Information
Journal Policies
Unpleasant Memories Related to Autobiographical Memory in Chronic Pain Patients
Karen dos Santos Ferreira1*, Camila Rimoldi Kameoka2, Guilherme Henrique Rosseto Nakamite2, Giovana Marino Saran2, Maria Paula Foss3
2.Neurology Clinic, Medical School, University Center Barao de Maua, Ribeirao Preto, Sao Paulo, Brazil.
3.Psychology, University Hospital, Medical School of Ribeirao Preto, University of Sao Paulo, Brazil.
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Purpose/ Aim of the study: The objective of the present study is to analyze the aspects related to autobiographical memory in patients with chronic pain compared to a control group. In addition, an attempt was made to assess the variables that might influence autobiographical memory.
Materials and Methods: This was a case-control study conducted on patients with chronic pain and controls with no pain. Subjects included 29 patients with chronic pain and 29 control patients. Demographic data, clinical data related to pain, as intensity and use of analgesics, comorbidities, as depressive disorder and anxiety disorder, were assessed. Neuropsychological evaluation included the Montreal Cognitive Assessment and the Autobiographical Memory Test, Brazilian version.
Results: The main type of pain was lower back pain (31.0%), the mean current frequency of pain was 22.3 + 10.8 days/month, and mean pain intensity was 8.1 + 1.6. Quantitative analysis did not differ significantly in the Montreal Cognitive assessment (22.5 versus 23.7; p = 0.18), Autobiographical Memory Test words remembering (30.2 versus 31.8; p = 0.58) and the latency time to respond (115.8 s versus 114.6 s ; p = 0.42). Qualitative analysis of memories evoked by neutral words revealed that chronic pain patients had more memories of negative content. These findings were not influenced by comorbidities.
Conclusions: The present results show that patients with chronic pain have changes in autobiographical memory compared to a control group, more specifically related to memory content (unpleasant memories) than to memory extension or latency time to assess memories.
Chronic pain, Cognitive dysfunction, Comorbidities,Psychiatry
Painful syndromes continue to be a great challenge today, including various aspects such as intensity and associated manifestations, as well as subjective and multidimensional factors. [1-3] The prevalence of chronic pain defined for the general population by the World Health Organization (WHO) ranges around 37% in developed countries and 41% in developing countries[4].
Chronic pain is a subject of research interest because it generates physical and emotional stress for the patients and their caregivers, as well as financial and social losses for the population, including the treatment of pain and worker benefits due to physical disability[3-5].
Patients with chronic pain frequently report cognitive complaints that cause difficulties in social situations and in daily life activities. Despite the considerable heterogeneity of the studies reviewed, there was a consistently significant result showing a better performance by healthy controls compared to patients with chronic pain in cognitive tests.[6-9] A 2013 meta- analysis study systematically assessed the literature about working memory function in persons with chronic pain. This result can be explained by the network of activated brain areas in patients with chronic pain defined as pain matrix. Curiously, these brain areas include structures of the limbic system that are also involved in memory retention and fixation[8].
More recently, two studies have assessed another cognitive strand in patients with chronic pain, i.e., autobiographical memory. This type of memory involves the memories of an individual about his own past at various levels of complexity, ranging from more generalized memories to specific life situations. These studies observed that the presence of pain resulted in loss of memory of autobiographical events in the life of an individual from both a qualitative and quantitative viewpoint[10,11].
The hypothesis raised is that pain, as a complex and disagreeable emotional phenomenon, may prevent the access to more extensive memories related to previous experience and also to pleasant memories, and may also facilitate the memory of negative events, as unpleasant memories[10,11].
Since mood disorders such as depressive and anxiety disorders may influence aspects related to memory and cognition[12], these factors should be analyzed jointly in a study model aiming to assess the neuropsychological performance of patients with chronic pain. In addition, the medications used for the treatment of chronic pain and comorbidities may also affect the cognitive performance and should also be analyzed[13].
Indeed, new aspects related to cognitive deficits of patients with chronic pain are being studied, indicating that new investigations should be devoted to such clinically relevant area. Thus, the objective of the present study was to describe and analyze the functioning of autobiographical memory in patients with chronic pain compared to control patients with no pain matched for sex, age and educational level. In parallel, the main factors that influence the cognitive disorders affecting the population with chronic pain were also assessed, as well as depressive and anxiety symptoms, use of medications and other comorbidities.
2. Methods
This was a case-control study. Patients were recruited at a University Hospital for a period of six months. Patients aged 18 to 60 years with non-oncologic chronic pain (lasting for more than 3 months)[14] , who agreed to give informed written consent were included in the study. They were recruited in the waiting rooms of the outpatient clinics of various specialties (orthopedics, neurology, internal medicine) by answering the question: “Throughout our lives, most of us have had pain from time to time (such as minor headaches, sprains and toothaches). Have you had pain, other than these everyday kinds of pain, in the last three months?”. The exclusion criteria were the presence of mental changes that would prevent the response to a questionnaire and illiteracy.
1) Demographic data such as age, sex, marital status, and profession.
2) A semi-structured questionnaire based on the Brief Pain Inventory 17 was applied to the patients with chronic pain. Clinical data regarding acute pain symptoms, location and characteristics of the pain, pain intensity (numeric pain scale), use of analgesic were obtained.
3) Comorbidities such as depressive disorder and anxiety disorder (Diagnostic and Statistical Manual of Mental Disorders 5 - DSM 5)18, sleep aspects (“Do you have any kind of sleep problems such as insomnia, unrefreshed sleep or sleep apnea?”), alcohol abuse (“How many doses of alcohol do you drink weekly?), history of head trauma
(“Have you ever had any kind of head trauma?”) and other comorbidities that were previously diagnosed by other clinicians such as thyroid dysfunction, diabetes and hypertension.
4) Use of medication.
5) Neuropsychological evaluation by the Montreal Cognitive Assessment (MoCA) test and the Autobiographical Memory test, Brazilian version[15].
Healthy patients matched for sex, age and educational level were recruited as controls.. The study was approved by the Ethics Committee of the University Center Barão de Mauá (CAAE 54917816.7.0000.5378).
The AMT consists of the presentation of a series of stimulus-words of different emotional valences (positive, negative and neutral), with the participant being asked to retrieve specific memories of his life history related to these words. The positive words used were Praise, Pleasant, Fun, Animated, and Honest, the negative words were Tragic, Unhappy, Misery, Angry, Disappointed, and the neutral words were Infantile, Moderate, New, Occasion, Rapid.
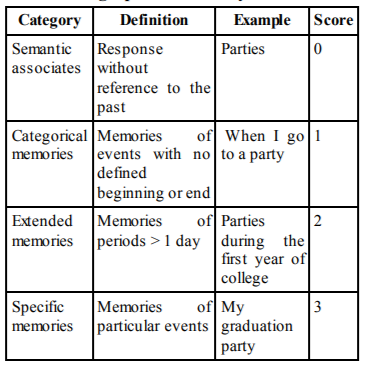
Taken together, latency time to a response and the results related to the specificity of the memories described represent the result of assessment.15 (see table below). The Brazilian version of the AMT can be used in research on populations of low socioeconomic and educational level and has been used in Brazil in investigations related to dementia.16
In this study, interviews related to the application of the Autobiographical Memory test were recorded and later analyzed by two blind evaluators (a neurologist and a neuropsychologist), who did not know who were patients with pain and control patients, to establish quantitative scores and qualitative data analysis.
3. Statis Tical Analys Is
Data were analyzed statistically using the SPSS software version 18.0.19 Categorical variables were analyzed by the X2 test or Fisher exact test according to the expected frequency in the cells. Quantitative variables were analyzed by the Kolmogorov-Smirnov test in order to define their type of distribution. Data with normal distribution were analyzed by analysis of variance (ANOVA) and data with non-normal distribution were analyzed by the nonparametric Mann-Whitney test. A linear regression model was used to correlate quantitative dependent variables controlled by independent variables, and a binary logistic regression model was used to correlate dependent categorical variables controlled by independent variables.
4. Results
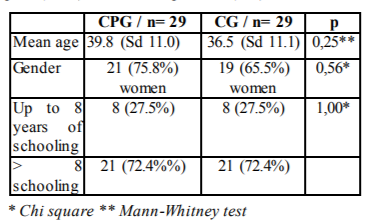
Seventy patients were selected for the study. Two controls were excluded due to the presence of mental changes that prevented them from answering the questions and ten patients were excluded because they did not complete the interview. Finally, 29 patients with chronic pain (CPG) and 29 control patients (CG) were included in the study. The two groups did not differ in terms of age, educational level or gender (Table 1).
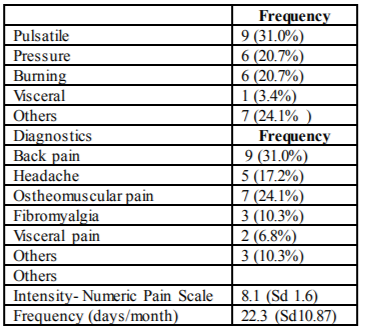
The main types of pain, frequency and the mean intensity of pain according to the Numeric Pain Scale were described in Table 2.
Regarding medication, 3 patients with pain (10.3%) used amitryptiline, 2 (6.8%) used other antidepressants, 1 (3.4%) used topiramate, 1 (3.4%) used gabapentin, and one (3.4%) used clonazepan. The analgesics more frequently used were dipyrone (16, 44.4%) and non-hormonal anti-inflammatory (6, 22,2%). The medications more frequently used by the controls were antidepressants (3, 10.3%) and clonazepan (1, 3.4%).
The comorbidities more frequently detected in CPG patients were generalized anxiety disorder (12, 41.4%), major depressive disorder (6, 20.7%), non-restoring sleep (10, 34.5%), hypertension (4, 13.8 %), diabetes mellitus (3, 10.3 %), and hypothyroidism (2, 6.8 %).
The comorbidities more frequently detected in CG patients were generalized anxiety disorder (10, 34.5%), non-restoring sleep (3, 10.3%), major depressive disorder (3, 10.3%), hypertension (1, 3.4 %), and hypothyroidism (1, 3.4%).
Patients with chronic pain did not show higher rates of anxiety disorder (p= 0.78) or depressive disorder (p= 0.47).
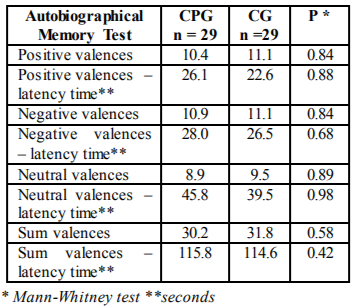
Quantitative assessment results of the neuropsychological tests applied revealed no differences in scores for chronic pain group, comparing to a control group, in the MoCa Test (22.5 versus 23.7; p = 0.18), remembering autobiographical memories - positive, negative and neutral emotional valences and in the latency time in responding questions - positive, negative and neutral emotional valences (see scores in Table 3).
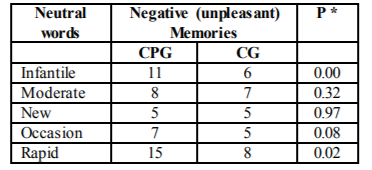
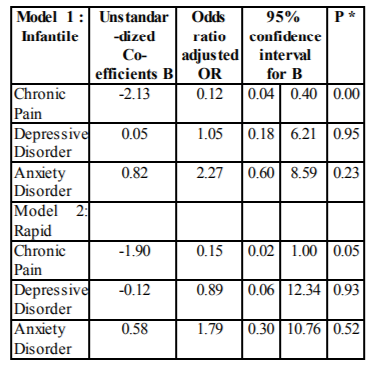
Regarding the qualitative assessment of neuropsychological tests applied, when we evaluated the memories evoked by neutral words, we observed that CPG patients had a distorted view of remembered memories, with a larger number of memories with a negative content (unpleasant memories) than CG patients for the words “Infantile” and “Rapid” (Table 4). To assess the content of memories (negative or not) evoked by the words “Infantile” and “Rapid” controlled for the independent variables chronic pain, depressive disorder and anxiety disorder, we used a binary logistic regression model (Tables 5). Chronic pain was an independent factor for the results obtained.
5. Discussion
The present study described and analyzed cognitive aspects related to autobiographical memory in patients with chronic pain and in controls with no pain paired for sex, age and educational level, in addition to assessing the main factors triggering the cognitive disorders observed such as depressive disorder and anxiety disorder.
Cognition and chronic pain represent a topic currently under study and the possible reasons for cognitive deficits include the presence of depressive symptoms (which are detected in 40 to 58% of patients with chronic pain) and the use of medications.[20] However, other studies have reported that chronic pain may be an independent factor for cognitive deficits[9].
Within this context, according to previous studies [10,11], autobiographical memory may also be influenced by the presence of chronic pain. It has been reported that patients with chronic pain may have a lower memory index for autobiographical events, as well as a longer latency time to start remembering these events. Another aspect studied is the distortion of these remembered memories in patients with chronic pain, who tend to remember more events with a negative emotional valence.
In the present study, we observed that a group of patients with chronic pain showed worse absolute scores than a control group in the autobiographical memory test, and a longer latency time to respond to all emotional valences (positive, negative and neutral). However, as also reported by others,[11] the results obtained were not statistically significant. The first possible justification of these findings could be that the small number of patients studied was insufficient to detect the expected results. In addition, similar results were obtained with the MOCA test, although in larger groups of patients differences between patients with chronic pain and controls with no pain have been previously reported by our group[9].
A second possibility is that control patients may also perform poorly in these types of tests with an abstract content since their educational level is also low, especially in our country. Since there are very wide variations in performance in this type of test, which is extremely subjective, and the low educational level in developing countries may influence the results, our findings may differ from the studies published in developed countries on samples of better socioeconomic and cultural level.
Regarding qualitative memory assessment, we detected a larger number of memories of negative content (unpleasant memories) when evoked by neutral words in patients with chronic pain, regardless of the presence of anxiety or depressive disorder. This finding demonstrates a distortion of described memories in patients with chronic pain, as also reported in a previous study[10]. This distortion of memories may be related to pain catastrophizing which is one of the stronger psychological predictors of the description of pain by the patients.[21]. In patients with chronic pain, "catastrophization" is defined as an exaggerated negative cognitive-affective orientation in relation to pain. Some studies have also detected a lower performance in neuropsychological tests associated with greater pain intensity and catastrophization[22].
Regarding the clinical implications of these findings, there is evidence of moderate and high quality using cognitive-behavioral therapy, multimodal treatment and mindfulness-based stress reduction for an improvement of catastrophizing symptoms, besides increasing patient self-efficacy for managing pain and pain acceptance.21;23 On this basis, it would be interesting to define a battery of tests that might identify the patients with these symptoms and refer them to proper treatment.
Thus, although the present study was a small one, we consider the demonstration of these findings to be pertinent for several reasons. First of all, no previous study has been conducted in Brazil to analyze autobiographical memory in patients with chronic pain. Secondly, there is the possibility to treat the symptoms of these patients, with a possible reduction of suffering and an improvement of the quality of life of these patients.
We may also suggest to other investigators to repeat these studies on a larger number of patients for a better definition of the quantitative analysis of the memories reported. In any case, the model of neurocognitive changes associated with chronic pain is still far from being fully understood.
In conclusion, the results lead us to believe that patients with chronic pain have cognitive changes related to autobiographical memory. These changes are more related to evoked memory content (unpleasant memories) than to memory extension (quantitative description) or latency time to evocation.
References
- Warfield CA, Bajwa ZH. Principles and Practice of Pain Medicine. Second edition, The McGraw-Hill, 2004
- Merskey H, Bogduk N. Classification of Chronic Pain: Description of Chronic Pain Syndromes and Definition of Pain Terms. IASP Press, WA, USA (1994).
- Shotter EF. Dame Cicely Saunders J Med Ethics 2006. 32: 309.
- Andersson HI, Ejlertsson G, Leden I, Rosenberg C. Chronic pain geographically defined general population: studies of differences in age, gender, social class, and pain localization. Clin J Pain, 1993. 9 (3): 174-82.
- Teixeira MJ, Marcon RM, Rocha RO, Figueiró JAB. Epidemiologia clinica da dor. Rev Med, 1999. 78 (2): 36-52.
- Apkarian A, Hashmi J, Baliki M. Pain and the brain: specificity and plasticity of the brain in clinical chronic pain. Pain 2011. 152: S49–64.
- Legrain V, Van Damme S, Eccleston C, et al. A neurocognitive model of attention to pain: behavioral and neuroimaging evidence. Pain, 2009. 144: 230–2.
- Berryman C, Stanton TR, Bowering KJ, et al. Evidence for working memory deficits in chronic pain: A systematic review and meta-analysis. Pain, 2013. 154: 1181–1196.
- Ferreira KS, Oliver GZ, Thomaz DC, Teixeira CT, Foss MP. Cognitive deficits in chronic pain patients, in a brief screening test, are independent of comorbidities and medication use. Arquivos de Neuro-Psiquiatria 2016.
- Meyer P, Karl A, Flor H. Pain can produce systematic distortions of autobiographical memory. Pain Medicine 2015; 16: 905-910.
- Liu X, Liu Y, Li L, et al. Overgeneral Autobiographical Memory in patients with chronic pain. Pain Medicine 2014; 15: 432-439.
- Hae Jin Ko, Se Jung Seo, Chang Ho Youn, et al. The Association between Pain and Depression, Anxiety, and Cognitive Function among advanced Cancer Patients in the Hospice ward. Korean J Fam Med. 2013. 34: 347-356.
- Andrade DC, Rodrigues CL, Abraham R, Castro LHM, Livramento JA, Machado LR, Leite CC, Caramelli P. Cognitive impairment and dementia in neurocysticercosis: a cross - sectional controlled study. Neurology, 2010. 74: 1288-95.
- Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R et al. A classification of chronic pain for ICD-11. Pain. 2015. 156 (6): 1003-7.
- Pergher GK, Stein LM. Recuperando memórias autobiográficas : avaliação da versão brasileira do Teste de Memória Autobiográfica. Psico 2008; 39 (3): 299-307
- Lemos C, Hazin I, Falcão JTR. Investigação da memória autobiográfica em idosos com Demência de Alzheimer nas fases leve e moderada. Estudos de Psicologia 2012. 17 (1): 135- 144.
- Toledo FO, Barros PS, Herdman M, et al. Cross-cultural Adaptation and Validation of the Brazilian Version of the Wisconsin Brief Pain Questionnaire. J Pain Symptom Manage, 2013. 46 (1): 121-30
- American Psychiatry Association. Diagnostic and statistical manual of mental disorders – DSM - 5. 5th ed. Washington: American Psychiatric Association, 2013.
- SAS/ STAT User´s Guide, Version 8, Cary, NC: SAS Institute Inc., 1999. R version 2.8.0 copyright © 2008. the r foundation for statistical computing.
- Landro NI, Fors EA, Vapenstad LL, et al. The extent of neurocognitive dysfunction in a multidisciplinary pain centre population. Is there a relation between reported and tested neuropsychological functioning? Pain, 2013.154: 972–977.
- Schutze R, Rees C, Smith A, et al. How can we best reduce pain catastrophizing in adults with chronic non-cancer pain? A systematic review and meta-analysis. JPain, 2017. S1526 - 5900(17) 30752-6.
- Baker KS, Gibson SJ, Georgiou-Karistianis N, Giumarra MJ. Relationship between self-reported cognitive difficulties, objective neuropsychological test performance and psychological distress in chronic pain. Eur J Pain, 2017, doi: 10.1002/ejp.1151.
- Turner JA, Anderson ML, Balderson BH, et al. Mindfulness -based stress reduction and cognitive behavioral therapy for chronic low back pain: similar effects on mindfulness, catastrophizing, self-efficacy, and acceptance in a randomized controlled trial. Pain 2016, 157(11): 2434-2444.