Information
Journal Policies
Far Away From Cities, More Limited Access to Mood Stabilizers: An Analysis On The Basis of the French Insurance Healthcare Database in Alsace
Bruno Michel1,2, Quentin Cormerais1, Marie-Christine Rybarczyk-Vigouret1, Sébastien Weibel3, Gilles Bertschy3, Hervé Javelot4, Morgane Beck1
2 Department Of Pharmacy, Strasbourg University Hospital; Humanis Ea7308, Faculty Of Pharmacy, Strasbourg, University Of Strasbourg, F-67000 Strasbourg, France.
3 Department Of Psychiatry, Mental Health And Addictology, Strasbourg University Hospital;Inserm U1114, Strasbourg; Translational Medicine Federation, University Of Strasbourg, F-67000 Strasbourg France.
4 Clinical Pharmacy Service, Mental Health Hospital (Epsan), F-67173 Brumath, France
Copyright : © 2016 Bruno M. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objectives: The aim of the study was to explore geographical differences in drug prescriptions regarding bipolar disorder in Alsace, a region of 1.86 million inhabitants (3% of the French population).
Methods: The study was conducted by using the French Insurance Healthcare databases. The investigation targeted patients, 20 years or older, who received, at least once in 2013, lithium, divalproex sodium or valpromide (two prodrugs of valproic acid).
Results: 4,661 patients were treated with one of the 3 mood stabilizers mentioned above (0.26% of inhabitants). Lithium was less prescribed than the others. The proportion of patients treated with mood stabilizers among the patients treated for mood disorder was higher in the larger cities areas suggesting a possible better access to diagnosis and specific treatment.
Conclusions: Our study contributed to a better understanding of medical practices relating to bipolar disorder in Alsace (France). Lithium is probably underused. Many patients with bipolar disorder may not receive the adequate treatment especially in rural areas. This result raises the question of the availability of information and/or specific training for psychiatrists but also for general practitioners who see a large number of bipolar patients.
Keywords: Bipolar Disorder; Health Insurance Database; Lithium; Prodrugs of Valproic Acid; Antidepressants.
1.Introduction
Bipolar disorder is characterized by recurrent mania or hypomania and depressive episodes [1]. Patients with bipolar disorder require both acute and steady therapies. Numerous prescribing guidelines are available; however the most common drugs used for bipolar disorder in France are mood stabilizers such as lithium, divalproex sodium and valpromide (two prodrugs of valproic acid), followed by other drugs with mood stabilizer action: (i) various antiepileptic drugs (e.g. carbamazepine, lamotrigine) and/or (ii) atypical antipsychotics (e.g. aripiprazole, asenapine, olanzapine, quetiapine, risperidone) [2,3]. Treatment for acute bipolar depression may integrate a mood stabilizer plus an antidepressant [2].
By using data extracted from the French Insurance Healthcare system, the aim of the study was to explore differences in prescriptions practices of lithium, divalproex sodium and valpromide according to the geographical location of the patients in Alsace (France).
2. Methods
A retrospective study was conducted by OMEDIT Alsace (Observatoire du Médicament, des Dispositifs médicaux et de l’Innovation Thérapeutique) from January 1, 2013 to December 31,2013 by using the French Insurance Healthcare database: ERASME (Extraction, Recherches, Analyses pour un Suivi Médico-Economique).
ERASME is an outpatient database. It is part of the SNIIRAM (Système National d’Information Interrégimes de l’Assurance Maladie) data warehouse of National Health Insurance that records anonymised data about French patients who benefit from medical care. Its access is restricted to authorized personal specified through a national policy. The information was made available following the approval of the French data protection Committee CNIL (Commission nationale de l’informatique et des libertés). The data extracted are related to the population of patients residing and insured in Alsace under the general scheme managed by CNAMTS (Caisse Nationale de l’Assurance Maladie des Travailleurs Salariés) which covered 80% of the residents in Alsace [4].
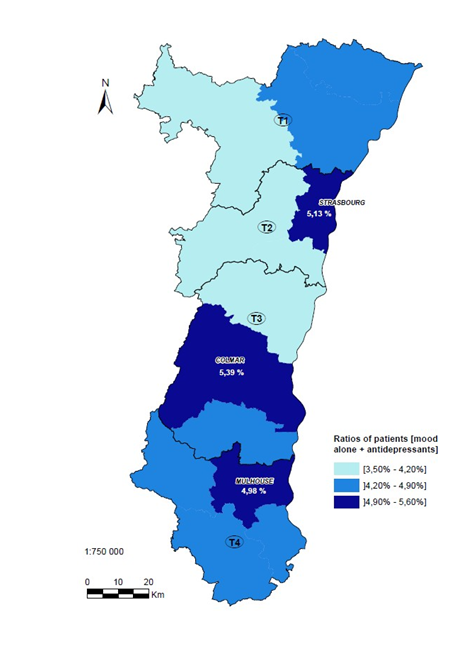
Alsace is a region of 1.86 million inhabitants (3% of the French population). Alsace is divided into four health territories, T1 through T4 (from North to South, see figure 1). Urban zones were also identified around the main cities of Alsace: Strasbourg (which belongs to T2), Colmar (T3) and Mulhouse (T4).
Three mood stabilizers were the object of a focus: lithium, divalproex sodium and valpromide. The use of antidepressants was explored considering N06A ATC (Anatomical Therapeutic Chemical) code.
The investigation targeted patients, 20 years or older, who received, at least once in 2013, one of the 3 specific mood stabilizers mentioned above and/or antidepressants. The number of patients treated, their geographical location, gender and age were sought. The proportion of patients treated for bipolar disorder according to their location was also analyzed as followed:
Ratio (for a specific health territory or zone) = mood stabilizers (alone or with antidepressants ) / mood stabilizers alone + antidepressants (alone or with mood stabilizers)
The numerator corresponded to the number of patients with detected bipolar disorder. The denominator represented the number of patients already detected and the patients under antidepressants. The rationale is that the numerator is a proxy for the prevalence of detected cases of bipolar disorder whereas the denominator is a proxy for the prevalence of patients with mood disorders including bipolar disorder misdiagnosed and treated as unipolar depression.
Statistical analyses were computerized using R, version 3.2.2. Geographical location of patients was studied using comparison of proportions. A p-value below 0.05 was considered to be of statistical significance.
3. Results
There were 4,661 patients treated with the studied mood stabilizers, i.e. 0.26% of Alsace inhabitants in 2013, with a male/female sex ratio of 0.77. The mean age of patients was 52 ± 15 years old. Three hundred and forty three patients were under 30 years old (7.4 %), 2,849 were between 30 and 59 years old (61.1%) and 1,469 were 60 years and older (31.5%). Two thousand and ninety two patients (44.9%) were treated with mood stabilizers alone and 2,569 (55.1%) with both mood stabilizers and antidepressants.
Lithium (13,335 medicine packs delivered by community pharmacists) was less prescribed than valpromide (24,997 packs) and divalproex sodium (24,606 packs).
Ratios between patients according to their location were as followed: T1 (North Alsace): 4.2 % (856 patients/20,294); T2:4.8 % (1,546/32,098); T3: 4.8 % (1,002/20,737); T4 (South Alsace): 4.8% (1,230/25,397) (figure 1). There were statistical differences between T1 vs. the other health territories (p-values < 0.01). Statistical differences were also observed between rural and urban zones [4.2 % (2,603/50,674) vs. 5.1% (2,031/47,852); p-value < 0.01] showing more patients treated for bipolar disorder in the areas of Strasbourg, Colmar and Mulhouse.
4. Discussion
The current study described, in a real-life setting, disparities in prescription practices of lithium and 2 prodrugs of valproic acid in Alsace by using ERASME, a French Insurance Healthcare database.
The primary objective of medico-administrative databases such as ERASME is to provide information about payment of medical care but their usefulness is now well accepted to study health-care issues [4]. The use of ERASME had however some limits. Firstly, patients who were not insured under the general scheme were not taken into account (20 % of Alsatians). Secondly, data about drugs which are commonly used in bipolar disorder such as carbamazepine, lamotrigine and antipsychotic agents were lacking. It was indeed not possible to analyze the data from drugs which have broader indications than bipolar disorder. Finally, inpatient drug-treatments during hospital stays were not included.
Lithium is the historic and gold standard of treatment for bipolar disorder [5]. As shown in our study, the drug was surpassed in clinical use (but maybe not in efficacy) by the mood-stabilizing agents: divalproex sodium and valpromide. This low use of lithium is consistent with the recent French study of Verdoux et al. [6]. This trend also consolidates data collected by Benazzi and could be explained by the need for closer monitoring with lithium compared to other mood-stabilizing agents [5].
In our study, there were 4,661 patients treated for bipolar disorder, corresponding to 0.26% inhabitants in Alsace in 2013. This result cannot be treated as prevalence since patients presenting with bipolar disorder are not necessarily and exclusively treated by lithium, divalproex sodium or valpromide. However, it is not markedly different from data already published [7]. Bipolar disorder usually begins in late adolescence or early adulthood [we found 343 (7.4%) patients under 30 years old], is more common in women than in men (our sex ratio was 0.77) and has a lifetime prevalence starting from 0.5% according to Kleinman et al and could be around 1.5 % in the general population [2,7].
The diagnosis of bipolar disorder is difficult. Depression occurring in bipolar disorder cannot be easily distinguished from unipolar depression. Some patients suffering from bipolar disorder may thus be misclassified as having depressive disorder. Our study revealed this finding particularly in the north of Alsace where the value was statistically lower than in the other parts of Alsace. These geographical disparities corroborate studies that present a significant under-use of mood stabilizers [8]. Our results also revealed a significant difference between the rural and the main urban zones of Alsace. This indicates that bipolar disorder could be underdiagnosed in rural areas and/or could be more prevalent in urban zones even if it is currently considered that bipolar disorder affects patients independently of ethnic background or of socioeconomic status [7]. This latest hypothesis of a higher prevalence of bipolar disorder in urban has nevertheless been formulated by Rouillon but needs further investigations [7]. In our opinion, the difference in prescription rates would be more related to an under-diagnose and/or under-treatment of bipolar disorder for patients who do not live in urban areas. In France, private psychiatrists are predominantly concentrated in the largest cities [9]. Thus patients with bipolar disorder ouside the largest cities would likely consult their general practitioner (where they receive an antidepressant prescription when they are depressed) instead of psychiatrists.
5. Conclusion
Our study contributed to a better understanding of drug prescriptions practices relating to bipolar disorder in Alsace. Lithium is probably underused. Many patients with bipolar disorder may not receive the adequate treatment especially in the north of Alsace and in rural areas. This result raises the question of the availability of information and/or specific training for psychiatrists but also for general practitioners who see a large number of bipolar patients. A regional network of counseling in psychopharmacology could appear as a useful tool for optimizing pharmacologic management of bipolar disorder.
6.Acknowledgements
The authors would like to thank Valérie Leray for proof reading and linguistic review of the manuscript and Catherine Lukasek for support with the design of the study.
7.Statement of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
8.Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Anderson IM, Haddad PM, Scott J. Bipolar disorder. BMJ 2012; 27:345-355.
- Kleinman L, Lowin A, Flood E, Gandhi G, Edgell E, Revicki D. Costs of bipolar disorder.Pharmacoeconomics 2003; 21(9):601-22.
- Stahl MS. The prescriber’s guide. Antipsychotic and mood stabilizers, Stahl's Essential Psychopharmacology, 3rd Edition, Cambridge University Press; 2009.
- Beck M, Velten M, Rybarczyk-Vigouret MC, Covassin J, Sordet C et al. Analysis and breakdown of overall 1-year costs relative to inpatient and outpatient care among rheumatoid arthritis patients treated with biotherapies using health insurance claims database in Alsace. Drugs - Real World Outcomes 2015; 2 (3): 205-215.
- Benazzi F. Bipolar disorder: focus on bipolar II disorder and mixed depression. Lancet 2007; 369: 935-945.
- Verdoux H, Pambrun E, Cortaredona S, Coldefy M, Le Neindre C, Tournier M et al. Geographical disparities in prescription practices of lithium and clozapine: a community-based study. Acta Psychiatr Scand 2016; 133: 470–480.
- Rouillon F. Bipolar disorder: epidemiology. Annales Medico-Psychologiques 2009; 167 : 793–795.
- Dardennes R, Thuile J. Even C, Friedman S, Guelfi JD.The costs of bipolar disorder.L’Encéphale 2006; 32:18-25.
- Conseil National de l’Ordre des Médecins (2016) La démographie médicale - cartographie interactive. https://www.conseil-national.medecin.fr/ [August 1st june 2016].