Information
Journal Policies
The Association between Mild Traumatic Brain Injury (mTBI) and Attention Deficit Hyperactivity Disorder (ADHD) Among Egyptian Adolescent Athletes
Jessica Uno MD.MA1,Lenard A.Adler MD2,Samuel Alperin MD3,Heba Hedaway MD4,Samir Abul Magd MD5,David A.Baron DO. MSEd6*
2.Departments of Psychiatry and Child and Adolescent Psychiatry, New York University, New York.
3.Cincinnati Children's Hospital Medical Center, Cincinnati, Ohio, and Hofstra NS-LIJ School of Medicine,Hempstead, New York.
4.Ain Shaums University, Cairo, Egypt.
5.Cairo University, Cairo, Egypt.
6.Keck School of Medicine of USC, Los Angeles, California.
Copyright :© 2017 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
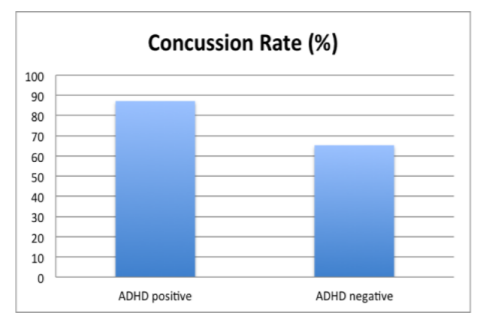
Mild traumatic brain injury (mTBI), or concussion, is highly prevalent among adolescent athletes in the United States. In characterizing the modifiers, risk factors, and persistent sequelae of mTBI, attention deficit hyperactivity disorder (ADHD) has been found to be strongly associated with mTBI in young athletes. This retrospective observational study examined the association between mTBI and ADHD using a blinded survey study in an international sample of 450 Egyptian adolescent athletes ages 14-19 years old. There was a significant association between ADHD and mild TBI (x2 (1) = 7.94. p= 0.005). In ADHD-positive subjects, 87.2% reported a history of mTBI, while a lower rate of 65.0% was reported in ADHD-negative subjects. ADHD was present in 11.3% of the subjects with mTBI and at a lower rate of 3.4% in the subjects without mTBI. These findings were similar to those from the United States and further highlight the urgency of understanding the relationship between ADHD and mTBI worldwide.
1.Introduction And Background
Mild traumatic brain injury (mTBI), also known as a “concussion,” is a prominent and common sports-related injury, as well as a growing public health concern among athletes worldwide. An estimated 1.3 to 3.8 million cases occurs annually in the United States.[1] “Mild” traumatic brain injury is distinguished from moderate and severe traumatic brain injury (TBI) based on the limited duration or presence of loss of consciousness, as defined by the Centers for Disease Control. No abnormality is usually detected on standard structural neuroimaging, and acute clinical symptoms are not localizable to a structural injury or brain lesion.[2] According to the 2012 Zurich International Conference in Sport Consensus Statement, the mechanism of mTBI results from impulsive transmitted forces that cause shearing, tearing, or stretching of brain tissue. Such forces include sudden acceleration, deceleration, or rotational forces that accompany rapid turning of the head and neck. Notably, concussion rarely involves loss of consciousness and does not require a direct blow to the head.[3]
Yet, mTBI can cause significant short-term and long-term disability, often characterized by persistent difficulties with attention, concentration, emotional dysfunction, and other neurocognitive deficits.[4] Symptoms can be divided among somatic, cognitive, and affective categories.[5] Risk of repeat head injury is high; athletes with a prior concussion history are up to three times more likely to suffer a subsequent concussion than those with no previous history.[6] Despite these dangers, mTBI remains an under-recognized and under-reported phenomenon. In the context of athletics, large discrepancies exist in the ways that return-to-play guidelines are applied across different levels of sports team representation. As highlighted by Rivara et al., an unfortunate trend in sporting culture over the past fifty years has underestimated the gravity and implications of mTBI in athletics (2014). Archaic ideas about simply “shaking off” the disorientation caused by a concussion, or pressure for team players to resume sports participation in time for competitions, can all hinder the road to recovery. For this reason, it becomes imperative to identify high-risk patients for mTBI and educate clinicians, sports coaches, and parents about concussion prevention, diagnosis, and management.
One condition strongly associated with mTBI is attention deficit hyperactivity disorder (ADHD). ADHD’s prevalence among the athletic population is similar to that of the general American population, affecting approximately 10% of adolescents under the age of 18 and 5% of adults.[7] mTBI has been associated with ADHD in several ways: either as a risk factor for development of secondary ADHD or as a consequence of the increased risk taking and accidents associated with ADHD.[8] While precise temporality is disputed, the latter hypothesis is supported by the fact that ADHD is known to increase the risk of injuries and accidents experienced by patients in general.[9] A 2014 study by Chou et al. demonstrated that adolescents with ADHD had a 1.3-fold greater incidence of extremity bone fractures than adolescents without ADHD.[10] The incidence of traumatic impact and accidents leading to extremity fractures would also convey on ADHD patients higher risk for traumatic brain injury, even in the absence of direct head trauma.
To date, the relationship between mild repetitive traumatic brain injury and ADHD has been poorly studied. Data on major TBI exists, but offers little insight into the effects and relationship with ADHD. Additionally, most of the literature on mTBI and ADHD has examined relatively small samples of US and European young adult or college-age males, such as Iverson et al.’s examination of 139 NCAA Division-I athletes (2014). Given that the global prevalence of ADHD is estimated to be 5.3-7% in adolescents and 3.4% in adults, we wanted to study an international sample consisting of pediatric patients.[11] [12] [13] Therefore, the objective of this project was to examine the rates of co-occurrence of ADHD diagnoses and mTBI history in a large sample of Egyptian male and female adolescent athletes.
2. Methods
This retrospective observational study was an Institutional Review Board (IRB) investigation surveying international pediatric athletes retrospectively about their recall of lifetime status of having or not having experienced mTBI in the context of athletic activities. The study protocol was approved by the local IRB at Aim Shaums University in Cairo, Egypt. Study participants were recruited from competitive representative, club sports or school sports teams in Cairo. Represented sport activities included soccer, handball, basketball, and badminton. Over a four-year period, from 2011 through 2014, 450 Egyptian adolescent athletes were administered a blinded survey at Cairo University, Ain Shaums. Regarding sample characteristics, 84% of the sample was male (n=302) and 16% were female (n=74) (Table 1). The sample participants ranged in age from 14 to 19 years old. This was a retrospective study, and subjects were not followed.
ADHD diagnoses were made by experienced academic psychiatrists in Cairo. Diagnosis was established on the basis of the World Health Organization Adult ADHD Self-Report Scale v1.1 Symptom Checklist (ASRS), and by comprehensive psychiatric interview. The ASRS was developed in 2005 by the Workgroup on Adult ADHD, which included researchers from New York University and Harvard Medical Schools, in conjunction with the WHO Composite International Diagnostic Interview (CIDI). [14] It consists of 18 questions consistent with the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria addressing the manifestation of ADHD symptoms in adults.[15] The ASRS takes into account the importance of symptoms,impairments, and history for a correct diagnosis of ADHD. The ASRS criteria have been validated for adolescents, with ASRS demonstrating high internal consistency and high concurrent validity with the clinician-administered ADHD-RS in adolescents with ADHD.[16] Adolescents who did not meet ASRS criteria for a diagnosis of ADHD are hereinafter referred to as the “non-ADHD” group.
The diagnosis of mTBI was made by experienced sports psychiatrists in Cairo, Egypt, and included an interview based on the Sport Concussion Assessment Tool, 3rd edition (SCAT-3) criteria. The SCAT-3 is a standardized concussion diagnosis tool for evaluating athletes ages 13 years or older.[17] It includes a battery of questions and neurologic exam maneuvers designed for sideline assessment of sports injuries to the head. A positive history of mTBI was established on the basis of self-reported symptoms associated with concussion. These included episodes of changes in vision (sensitivity to light, blurry vision, vision issues), changes in balance (with or without nausea, vomiting, sensitivity to sound, ringing in ears), mental reaction (increased irritability, emotionality, sadness, anxiety, nervousness), sleep disturbances (difficulty falling asleep, drowsiness, increased or decreased sleep), dizziness, headache, or “off-canter” cognition (mental slowing, mental fog, difficulty concentrating, difficulty remembering, confusion about recent events, feeling dazed or stunned) for the 3 days immediately following any sports injury (Table 2).
Figure 1, “Sports injuries” could have occurred either during practice or competition, as well as outside of direct play but during activities related to preparing for or transitioning out of participation. For example, such an outside-of-play scenario could be slipping and falling in the locker room when a participant was changing into or out of their athletic uniform. The criteria for sports injury did not specify a blow to the head, consistent with the understood mechanism of concussive injury. Subjects were considered to have a history of mTBI if they were positive for three incidents.[18]
3. Results
There was a significant association between ADHD diagnosis and positive mTBI history, as determined by a chi-squared analysis (x2 (1) = 7.94. p = 0.005) (Table 3). Mild TBI occurred in 87.2% of the subjects with ADHD and at a lower rate of 65.0% in the subjects without ADHD (Figure 1). ADHD was present in 11.3% of the subjects with mTBI and at a lower rate of 3.4% in the subjects without mTBI. Rates were similar in males and females, although females were less represented in this sample.
4. Discussion
This examination revealed a significant association between ADHD and mTBI in this sample of Egyptian youth athletes. The association between ADHD and mTBI we found is a similar finding to the results of the meta-analysis by Adeyemo et al (2014). As shown in adolescents with ADHD sustained identifiable mTBI at a rate 22.2% higher than their non-ADHD peers. From another perspective, if we examine the total group of adolescents who sustained mTBIs, ADHD was present in 11.3% of the subjects. In the group of adolescents without mTBI, there was a much lower rate of 3.4% for ADHD.
Thus, this sample demonstrated that adolescents with ADHD had a rate of positive mTBI history close to 3.5 times that of non-ADHD adolescents. This rate corresponds with the findings of Nelson et al. 2015 study’s finding that American college athletes with ADHD were associated with 3 times the prevalence of mTBI.[19] Further, the rate of ADHD occurring in this international sample (8.7%) is similar to that documented in the United States.[20] It also is similar to the projected ADHD rate of ~7% worldwide, as mentioned in the introduction. Likely, this study’s sample population is representative of other international youth athlete samples that display similar rates of ADHD, and its findings could be replicated among those groups.
While it is difficult to approximate the global rate of sports-injury mTBIs, our findings point to the results demonstrated by American and European studies of ADHD and mTBI among athletes being an international phenomenon. Additionally, the age demographics of our study suggest that comorbid ADHD and mTBI is a global public health issue for child and adolescent athletes, in addition to college-age and professional athletes. The implications of our findings justify heightening the vigilance internationally among providers, coaches, teachers, and parents regarding mTBI incidents among their wards, child and adolescent athletes with ADHD.
As a premorbid condition, ADHD can greatly raise the stakes for patients who suffer mild traumatic brain injury, as the interaction of the two pathologies may contribute to complex long-term psychiatric complications of sports accidents. Scholars such as Faraone et al. have established that patients with childhood primary ADHD are high-risk for psychiatric comorbidity as they age (2015). The manifestation of subsequent psychiatric disorders among ADHD patients is an important dimension of ADHD’s etiologic heterogeneity. Because there are multiple genetic, epigenetic, and environmental determinants of ADHD and its presentation, adolescents with ADHD can have greater vulnerability to neuropsychiatric insult. In agreement with this premise are new studies showing that pediatric patients with ADHD suffer more severe mTBI symptoms and a prolonged recovery course compared to their non-ADHD peers.[21]
Separately, it has been shown by investigators such as Fann et al. (2004) that in adults, mild traumatic brain injury carries increased risk for psychiatric illness following mTBI. This pattern was seen both in subjects both without prior psychiatric illness AND with prior psychiatric illness.xxii Prior psychiatric illness significantly modified the relationship between TBI and subsequent psychiatric illness. Previous psychiatric conditions were also a significant predictor of subsequent psychiatric illness. Fann’s study included subjects ages 15 to 44 years old. Thus, as a premorbid psychiatric condition, ADHD may be associated with persistent psychiatric illness following mTBI.
Conversely, our study’s findings could be applied to improving international ADHD screening and diagnosis standards for adolescent patients. A 2014 study done by Ilie et al. in Canada found that adults with a history of traumatic brain injury had almost 2.5 times the odds of lifetime ADHD diagnosis and screening positive for current ADHD.[23] Therefore it may be useful for providers to assess mTBI history during screening and assessment of ADHD in the adolescent population. Incorporating mTBI history into accurate ADHD screening practices however would first require better differentiation between primary and secondary ADHD, as will be discussed in the next section.
5. Limitations And Future Directions
One caveat to these findings is the potential for selection bias, as the subjects were being specifically queried for the presence of mTBI. Secondly, evaluation of positive mTBI status relied heavily on self-report and subject recall of symptoms. This is a common limitation of mTBI studies in the continued absence of established biomarkers and other objective measures for concussion diagnosis. Symptom-based diagnosis of mTBI can be problematic because certain symptoms could be attributed to multiple causes, not exclusively mTBI. As discussed earlier, the ADHD population may have other psychiatric comorbidities whose presentation mimic mTBI. Regarding this issue of concussion diagnosis, attempts to characterize the relationship between mTBI and ADHD status would greatly benefit from the consolidation of a standardized definition of mTBI, locally and internationally.The American Neurologic Association acknowledged in 2013 that no such consensus existed.[24]
Another limitation of these findings is the small sample of female participants included, causing the lack of significant gender differences in ADHD and mTBI rates to be tentative. It has been widely established that ADHD predominantly presents in males, exhibiting a male-to-female sex ratio of 4:1 in clinical studies, 2.4:1 in populations studies.[25] However, this does not justify neglecting a thorough examination of any gender differences in ADHD and mTBI rates among female pediatric patients.
Finally, as was demonstrated of other studies in Adeyemo et al.’s 2014 meta-analysis, it was not possible to determine the temporal association between ADHD and mTBI in the current sample.[26] There is ongoing debate about the phenomenon of “secondary ADHD,” or the new onset of ADHD symptoms following mTBI. Secondary ADHD diagnoses in child and adolescent patients are suspect in the sense that evaluators cannot determine that patient would not have developed ADHD in the absence of mTBI. Some investigators hypothesize that patients presenting with seemingly secondary ADHD actually had primary ADHD that went undiagnosed until clinical work-up following concussion. Likely, mTBI exacerbates pre-existing attention and concentration deficits of patients with primary ADHD that was previously subthreshold for diagnostic criteria. Future directions include a prospective cohort study following youth with established ADHD diagnoses preceding any mTBI incidence in a large international sample with equal representation of both genders. Through such work, we hope to improve standard of care for ADHD patients across the lifespan.
References
- Adeyemo, B., Zafonte, R., Kagan, E., Uchida, M., Kenworthy, T., Spencer, A., & Faraone, S. (2014). Mild traumatic brain injury and ADHD: A systematic review of the literature and meta-analysis. Journal of Attention Disorders, 18(7), 576-584.
- Fann, J., Burington, B., Leonetti, A., Jaffe, K., Katon, W., & Thompson, R. (2004). Psychiatric Illness Following Traumatic Brain Injury In An Adult Health Maintenance Organization Population. Archives of General Psychiatry, 61(1), 53-61.
- McCrory P, Meeuwisse WH, Aubry M, et al (2012). Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med 2013; 47: 250–58.
- Radhakrishnan, R., Garakani, A., Gross, L. S., Goin, M. K., Pine, J., Slaby, A. E., Baron, D. A. (2016). Neuropsychiatric aspects of concussion. The Lancet Psychiatry, 3(12), 1166-1175.
- Harmon KG, Drezner JA, Gammons M, et al (2013). American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med, 47: 15–26.
- Rivara, F. P., & Ford, M. A. (2014). Consequences of Repetitive Head Impacts and Multiple Concussions (R. Graham, Ed.). In Sports-Related Concussions in Youth: Improving the Science, Changing the Culture. Washington DC: National Academies Press (US).
- Alosco, M. L., Fedor, A. F., & Gunstad, J. (2014). Attention deficit hyperactivity disorder as a risk factor for concussions in NCAA division-I athletes. Brain injury, 28(4), 472-474.
- Iverson, G. L., Atkins, J. E., Zafonte, R., & Berkner, P. D. (2014). Concussion history in adolescent athletes with attention-deficit hyperactivity disorder. Journal of Neurotrauma, ja.
- Adeyemo, “mTBI and ADHD review meta-analysis,” 577.
- Chou, I.-C., Lin, C.-C., Sung, F.-C., & Kao, C.- H. (2014). Attention-deficit-hyperactivity disorder increases risk of bone fracture: A population-based cohort study. Developmental Medicine & Child Neurology, 56(11), 1111– 1116.
- Polanczyk G, de Lima MS, Horta BL, et al (2007). The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry, 164: 942-948.
- Willcutt EG (2012). The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics, 9: 490-499.
- Fayyad J, de Graaf R, Kessler R, et al (2007). Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry, 190: 402-409.
- Kessler, R.C., Adler, L., Ames, M., Demler, O., Faraone, S., Hiripi, E., Howes, M.J., Jin, R., Secnik, K., Spencer, T., Ustun, T.B., Walters,E.E. (2005). The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 35(2), 245-56.
- Adler, L.A., Spencer, T., Faraone, S.V., Kessler, R.C., Howes, M.J., Biederman, J., Secnik, K. (2006). Validity of pilot adult ADHD Self-Report Scale (ASRS) to Rate Adult ADHD symptoms. Ann Clin Psychiatry. Jul-Sep; 18(3): 145-8.
- Adler, L. A., Shaw, D. M., Spencer, T. J., Newcorn, J. H., Hammerness, P., Sitt, D. J., . .Faraone, S. V. (2012). Preliminary Examination of the Reliability and Concurrent Validity of the Attention-Deficit/Hyperactivity Disorder Self-Report Scale v1.1 Symptom Checklist to RateSymptomsofAttention- Deficit/Hyperactivity Disorder in Adolescents. Journal of Child and Adolescent Psychopharmacology, 22(3), 238-244.
- Guskiewicz, K. M., Register-Mihalik, J., Mccrory, P., Mccrea, M., Johnston, K., Makdissi, M., . . . Meeuwisse, W. (2013). Evidence-based approach to revising the SCAT2: introducing the SCAT3: Table 1. British Journal of Sports Medicine, 47(5), 289-293.
- Baron, D., Reardon, C., Baron, S. (2013). Clinical Sports Psychiatry: A Global Perspective. Wiley Press., London, England.
- Nelson, L. D., Guskiewicz, K. M., Marshall, S. W., Hammeke, T., Barr, W., Randolph, C., & Mccrea, M. A. (2015). Multiple Self-Reported Concussions Are More Prevalent in Athletes With ADHD and Learning Disability. Clinical Journal of Sport Medicine, 26(2), 120-127.
- Adeyemo 2014, Fann 2004, Alosco 2014.
- Bonfield, C. M., Lam, S., Lin, Y., & Greene, S. (2013). The impact of attention deficit hyperactivity disorder on recovery from mild traumatic brain injury. Journal of Neurosurgery: Pediatrics, 12(2), 97-102.
- Fann “Psychiatric Illness Following,” 60.
- Ilie, G., Vingilis, E. R., Mann, R. E., Hamilton, H., Toplak, M., Adlaf, E. M., Cusimano, M. D. (2015). The association between traumatic brain injury and ADHD in a Canadian adult sample. Journal of Psychiatric Research, 69, 174-179.
- Giza CC, Kutcher JS, Ashwal S, et al (2013). Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology, 80: 2250–57.
- Faraone, S., Asherson, P., Banaschewski, T., Biederman, J., Buitelaar, J., Ramos-Quiroga, J., Franke, B. (2015). Attention- deficit/hyperactivity disorder primer. Nature reviews. Disease primers, 1.
- Adeyemo 2014, Alosco 2014, Iverson 2014.