Information
Journal Policies
Incidence of Ambulatory Care Visits and Association with Comorbidities of Overactive Bladder in Taiwan
Hsin-Li Liu1,Kai-Yu Tseng2,Shu-Ching Chiu3,Horng-Mo Lee4,Yueh-Chin Chung5
2.School of Medical Laboratory Sciences and Biotechnology, Taipei Medical University, Taipei, Taiwan.
Copyright :© 2017 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Objectives: The present study is designed to explore the incidence of ambulatory care visits and association with comorbidities of overactive bladder (OAB) in Taiwan.
Methods: Data from the National Health Insurance Research Database(LHID) 2005 containing all of the original claim data of 1,000,000 beneficiaries enrolled in 2005 were randomly sampled from the 2005 Registry for Beneficiaries (ID) of the NHIRD and then statistically analyzed in terms of percentage, incidence of ambulatory care visits , odds ratio (OR), and 95% confidence intervals.
Results: The subjects enrolled in this study included females (62.93%) mostly aged 51 to 60 years (19.97%) and males (19.68%) aged 71 to 80 years. The ratio of females to males was 0.8–2.51:1.0. Overall, the annual incidence of ambulatory care visits increased from 2.1% in 2006 to 2.9% in 2009. The annual incidence of ambulatory care visits of females and males reached the maximum of 3.5% and 2.3% in 2009. In females, comorbidities, such as frequent urination, urinary incontinence (UI), and urinary calculi, and menopause (OR>1; P< 0.05). In males, frequent urination, nocturnal enuresis, UI, benign prostatic hypertrophy and anxiety state (OR>1; P< 0.05) were associated with OAB.
Conclusions: The incidence of ambulatory care visits of patients with OAB in Taiwan was low. OAB may significantly affect the quality of life. Thus, the medical attention and effective treatment for patients with OAB should be enhanced.
Abbreviations: OAB: overactive bladder, UI: urinary incontinence, UUI: urge urinary incontinence, SUI: stress urinary incontinence, LUTS: lower urinary tract symptoms, ICD: international classification of diseases, NHIRD: National Health Insurance Research Database, OR:odds ratio.
overactive bladder; incidence; ambulatory carevisits; comorbidities; National Health Insurance Research Database,Urology
1. Introduction
Overactive bladder (OAB), a common but easily neglected condition accompanied with bladder hypersensitivity or contraction abnormalities and often resulting in urgent urination, frequent urination, nocturnal enuresis, or urinary incontinence (UI), causes embarrassment and may interfere with normal life[1]. Wein and Rovner emphasized that OAB covers a very wide range, including urge urinary incontinence (UUI), a portion of mixed UI, a portion of stress urinary incontinence (SUI)[2], and a sense of urgency in urine, which is the main symptom of OAB[3].
The prevalence of OAB also increases with age, that is, 12% to 22% of affected individuals are over 40 years old and 30% to 40% of such individuals are over 75 years old; one-third of these patients present signs of UI[4]. Stewart, Herzog, and We in reported that 21 million people in the United States experience urinary frequency and urinary urgency but not UI, and 3.3 billion patients manifest OAB[5]. The attack rate of OAB may increase with age, and 60% showed symptoms, but only 27% received treatment. The prevalence of OAB may also increase with age and may affect 5.9% to 16% of males and 6.0% to 16.9% of females [6].Moorthy, Lapitan, Quek, and Lim surveyed 2,369 male patients with a mean age of 18 to 70 years in 11 Asian countries in 1998 and found that 709 patients (29.9%) suffered from OAB, and 43.0% of these patients were at the working age; the incidence of OAB increased with age, and the age group of over 70 years accounted for 53.0%[7]. Abrams et al. indicated that females present a higher risks of OAB than males [8].
About 10% to 18% of the Taiwanese population showed varying degrees of OAB, and the prevalence rate increases with age. Among 23 million Taiwanese, approximately 4.14 million people are at a serious risk of OAB, but only 13% of these individuals have sought medical attention [9]. The prevalence of OAB among females aged over 20 years in Taiwan is 36.0%[10]. Irwin et al. estimated that 0.303 billion females aged more than 20 years will experience UI, 0.255 billion females will suffer from stress incontinence, 53 million females will complain of mixed incontinence, and 33 million of females will manifest UI by 2018; approximately 0.298 billion individuals will suffer from OAB[11]. The prevalence of UI among females is greater than that among males, and their medians correspond to 27.6-58.4% and 10.5%[12,13].
The risk factors of OAB in females include urinary tract infection, SUI, interstitial cystitis, menopause, polyuria, diabetes, heart failure, medication, and aging (P< 0.05)[14,15]. The risk factors of OAB for males are aging, constipation, and prostate enlargement (P< 0.05)[16,17]. Surgical treatments, cystic calculus, obesity, and neurological abnormalities, such as stroke, Parkinson’s disease, anxiety, and lower urinary tract symptoms (LUTS), are also factors contributing to OAB[18]. The prevalence of LUTS is 41%, which increases with age; for the age groups of 18 to 49, 50 to 64, and ≥ 65 years, the prevalence rates correspond to 14.1%, 41.5%, and 60.8%[19], and SUI accounts for about 50%[20,21].
With regard to the effects of OAB on living quality, the survey results in the 11 Asian countries showed that 53% of Asian women have developed symptoms of OAB, but only 21% of these women have sought medical attention. The 2014 survey in Taiwan also revealed that 35% of Taiwanese women were aware of their OAB symptoms. OAB symptoms often negatively affect the social life, work, mood, family life, and sex life of patients and thus seriously affect their quality of life [18,19,22-29].
With the effects of OAB symptoms on their careers, the daily work of 24.9% of male patients is affected and job decisions for 10% of male patients are underdetermined and thus prompt them to change jobs or become dismissed; early retirement is documented in 7.8% of male patients; female patients also experience similar cases [6,28].
OAB affecting the quality of life in the healthcare system has been extensively investigated. Therefore, this study examined the annual incidence of ambulatory care visits, gender ratio, and comorbidity of OAB by using the relevant data from the National Health Insurance Research Database of Taiwan from 2003 to 2010 and by providing research data regarding the current condition of OAB in Taiwan and other factors to predict its future condition.
2. Materials And Methods
This paper presents a longitudinal study with data sourced from the relevant outpatient and medical insurance files of LHID 2005. The LHID 2005 contains all the original claim data of 1,000,000 beneficiaries enrolled in 2005 and randomly sampled from the 2005 Registry for Beneficiaries (ID) of the National Health Insurance Research Database (NHIRD), which was released once every 40,000 beneficiaries were sampled and then updated once a year. In this study, the column (ACODE_ICD9_1) of the international classification of diseases(ICD) in the outpatient files (CD) of the National Health Insurance Research Database is cited, with the first three codes in front of the ICD representing the current diagnosis of a subject investigated, thereby obtaining the primary diagnostic distribution and dividing the diagnosis districts into 18 groups.
The present study included 503 males and 854 females, comprising a total of 1,357 subjects. The patients enrolled were diagnosed of OAB from 2003 to 2010 (ICD-9-CM: 596.51 patients). The diagnostic codes of comorbidities are as follows: diabetes mellitus (250), multiple sclerosis (MS) (340), secondary parkinsonism (332.1), renal calculus (592), ureteral calculus (592.1), acute cystitis (595), frequent urination (788.41), nocturnal enuresis (788.43), UI (788.31), other urination abnormalities (788.69), benign prostatic hypertrophy (BPH) (600), menopause (627.2, 627.8, 627.9), and anxiety state (300.00, 300.02, 300.09). This study was approved by the NHRI Review Committee and by the Institutional Review Board of the China Medical University Hospital, Taichung, Taiwan (CMUH103-REC1-088).
SPSS17.0 statistical software was used for data reduction and subsequent analysis. The age/sex distribution of 2003 to 2010 OAB patients was analyzed in terms of percentage. The annual consultation rate was calculated on the basis of gender to provide data of the current situation of OAB in Taiwan. The presence of OAB comorbidity in different genders is quantified by odds ratio (OR). Accordingly, 95% confidence interval was used for correlation and significance. The significance level (α) was set to 0.05.
3. Results
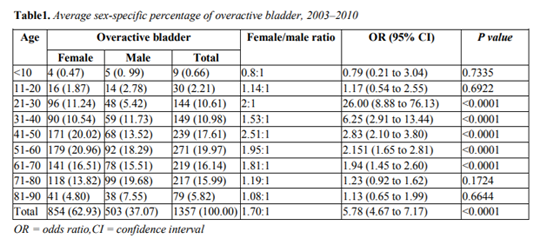
In this study, 503 males and 854 females, comprising a total of 1,357 cases, were enrolled. After the age/ gender grouping, 918 cases were found to present hereditary OAB, and the control group was composed of 1,827 subjects. The subjects enrolled were mostly at the age of 51 to 60 years old (19.97%). Among these subjects, females accounted for 62.93%, and most of them are at the age of 51 to 60 years old (20.96%); majority of males are at the age of 71 to 80 years old (19.68%). The gender ratio of females to males was 0.8–2.51:1.0, and this ratio varies with age. Differences were found between the genders, particularly in the age groups of 21 to 30, 31 to 40, 41 to 50, 51 to 60, and 61 to 70 years old (P< 0.0001) (Table 1).
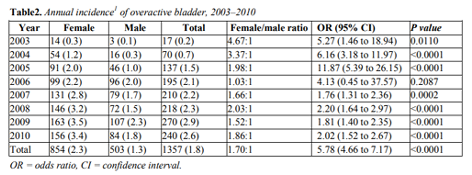
As shown in Table 2, the overall annual incidence of ambulatory care visits increased from 2.1% in 2006 to 2.9% in 2009; the annual incidence of ambulatory care visits of females reached the maximum by up to 3.5% at most in 2009, whereas that of males reached the peak at 2.3% in 2009; differences were found in terms of gender in the annual incidence of ambulatory care visits in 2004, 2005, 2008, 2009 and 2010 (P< 0.0001).
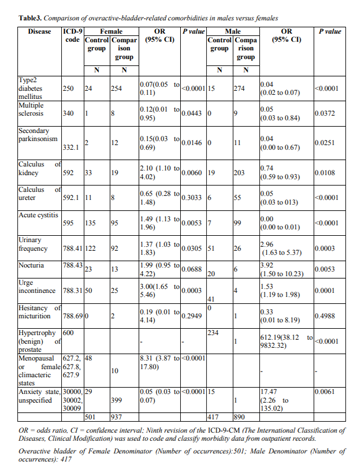
After the age/sex grouping, 918 hereditary OAB cases and 1,827 non-hereditary OAB cases were included for analysis. In terms of the comorbidity of OAB, the OAB-related comorbidities among females included renal calculus, acute cystitis, frequent urination, UI, and menopause (OR>1; P< 0.05), whereas those among males involved frequent urination, nocturnal enuresis, UI, BPH, and anxiety state (OR>1; P< 0.006). Up to 48 females with hereditary OAB showed menopausal symptoms, and 10 females with non-hereditary OAB presented menopausal symptoms. The risks for females with hereditary OAB complications and menopausal symptoms were 8.31 times as those of the normal group (95% CI 3.87-17.80); 50 females with hereditary OAB showed UI symptoms, whereas 25 cases with non-hereditary OAB presented such symptoms. The risks for females with hereditary OAB complications and UI were thrice as those of the normal group (95% CI 1.65-5.46); 33 females with hereditary OAB exhibited renal calculus, and 19 females with non-hereditary OAB displayed renal calculus. The risks for females with hereditary OAB complications and renal calculus were 2.10 times as those of the normal control group (95% CI 1.10 -4.02). Up to 234 males with hereditary OAB presented BPH symptoms, whereas only one male with non-hereditary OAB demonstrated such symptoms. The risks for males with hereditary OAB complications and BPH symptoms were 612.19 times as those of the normal control group (95% CI 38.12-9832.32); 15 males with hereditary OAB were in anxiety state, whereas only one male with non-hereditary OAB was in the same state. The risks for males with hereditary OAB complications and remaining in anxiety state were 17.47 times as those of the normal group (95% CI 2.27-135.02). Twenty males with hereditary OAB presented nocturnal enuresis symptoms, and only six males with non-hereditary OAB showed such symptoms. The risks for males with hereditary OAB complications and nocturnal enuresis symptoms were 3.92 times as those of the normal control group (95% CI 1.50-10.23) (Table 3).
4. Discussion
The present study is the first to explore the consultation rate of OAB in Taiwan on the basis of massive nationwide data. This study, which is characterized by large sample size and massive medical data, is relatively objective, and this study covers the deficiencies of previous studies in terms of various factors, including follow-up, response rate, or recall bias.
The subjects investigated were mainly at the age of 51 to 60 years old (19.97%). Females with OAB were mostly at the age of 51 to 60 years old (20.96%), whereas males with such diseases were at the age of 71 to 80 years old (19.68%). These findings indicate that the incidence of OAB may increase with age [13].
The results showed that more females suffer from OAB; in terms of OAB incidence, the ratio of females to males is 0.8–2.51:1.0; at the age of 21 to 70 years old, females are in the majority with greater risks for developing OAB than males[8]. Overall, the annual incidence of ambulatory care visits among all the subjects increased from 2.1% to 2.9% in 2006; the annual incidence of ambulatory care visits of females was 3.5% at most, whereas that of males was 2.3%; differences were found between genders in the annual incidence of ambulatory care visits in 2004, 2005, and 2008 up to 2010 (p< 0.0001); the average incidence of ambulatory care visits of females was 2.3%, which was higher than that of males (1.3%). About 10% to 18% of the Taiwanese population suffer from OAB; in particular, the prevalence of OAB among females over 20 years old was up to 36.0%[10], but only 13% of them have ever sought for medical attention[6]. As relevant survey results showed, compared with other countries, 60% of the European population suffer from OAB symptoms, and only 27% of them have received treatment[5]. The incidence of OAB among females in Switzerland was 20%, and the cure rate was 42%[11]. The results showed that the incidence of ambulatory care visits of OAB in Taiwan was low on the basis of the sampling results of the NHIRD because (1) the Orientals are more conservative, and they often think that urinary tract disease is a disease to be ashamed of; thus, they are unwilling to seek medical attention; and (2) many people consider that urinary incontinence is a sign of normal aging, without the need of seeing a doctor, thus delaying the optimal time for treatment and seriously affecting the quality of life[29]. The prevalence of LUTS was 41%, which may increase with age[19], and SUI approximately accounted for 50% of this prevalence[20,21].
OAB comorbidities among females include frequent urination. Milson et al. (2001) reported that the attack rate of OAB is 16.6%, and 85% of OAB patients develop frequent urination; the attack rate increases with age, in which 60% presented symptoms, but only 27% received treatment. The risks for females with hereditary OAB complications developing UI are 3.00 times as the normal control group, and the prevalence of UI among females varies significantly from 4.8% to 58.4%. The prevalence of UI roughly increases with age, and the most common symptom of UI is SUI, approximately accounting for 50% [2,13]. The study on Swedish females from 1991 to 2007, the incidence of UI was 21%, and the cure rate was 34%; although the cure rate was not low, 66% of the females have suffered from UI in the 16 years. The risks for females with hereditary OAB developing menopause and those for females with OAB complications suffering from menopausal symptoms were generally 8.31 times as those of the normal control group because post-menopausal females easily leak urine as a result of reduced secretion of female hormones and urethral mucosal atrophy [15].
The risks for males with OAB hereditary complications developing nocturnal enuresis symptoms were generally 3.92 times as those of the normal control group. In epidemiological studies on LUTS, such as those on UI, about 41% to 62% of males suffered from LUTS, the incidence among adults over 60 years old increased up to 60.8% to 81%[19,29], and SUI approximately accounted for 50%[20]. LUTS such as frequent urination, nocturnal enuresis, urgent urination, UI, difficulty in urination, intermittent urination, and acute urinary retention are all typical benign BPH symptoms. The risks for males with hereditary OAB complications and BPH symptoms are generally 612.18 times as those of the normal control group. LUTS and BPH symptoms are also important contributory factors to OAB, negatively affecting sleep quality and mental health[18,19,27,30]. The risks for males with hereditary OAB complications and remaining in an anxiety state were generally 17.47 times as those of the normal control group. Milsom[6,18]
found in his studies on the effects of OAB on patients’ personal development in marketplace that 2% or 3% of OAB patients are in anxiety state, and they often worry about accidents sometimes happening in the rush.
However, certain limitations affect this study. For example, additional physiological data are impossible to access as evidence from NHIRD. As such, only ICD9-CM can be used to distinguish diseases. If patients are unaware that such symptoms are curable or they fail to seek medical treatment, they are slipping through the present study. In addition, the coverage of NHIRD is very limited in terms of education, lifestyle, or social support. Therefore, data collection in the form of questionnaire or qualitative survey is recommended in the future to completely control the effects of other factors.
In Conclusion, a systemic review on the relevant literature worldwide indicated that OAB may significantly affect work and life quality and increase healthcare spending, and the healthcare spending on OAB patients may increase with age. The statistics of the consultation rate in the present study are relatively low. The literature verified that the prevalence of OAB is far above the actual consultation rate. Thus, the consultation and effective curative rates should be improved.
Acknowledgements
This study was supported by a grant from the Central Taiwan University of Science and Technology (CTU105-PC-008).
References
- Wein AJ, Rovner ES.Definition and epidemiology of overactive bladder. Urology 2002;60:7-12.
- Abrams P, Hanno P, Wein A.Overactive bladder and painful bladder syndrome:There need not be confusion. Neurourol Urodyn 2005; 24:149-150.
- Hung M J, Ho ES, Shen PS,et al. Urgency is the core symptom of female overactive bladder syndrome, as demonstrated by a statistical analysis. J Urol 2006; 176:636-640. The Gallup group in collaboration with pharmacia& Upjohn. Data on file, 1998.
- Stewart W, Herzog R, Wein AL.On behalf of the NOBLE program research team: Prevalence and impact of overactive bladder in the US: Results from the NOBLE program. Neurourol Urodyn 2001; 20: 24.
- Milson I, Abrams P, Cardozo L, Roberts RG, Thuroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how they are managed? A Population-based prevalence study. British Journal of Urology 2001; 87: 760-766.
- Moorthy P, Lapitan MC, Quek PL, Lim PH. Prevalence of overactive bladder in Asian men: An epidemiological survey. British Journal of Urology 2004; 93:528-531.
- Abrams P, Kelleher CJ, Kerr LA, Rogers, RG. Overactive bladder significantly affects quality of life. American Journal of Managed Care 2000; 6: S580-590.
- Li Weijia, Zhuang Yaoji.Talking about overactive bladder, Chang Gung Medical News 2016; 37:1.
- Chen GD, Lin TL, Hu SW, Chen YC, Lin LY. Prevalence and correlation of urinary incontinence and overactive bladder in Taiwanese women. Neurourology &Urodynamics 2003; 22:109-117.
- Irwin DE, Kopp ZS, Agatep B, Milsom I, Abrams P. Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU Int 2011; 108:1132-1138.
- Minassian VA, Drutz HP, A1-Badr A.Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet 2003; 82:327-338.
- Smith AL, Wein AJ.Contemporary management of overactive bladder. Postgrad Med 2012; 124:104-116.
- Neymark AI, Voytenko AN, Bondarenko AV, MuzalevskayaNI,KruglykhinIV. DIAGNOSIS AND TREATMENT OF OVERACTIVE BLADDER SYNDROME IN PELVIC INJURIES.Urologiia 2015; 5:38-42.
- Wen-Tsang Hsu. Prevalence of Lower Urinary Tract Symptoms and Urinary Incontinence inWomen of the Matsu area of Taiwan. An unpublished Thesis, Institute of Clinical Medicine of National Taiwan University, Taipei. 2006.
- Wu JW, Xing YR, Wen YB, et al. Prevalence of Spina Bifida Occulta and Its Relationship With Overactive Bladder in Middle-Aged and Elderly Chinese People. Int Neurourol J 2016; 20:151-158.
- Eapen RS, Radomski SB, Review of the epidemiology of overactive bladder Res Rep Urol 2016; 8:71-76.
- Golabek T, Skalski M, Przydacz M, et al. Lower urinary tract symptoms, nocturia and overactive bladder in patients with depression and anxiety. Psychiatr Pol 2016; 50:417-30.
- Cambronero Santos J, Errando Smet C.Prevalence of storage lower urinary tract symptoms in male patients attending Spanish urology office. Urinary urgency as predictor of quality of life. Actas Urol Esp 2016; Jun 23. pii: S0210-4806(16)30056-0.
- Minassian VA, Drutz HP,A1-Badr A.Urinary incontinence as a worldwide problem. Int J Gynaecol Obstet 2003; 82:327-338.
- Smith AL, Wein AJ.Contemporary management of overactive bladder. Postgrad Med 2012; 124:104-116.
- Mao-Rong Sun. 2016. Overactive Bladder (OAB). [Cited August 21, 2016].Available from http://www.cch.org.tw/cchhec/knowledge_detai l.aspx?oid=113.
- Choi H, Bae JH. Overview of the Epidemiology of Lower Urinary Tract Dysfunction in South Korea. Int Neurourol J 2016; 20:91-100.
- White N, Iglesia CB.Overactive Bladder. Obstet Gynecol Clin North Am 2016; 4 3:59-68.
- Reynolds WS, Fowke J, Dmochowski R. The Burden of Overactive Bladder on US Public Health. Curr Bladder Dysfunct Rep 2016; 11:8-13.
- Kobelt-Nguyen G, Johannesson M, Mattiasson A, Abrams P. Correlations between symptoms of urge incontinence and scores of a generic quality of life instrument (SF36) and health status measurements (EuroQoL) and between changes in symptoms and QoL scores (abstract). 27th Annual Meeting of the International Continence Society, Yokohama, Japan, September 23–7, 1997.
- Coyne K, Revicki D, Hunt T, et al. Psychometric validation of an overactive bladder symptom and health-related quality of life questionnaire: The OAB-q. Quality of Life Research 2002; 11: 563-574.
- Gu J, Restorick JM, Blank MA, et al. Vasoactive intestinal polypeptide in the normal and unstable bladder.Br J Urol 1983; 55:645-647.
- Rechberger T, Kulik-Rechberger B, Miotła P,Wrobel A. The new era in the pharmacological treatment of overactive bladder (OAB): mirabegron-a new selective beta3 agonist. Ginekol Pol 2014; 85:214-219.
- Kinsey D, Pretorius S, Glover L, Alexander T. The psychological impact of overactive bladder: A systematic review. J Health Psychol 2014; 21:69-81.