Information
Journal Policies
Functional Results after Anterior Cruciate Ligament Reconstruction with Isquiotibial Graft: Analytic Study of Two Kinds of Graft
Josafat Yair Arroyo-Aparicio MD1, Gabriel Partida Cota MD2, Alberto Robles Mendez Hernandez MD3, Pedro Leonardo Villanueva Solorzano MD3, Diana Laura Rodriguez Romero MD4, Jose Eduardo Vallejo Ramirez MD4, Haizel Valencia Romero MD4, Christopher Israel Valencia Romero MD4, Maria Fernanda Escandon Velazquez MD4, Adolfo De la Rosa Perez MD4, Yazmin Frias Lucio MD5, Luis Angel Medina Andrade MD4*
2.Medical Student, Escuela Medico Naval, Universidad Naval, Hospital Regional Naval de Mazatlán, Sinaloa, México.
3.Could you change this affiliation please for the next: General Surgery Service, La Salle University, Hospital Angeles Metropolitano, Mexico City, Mexico.
4.General Surgery Service, Hospital General de Zona #30, Instituto Mexicano del Seguro Social, IMSS, Mexico City, Mexico.
5.Occupational Medicine Service, Hospital General de Zona #32, Mexico.
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
The arthroscopic treatment of the anterior cruciate ligament lesions with the use of a graft of hamstring tendons for their reconstruction is very useful and presents good functional results. However, the selection of technique and kind of graft still controversial. We aim to compare the functional results between the use of semitendinous internal rectus or semitendinous graft for the treatment of anterior cruciate ligament lesions.
Material and Methods: A total of 45 patients from June 2017 to June 2018 were included. Variables like physical activity, age, sex, affected knee, Lachmann, Pivot -shift, Lysholm, and Sf-36 probes results were compared between both groups and analyzed.
Results: From the 45 patients included, 20 receive the semitendinous internal rectus graft and 25 the semitendinosus graft. The median age was 32 +/- 8.5 years, with 86.7% of males, working for the marine infantry (MI) with a 46.7% of the postsurgical patients, and associated meniscal lesions in 64% of the cases. Comparing both grafts with the Lysholm test Sf-36 it has been demonstrated that there no exist a significant difference between the results of on graft over the other.
Conclusion: The use of isquiotibial grafts is a good option for the reconstruction of the anterior cruciate ligament, with good functional results, taking in account that there is no significant difference between one and other graft.
Anterior cruciate graft, graft, isquiotibial, semitendinous, internal rectus, Lysholm test,Surgery
1. Introduction
In the naval field, patients with anterior cruciate ligament lesion are active military, with demandant physical activities every day, the reason why is so important to incorporate them as soon as possible to their work and daily activities, with the minimal functional sequelae, diminishing the life quality and adequate service activities develop. This study is a retrospective one, reviewing the files of each patient and do not need additional studies.
The rupture of the anterior cruciate ligament (ACL) is a common lesion around the world. The incidence is about 35 for every 10,000 people of all ages. This rupture frequently results in knee instability, increased articular laxity and activity reduction, with an increased risk of knee osteoarthrosis at long-term[1].
The patients with the diagnosis of secondary articular instability after ACL rupture suffer from knee functional limitation, and an arthroscopic intervention is needed to reconstruct the ligament with a graft[2]. In the Hospital Regional Naval de Mazatlan, Mexico, the isquiotibial grafts (semitendinous and internal rectus) are the most used, for his reason is necessary to evaluate the obtained functional results to determine the effectivity of those procedures.
This work seems to evaluate if there exists a functional difference between the use of isquiotibial grafts after ACL reconstruction.
2. Material And Methods
A non-experimental, observational, transversal, comparative and retrospective study was carried on in the Hospital Regional Naval de Mazatlan, Mexico. For the functional evaluation after ACL plasty the test of LACHMAN and PIVOT-SHIFT was used to evaluate articular stability, the LYSGHOLM test was used to evaluate the knee functionality and the SF-36 test was used to estimate the perception of health by the patients.
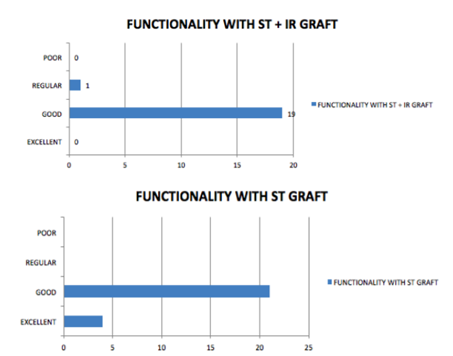
The Lysholm test was used to evaluate the knee functionality in a subjective manner by the patient. The qualification under 65 points was considered poor; between 66 to 83 regular; from 84 to 94 good and above 95 points excellent.
The SF-36 test was used to evaluate the health state of the patients in 8 areas, according to the patient perception. A punctuation is between 0 to 100, and a higher punctuation represents a better health The data was collected from the patient's files and introduced in the Excel program for their statistic analysis. The positive or negative results in the Lachmann and Pivot-Shift test were registered too.
The patients with surgery for ACL plasty with isquiotibial graft treated in the Hospital Regional Naval de Mazatlán in the period between June 2017 and June 2018 were included. A total of 45 patients were studied from which 20 patients were treated with semitendinous internal rectus graft and 25 patients with semitendinous graft.
To elucidate if there is a functional difference between the use of ST+IR graft or ST graft only in the treatment of ACL rupture.
3. Results
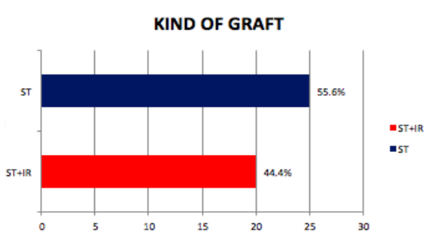
For the analysis of the results, the program Excel of Microsoft office with Windows 10 was used for descriptive data, with stratification according to the used graft. From a total of 54 patients, 9 were excluded for incomplete files. In total 45 patients were analyzed, 20 from the ST+IR group and 25 from the ST group (Figure 2). The ST graft has a total of 55.6% vs the ST+IR with 44.4%.
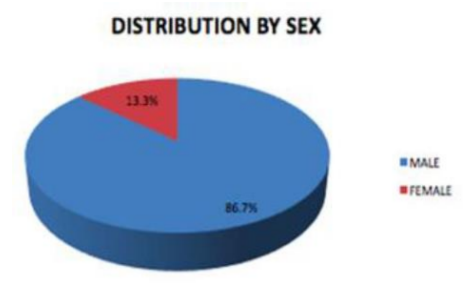
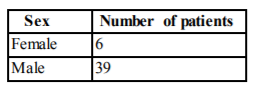
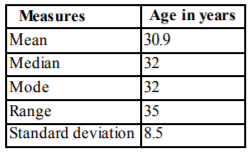
The general distribution by sex was 39 men and 6 women (Table 5, figure 3). The age range was from 16 to 51 years, with an average of 30.9 years and a standard deviation of 8.5 years, the median of 32 years, mode of 32 years and a male: female ratio of 3.6:1 (Table 6).
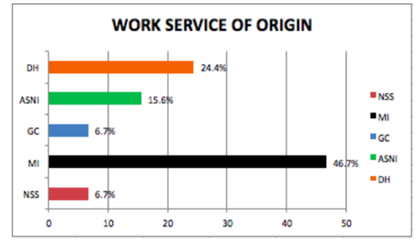
DH: With access to hospital service, SAIN: Administration Service of Naval Intendency, CG: General Marine Corps, IM: Marine Infantry, SSN: Naval Sanity Service. From Clinical Files of the HOSNAVTLA From the total studied patients, 3 are from the Naval Sanity Service, 21 from the Marine Infantry, 3 from the general marine corps, 7 from the Administration Service of Naval Intendency, and 11 with access to hospital services (figure 4).
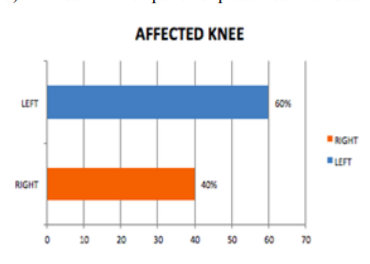
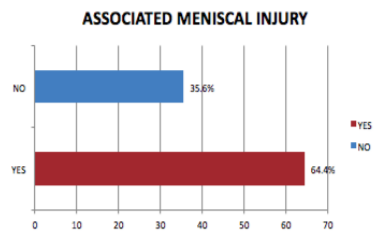
All patients go through rehabilitation, 27 had a left knee injury and 18 right knee injury (Figure 5). A total of 29 patients presented meniscal associated injury (Figure 6), and from the total 13 are marine infantry (48.8% of the associated meniscal injuries).
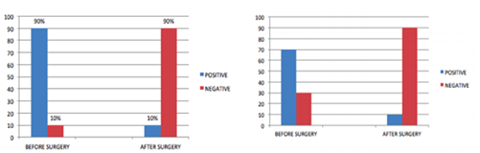
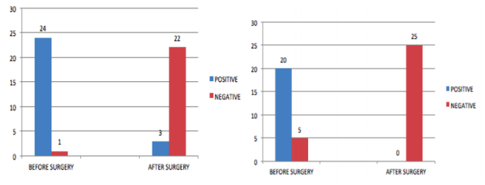
The articular stability test of Lachmann and Pivot-Shift in the pre and post-surgery time using the ST+IR graft in 20 patients were registered and shows the significant improvement in the stability after ACLR (Figure 7).
The same analysis with the mentioned tests with the use of ST graft only shows improvement in the stability too (Figure 8).
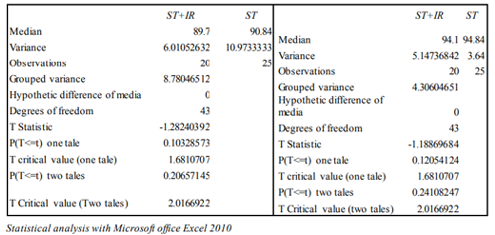
The 20 patients with ST+IR graft presents a median in the Lysholm test of 89.7 points with a standard deviation of 7.7 points and the 25 patients with ST graft obtain a median in Lysholm test of 90.84 points and a standard deviation of 7.7. Both Lyshom test were compared by Student T-test obtaining a p= 0.206, without significant differences between grafts, and in the Sf-36 test, the P was .241, without significant difference neither (Table 7).
In the Lysholm test, the results were grouped by range. The results under 65 points were considered poor, between 66 and 83 regular, from 84 to 94 good and over 95 excellent (See figure 9).
4. Discussion
This is the first study carried out in a Regional Naval Hospital about the functional results after anterior cruciate ligament reconstruction with isquiotibial grafts using the semitendinous and semitendinous and internal rectus. There exist many studies worldwide but none of them present a similar population, with Mexican military personnel with a high grade of physical activity. However, a bigger sample and follow up for better and significant results are mandatory.
In this study, we did not find significant differences in the use of one or other graft, although the internal rectus preservation can increase the time to recovery and preadaptation of the patients. According to other studies about the same topic but in different populations, the results are very similar to the presented in this study.
Actually, the gold standard in lesions of the ACL is the surgical reconstruction with plasty or graft[20]. The selection of graft type must be individualized according to the advantages of each one, surgeon experience and patients preference after discussion of pros and cons. The ideal graft is the one who mimics the anatomy and ACL properties, capable to support the needed pressure, follow the anatomic path, guarantee an initial safe fixation and integration[2]. There is no significant clinical differences between autograft or allograft; however, the allograft with sterilization techniques with radiation could present high failure indexes[21].
The complete treatment included rehabilitation for the adequate mobility and normal strength in the knee joint, the critical step is the fast recovery of the complete extension[7].
The complications after ACL reconstruction are divided in the directly related to the surgical procedure and the medical ones. The surgical complications include: infection (0.14% to 5.7% ), articular rigidity (4% to 35%), graft failure and osteoarthritis (50 to 70 %). The most frequent medical complications are the Deep venous thrombosis and pulmonary embolism[12,22,24].
In consequence, the preservation of muscular strength of isquiotibial muscles is particularly important in sportsman and sportswoman with ACL injury. Gobbi, A et al. [39]presents a work questioning the necessity of using the internal rectus in the isquiotibial reconstruction, showing good functional results with the use of semitendinous only and similar results in patients using semitendinous and internal rectus for ACL reconstruction.
Considering the literature about the use of the mentioned grafts and the similar functional results we found that both techniques offer excellent results for the patients. It must be considered that the use of semitendinous only in the triple band we can diminish the associated morbidity in the donor site, with less affection in the strength and flexion grades that with the use of semitendinous plus internal rectus.
With the analyzed data from military patients and rightful owners of the HOSNAVTLAN, we confirm that the rupture of ACL is more frequent in men than women with a relation of 6.5:1, with the IM service being the one with greater incidence of this pathology with a relation of 7:15, the median age was 30.9 +/- 8.5 years, and the meniscal associated injury was present in 67% of the cases, and from the total of those injuries 48% were in IM service. Those associations are related to the population in the study, the intense and constant physical activity.
The good functionality of this kind of grafts with the functional test was confirmed, with Lachman test negative in 89% of patients for both grafts and negative Pivot-shift test in 95%. With the functional test of Lysholm with 90.27 points in average, the initial hypothesis was accepted, with an adequate articular and functional recovery independent of the use of ST or ST+IR.
5. Conclusion
We could identify with this study a risk group in the MI service, where the preventive medicine could be a good option to reduce the incidence of this injury in the military personnel. With the actual tendency to better surgical techniques, fast and functional recovery after surgery reduced damage and comorbidity, the present study suggests that the use of ST graft only is a better option than ST+IR to diminish the donor site comorbidity with less grade of flexion, increased post-surgical pain and longtime of recovery.
Advice
From this paper we can continue the research in multiple fields like the risk factors conditioning the ACL rupture in the MI personnel, to implement preventive measures for the ACL rupture and meniscal injury, and the economic impact of this diseases comparing the use of isquiotibial graft and other grafts.
Ethical Cons Iderations
According to NOM-012-SSA3-2012, “that establish the criteria for the execution of research projects in human beings", this is a research protocol for human health, observational, comparative, transversal, retrospective, comparing the functional results of 2 different surgical techniques, both extensively described in the literature with good results. The nature of this study does not place the patient integrity in any risk and only the functional results are analyzed and compared with the hospital files.
References
- Sutton KM, Bullock JM. Anterior cruciate ligament rupture: differences between males and females. J Am Acad Orthop Surg. 2013 Ene 21; (1):41-50.
- Garín D, Reyes E, Penagos A. Lesión del ligamento cruzado anterior; Opciones actuales de tratamiento en el deportista. Orthotips. Abr-Jun 2016; (12): 2.
- Malheiros MV, Silviera, Cury. Anterior cruciate ligament –updating article. Rev Bras Ortop. 2016; 5 1(4):385–395.
- Irarrázaval S, Marcio A, Chao T, et al. Arthroscopic, and Radiographic Anatomies of the Anterior Cruciate Ligament. Elsevier Clin Sports Med 36. 2017: 9-23.
- Ayala J, García G, Alcocer E. Lesiones del ligamento cruzado anterior, Acta Ortopédica Mexicana. 2014 Ene-Feb; 28(1): 57-67.
- Forriol F, Maestro A, Vaquero MJ. El Ligamento cruzado anterior: morfología y función, trauma, Fundacion MAPFRE, Trauma Fund MAPFRE. 2008; (19): 17-18.
- Akihiko H, Shuhei O, Chantal P, et al. Anterior Cruciate Ligament Changes in Human Joint in Aging and Osteoarthritis, National Institutes of Health, Arthritis Rheum. 2012 Mar; 64(3): 696–704.
- Nessler T, Denney L, Sampley J. Injury Prevention: What Does Research Tell Us? Springer Science+Business Media, LLC. 2017.
- Kaeding c, Léger-St-Jean B, Magnussen R, Epidemiology and Diagnosis of Anterior Cruciate Ligament Injuries, Elsevier. Clin Sports Med 36. 2017: 1–8.
- Sulaiman A, Sukeik M, Ibrahim M. Management of anterior cruciate ligament injury: pathophysiology and treatment, British Journal of Hospital Medicine, Apr 2016; (77), 4: 222-225.
- LaBella C, Hennrikus W, Hewett T. Anterior Cruciate Ligament Injuries: Diagnosis, Treatment, and Prevention, AMERICAN ACADEMY OF PEDIATRICS, PEDIATRICS. May 2014; (133), 5.
- Márquez W, Márquez J, Gómez C. ¿Qué ocurre con las lesiones del ligamento cruzado anterior, su tratamiento, la recuperación de la función y el desarrollo de osteoartritis a largo plazo? ¿Hay espacio para el tratamiento conservador? Revisión de conceptos actuales. Els evier España Rev Colomb Ortop Traumatol. 2017; 31(2):75-86.
- Márquez J, Márquez W. Lesiones del ligamento cruzado anterior de la rodilla. Revista médica Universidad de Antioquia. IATREIA. 2009 sep; (22), 3.
- Lustig S, Servien E, Parratte S, et al. Lesiones ligamentosas recientes de la rodilla del adulto. EMC Aparato locomotor 2013; 46 (2): 1-19.
- Delgado M. Cirugía Ortopédica y Traumatología. 3ª edición. Editorial médica Panamericana. Mar 2015; 616-621.
- Álvarez A, García Y, Lesiones del ligamento cruzado anterior, Archivo Médico de Camagüey, Rev. Arch Med Camagüey. 2015; (19): 1.
- Eshuis R, Wilhelmus G, Tegner Y. Translation and Cross -cultural Adaption of the Lysholm Score and Teg, Journal of Orthopaedic & Sports Physical Therapy. 2016; 1-2.
- Forriol F, Ripoll PL, La reparación del ligamento cruzado anterior: solución de un problema histórico en el siglo XX. Trauma, fundación MAPFRE. Trauma Fund MAPFRE. 2012; (23):29-47.
- Bolívar V, Raya A, Garrido J. Lesiones del ligamento cruzado anterior. Nuevas opciones de tratamiento mediante ingeniería de tejidos. actualidad médica. Actual. Med. 2014; 99: (793): 157-161.
- Murawski C, Van Eck C, Irrgang J. Operative Treatment of Primary Anterior Cruciate Ligament Rupture in Adults. THE JOURNAL OF BONE AND JOINT SURGERY. J Bone Joint Surg Am. 2014; (96): 685-94.
- Duncan M, Poldervaart M, Ron L, et al. Guideline on anterior cruciate ligament injury a multidisciplinary review by the Dutch Orthopaedic Association; Acta Orthopaedic. 2012; 83 (4): 379-386.
- Archibald JD, Baer GS. Complications of anterior cruciate ligament reconstruction. En: Scott WN. Insall & Scott Surgery of the Knee. 5 the ed. Philadelphia: Elsevier; 2012; 428-34.
- Wilk K, Arrigo CA. Rehabilitation Principles of the Anterior Cruciate Ligament Reconstructed Knee. Twelve Steps for Successful Progression and Return to Play. Elsevier. Clin Sports Med 36. 2017; 189–232.
- Maletis G, Inacio, Reynolds Sarah. The incidence of Postoperative Anterior Cruciate Ligament Reconstruction Infections: Graft Choice Makes a Difference, Am J Sports Med. 2013 (41): 1780.
- Alanís LM, Zamora P, Cruz A; Ruptura de ligamento cruzado anterior en mujeres deportistas, An Med. Mex. 2012; 57(2): 93-97.
- Johnson DL, Harner CD, Maday MG, et al. Knee Surgery. Baltimore, MD: Williams and Wilkins; 1994: 877-895.
- Brown CH, Carson EW. Revision anterior cruciate ligament surgery. Clin Sports Med. 1999; 18:109-171.
- Mendoza P, Rodríguez J, Gutiérrez C, et al. Percepción funcional de los pacientes tras reconstrucción del ligamento cruzado anterior. Serie de casos. Revista Colombiana de Ortopedia y Traumatología. Rev Colomb Ortop Traumatol. 2017; 31(1):16-21.
- Akihiko H, Shuhei O, Chantal P, et al. Anterior Cruciate Ligament Changes in Human Joint In Aging And Osteoarthritis. National Institute of Health. Arthritis Rheum. 2012 Mar; 64(3): 696-704.
- Tashiro T, Kurosawa H, Kawakami A Et al. Influence of Medial hamstring tendon harvest on knee flexor strength after anterior cruciate ligament reconstruction: A detailed evaluation with a comparison of single and double tendon harvest. Am J Sports Med. 2003; (31): 522-529.
- Schwingler P. AANA, 2012.
- Mariscalco M, Flanigan D, et al. The influence of hamstring autograft size on patient-reported outcomes and risk or revision after anterior cruciate ligament reconstruction: A multicenter orthopedic outcomes network (MOON) cohort study. Arthroscopy. Dic 2013; (12) 29.
- Noyes FR, Butler DL, Grood ES, et al. Biomechanical analysis of human ligaments grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am. 1984; (66): 344-352.
- Linden M, Jered L, Sernert N, et al. Patellar Tendon or semitendinosus Autografts for Anterior Cruciate Ligament Reconstruction. AJSM. May 2007; (35) 740-748.
- Freeman KB, D'Amato MJ, Nedeff DD, et al. Arthroscopic anterior cruciate ligament econstruction: A meta-analysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003; (31): 2-11.
- Draganich L, Jaeger R, Kralj A: Coactivation of the hamstrings and quadriceps during extension of the knee. J Bone Joint Surg. 1989; (71) :1075-1081
- Liu W, Maitland M. The effect of hamstring compensation for anterior laxity in the ACLdeficient knee during gait. J Biomech. 2000; (33): 871-879.
- More R, Karras B, Neiman R et al, An anterior cruciate ligament protagonist. An in vitro study. Am J Sports Med. 1993; (21): 231-237.
- Gobbi A, Domzalski M, Pascual, J et al. Anterior Cruciate Ligament Reconstruction: Is It Necessary to Sacrifice the Gracilis.Arthroscopy. Mar 2005; 275-280.
- Zelle, B.A. Herzka, A.S. Harner, C. Evaluation of clinical outcomes in anterior cruciate ligament surgery. Oper Tech Orthop 2005; 15:76-84.
- Haim A, Pritsch T, Yosepov L, Arbel R. Anterior cruciate ligament injuries. Harefuah 2006 Mar; 145(3):208-14, 244-5.
- Irrgang JJ, Ho H, Harner CD, Fu FH. Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligamentreconstruction. Knee Surg.Sports
- Furman W, Marshall JL, Girgis FG. The anterior cruciate ligament. A functional analysis based on postmortem studies. J.Bone Joint Surg.Am. 1976 Mar; 58(2):179-185.
- Hashemi J, Chandrashekar N, Mansouri H, Slauterbeck JR, Hardy DM. The human anterior cruciate ligament: sex differences in ultrastructure and correlation with biomechanical properties. J.Orthop.Res. 2008 Jul; 26(7):945-950.
- Siebold R, Ellert T, Metz S, Metz J. Femoral insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: morphometry and arthroscopic orientation models for double-bundle bone tunnel placement--a cadaver study. Arthroscopy 2008 May; 24(5):585-592.
- Zimny ML. Mechanoreceptors in articular tissues. Am.J.Anat. 1988 May; 182(1):16-32. 124
- Amir G, Lowe J, Finsterbush A. Histomorphometric analysis of innervation of the anterior cruciate ligament in osteoarthritis. J.Orthop.Res. 1995 Jan; 13(1):78-82.
- Zantop T, Petersen W, Sekiya JK, Musahl V,Fu FH. Anterior cruciate ligament anatomy and function relating to anatomical reconstruction. Knee Surg.Sports Traumatol.Arthrosc. 2006 Oct; 14(10):982-992.
- Kennedy JC, Weinberg HW, Wilson AS. The anatomy and function of the anterior cruciate ligament. As determined by clinical and morphological studies. J.Bone Joint Surg.Am. 1974 Mar; 56(2):223-235.
- Noyes FR, DeLucas JL, Torvik PJ. Biomechanics of anterior cruciate ligament failure: an analysis of strain-rate sensitivity and mechanisms of failure in primates. J.Bone Joint Surg.Am. 1974 Mar; 56(2):236-253.