spinal tuberculosis constitutes 2% of all tuberculosis cases (5-7). In this report we want to present a case with tuberculosis spondylodiscitis and accompanying bilateral psoas abcess.
CASE
67-year-old male patient was admitted to hospital with back pain which increasing by movement and ongoing for three months. Intermittent fever and night sweats were the complaints of the patient. Patients had also complained of loss of appetite and weight loss as well as 20 kilos. The left shoulder pain related to tenosynovitis about ten days ago was learned from his history.
Patient had any other chronic diseases. But it was learned that he was diagnosed and treated as pleural empyema three years ago. In this period, patient had been investigated, but any evidence in favor of tuberculosis has not been obtained.
In his physical examination, fever was 36. 8°C, pulse rate was 82/min, blood pressure was 120/80 mmHg. Decreased breath sounds at medium and basal of the left lung was revealed at patient's lung examination. Movement limitation in both lower extremities due to pain was revealed in his neuromuscular system examination. In addition that bilateral laseque and femoral stretch tests were positive.
His white blood cell count was 6300 K/μL (Neutrophil 60%, Lymphocyte: 26%, monocyte 7%) Hemoglobin was 9.7 g/dl, Hematocrit was % 30,4, platelets was 479000 K/μL, sedimentation was 105 mm/h, CRP was 9.93 mg/L, AST was 19 IU/L, ALT was 19 IU/L, ALP was 296 U/L, GGT was 170 U/L, total and direct bilirubin level was normal. Blood sodium level was 127 mEq / ml. Renal function tests and urinalysis were normal.
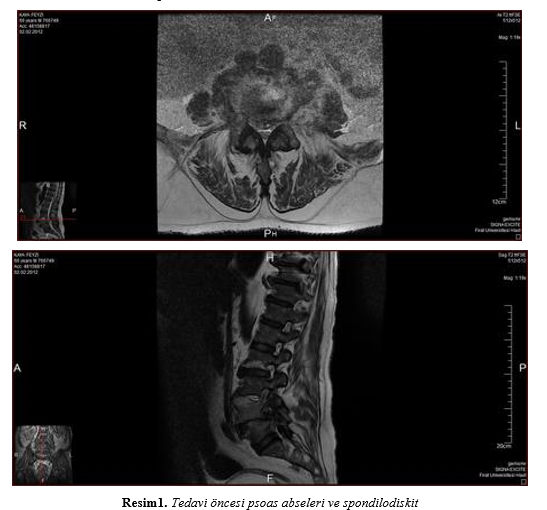
Brucella Wright test and coombs test were resulted negative. Tuberculin skin test was applied and resulted negative. Persistant fever was observed at patient’s follow up. Lumbar MRI with contrast was filmed due to the patient's back pain. MR results were obtained as intensity increases and contrast enhancement at L3-L5 vertebral corpus and disc involvement with some pedincules, adjacent anterior and posterior wall thickening and contrast enhancement (epidural phlegmone) and 67x35 mm left psoas abcess and 27x19 mm right psoas abcess (Figure 1). Any pathological contrast enhancement wasn’t revealed in his thoracic spine MRI.
Chest tomography was taken. Mediastinal calcified lymph nodes, 12 mm pleural effusion at left lung, adjacent atelectasis, bilateral several pulmonary nodules has been observed at chest tomography.
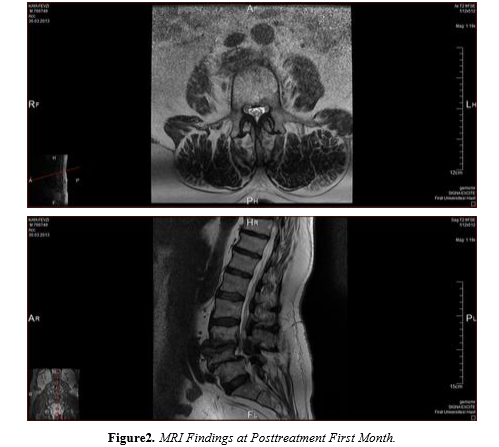
Percutaneous drainage catheter was placed into the left psoas abscess the with the help of ultrasound probe. Positive findings were not detected from abcess dreinage fluid staining. Methicillin-sensitive Staphylococcus aureus was obtained from drainage fluid culture. Anaerobic cultures and tuberculosis cultures were negative. The abscess related findings were revealed from histopathological examination. Adenosine deaminase (ADA) levels were studied from drainage fluids. Because of determining ADA level >200 IU/L, isoniazid, rifampicin, pyrazinamide and ethambutol therapy was began and combined with cefazolin therapy. Cefazolin treatment was applied during three weeks. Total 3500 cc drainage fluid was collected from abcess and regretion was observed at 24. days of treatment. The psoas abscess disappeared at control lumbar MRI 's which was taken 35 days of treatment and decreasing at disc and epidural involvement was detected. Antituberculous treatment was applied during 12 months. contrast-enhanced MR Complete disappearance of the psoas abscess was observed in the first month of treatment (Figure 2).
DISCUSSION
Tuberculosis is an important pathogen causing morbid spinal disease in the world wide. Vertebral tuberculosis is the most observed type among bone and joint tuberculosis. In recent years, overall tuberculosis cases has been observed decreasing, but it is still a disease that can be observed in the older age groups. When compared to other pyogenic discitis it is seen as more serious bone and leads to tissue destruction. Therefore, tuberculosis related spondylodiscitis is an important cause of morbidity. In tuberculosis spondylodiscitis, disc involvement is more prevalent than in pyogenic spondylodiscitis. In pyogenic infection, there is no involvement in the posterior elements. However, later in the period, posterior elements may be accompanying to clinic entitiy. This situation causes difficulties in differential diagnosis (11-13).
In pyogenic infections, paraspinal soft tissue involvement are observed in one third of the cases and neurological deficits rate is 4-17% in these patients (13). In our case, bone and paraspinal tissue destruction was determined, posterior elements involvement was observed.
Clinical signs of lumbosacral tuberculosis is similar as other spondylodiscitis. These symptoms are pain, muscle spasms, radiculopathy, motor and sensory loss, neurological findings of compression. However, fever, anorexia and constitutional symptoms such as weight loss can be observed. serious complications of tuberculosis Spondylodiscitis are psoas abscess, bone destruction and spinal cord compression. Usually, these complications are seen when insufficient or inappropriate was given (13).
Psoas abscess occurs about 5% of cases in the presence of Pott's disease. Psoas abscess are assessed in two categories as primary and secondary. While there is no obvious source at primary psoas abscess, secondary psoas abscess arises from another infected focus. Pott disease related psoas abscess is a rare condition. Usually, secondary psoas abcess occurs. But previously primary psoas abscess has been published (11). Due to the presence of previously undiagnosed empyema is considered to be secondary psoas abscess in our case. Psoas abscess is usually a case of subacute on chronic and insidious. Therefore, delay is observed in the diagnosis. In this case causes delayed treatment and increased morbidity (9-11). Psoas abscess are usually unilateral. Bilateral psoas abscess are rare clinic condition. A few report related to biliateral psoas abscess has been published in the literature (8,9). Bilateral psoas abscess which was developed subacute and chronic basis was detected in our case.
The classic triad of the psoas abscess are fever, back and lumbar pain, hip restriction signs in action are seen only 35% of cases. Fever, weight loss and constitutional symptoms can be observed only in 40% of patients. Neurological deficits caused by tuberculosis spondylodiscitis were observed in 40% of cases. If clinical findings such as progressive back pain, muscle spasm and rigidity are seen, it is necessary to suspect abscesses (9-11).In our case the clinical symptoms such as fever, limitation of movement, back pain and constitutional symptoms have been observed.
Clinical suspicion is prominent for the diagnosis of psoas abscess and we need good clinical examination and diagnostic tests. Promote CT / MRI scans are also required together with microbiological and histopathological examination. Radiographically, osteopenia, narrowing of the disk surface and the end plate erosion can be seen and paravertebral soft tissue shadows may be accompanied. In Magnetic resonance imaging, bone-marrow edema, end plate erosion, presence of granulation tissue and abscess formation may be seen. Aspiration of the abscess should be performed both diagnostic and treatment purposes (8-10). Tissue culture and histopathological examination are the most important factor for diagnose. However, it takes a long time and typical histological findings are not usually observed (13).
Psoas abscess is often drained by percutaneous drainage guided by ultrasound when drainage requires. Antituberculosis drugs should be combined to drainage simultaneously (13,14). In our case we applied ultrasound guided drainage to the left side abscess and drainage of mycobacterial culture and histopathological variables were assessed. But diagnostic contribution was not achieved.
Antituberculosis treatment for tuberculosis spondylodiscitis should be continued until clinical and radiological improvement is achieved. Bhojraj 's study, fifteen patients, which have large abscesses and neurological deficits caused by granulation tissue and neural compression, have been evaluated. Decreasing at abscess sizes with antituberculosis drugs has been emphasized in this study (8). American Thoracic Society recommends 6-9 months of antituberculosis therapy of bone and joint tuberculosis (14). Antituberculosis treatment is given in a total of 12 months in our case. MR findings were observed completely disappeared after treatment.
Pyogenic bacterial superinfection can accompany Spondylodiscitis tuberculosis simultaneously in some patients. There is a similar case in the literature (13). In our case, methicillin-sensitive Staphylococcus aureus culture was obtained from drainage culture simultaneously. We were not able to get a positive culture results or ARB postivity in favor of tuberculosis but we have achieved positive ADA result from drainage fluid. The diagnosis of tuberculosis spondylodiscitis and pyogenic superinfection was confirmed with this evidences.
As a result; spondylodiscitis tuberculosis is an important clinical condition with high morbidity in developing countries. Psoas abscess formation can occur when diagnose delayed. In some rare cases, such as in our case, bilateral psoas abscess and pyogenic super infection may be faced and this may lead to misinterpretation.
REFERENCES
- Snider GL. Tuberculosis then and now: a personal perspective on the last 50 years. Ann Intern Med 1997;126(3):237-243.
- Jensen AG, Espersen F, Skinhoj P, Rosdahl VT, Frimodt-Møller N. Increasing frequency of vertebral osteomyelitis following Staphylococcus aureus bacteraemia in Denmark 1980–1990. J Infect 1997;34(2):113–8.
- Espersen F, Frimodt-Moller N, Thamdrup Rosdahl V, Skinhøj P, Bentzon MW. Changing pattern of bone and joint infections due to Staphylococcus aureus: study of cases of bacteremia in Denmark, 1959–1988. Rev Infect Dis 1991;13(3):347–58.
- Sobottke R, Seifert H, Fatkenheuer G, Schmidt M, Gossmann A, Eysel P. Current diagnosis and treatment of spondylodiscitis. Dtsch Arztebl Int 2008;105(10):181–187.
- Mylona E, Samarkos M, Kakalou E, Fanourgiakis P, Skoutelis A. Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin Arthritis Rheum 2009;39(1):10–17.
- Gouliouris T, Aliyu SH, Brown NM. Spondylodiscitis: update on diagnosis and management. J Antimicrob Chemother 2010;65(3):11–24.
- Di Martino A, Papapietro N, Lanotte A, Russo F, Vadalà G, Denaro V Spondylodiscitis: standards of current treatment. Curr Med Res Opin 2012;28(5): 689-99.
- Bhojraj S, Nene A. Lumbar and lumbosacral tuberculous spondylodiscitis in adults. Redefining the indications for surgery. J Bone Joint Surg Br. 2002;84(4):530-534.
- Elnaim AL. Bilateral Psoas Abscess and Extensive Soft Tissue Involvement Due to Late Presentation of Pott's Disease of the Spine. Indian J Surg. 2011;73(2):161-162.
- Goni V, Thapa BR, Vyas S, Gopinathan NR, Rajan Manoharan S, Krishnan V. Bilateral psoas abscess: atypical presentation of spinal tuberculosis. Arch Iran Med. 2012;15(4):253-256.
- Chawla K, D'Souza A, N SB, Mukhopadhayay C. Primary tubercular psoas abscess: a rare presentation. J Infect Dev Ctries. 2012;6(1):86-88.
- Namisato S, Nakasone C, Okudaira S, Touyama M, Ishikawa N, Higa H, et al. A case of afebrile miliary tuberculosis that progressed from tuberculous spondylitis with iliopsoas abscess. Intern Med. 2010;49(19):2151-2155.
- Kim YM, Cha JH. Delayed diagnosis of tuberculous spondylitis masked by concomitant methicillin resistant Staphylococcus aureus infection. J Korean Neurosurg Soc. 2010;47(3):235-238.
- Blumberg HM, Burman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN et al. American Thoracic Society/Centers for disease control and prevention/infectious diseases society of America: Treatment of tuberculosis. Am J Respir Crit Care Med 2003;167(4):603-662.