Information
Journal Policies
Accuracy of Performing Home-Based Exercises in Musculoskeletal Disorders: A Cross-Sectional Study
Emin Ulas ERDEM1, Eda AKBAS1*, Banu UNVER1
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background: Home-based exercises (HBE) have been constantly used for the management of musculoskeletal problems. Despite, adherence to HBE have been investigated widely, patients’ exercise performing accuracy was not been considered.
Objective: The purpose of this study was to investigate HBE performing accuracy in patients with musculoskeletal disorders.
Patients and Methods: A total of one-hundred fourteen patients allocated to the study (five groups; posture (n=22), knee (n=21), shoulder (n=15), back (n=39) and neck (17)). All patients were instructed HBE therapy including five different exercise according to his/her group by an experienced physiotherapist. After six weeks, instructed exercises are requested to perform from patients. Five-point scale was used for assessing the exercise accuracy performance. Also pain intensity was measured with visual analogue scale.
Results: There were no difference in performing accuracy scores of HBE among the groups (p>0.05). There were significant differences among performing accuracy scores of the exercises in knee and shoulder group (p< 0.05). No significant difference was found in any group after six-week HBE program (p>0.05).
Conclusion: Our study exhibited that the performing accuracy of HBE in patients with musculoskeletal problems was low to moderate. Regular auditing of exercises may reduce compensations and improving the effect of HBE in patients with musculoskeletal disorders.
Home-based exercise, auditing the exercise, exercise compensation, adherence to exercise,Orthopedics
1. Introduction
The home-based exercise (HBE) programs are widely used as an efficient, cheap, non-invasive and easily accessible part of musculoskeletal rehabilitation. HBE programs aim to increase the effectiveness of the treatment by applying the set of exercises determined outside the clinic in certain sets and repeats [1]. Besides, a careful and attentive arranged HBE program significantly reduces the recurrence rate [2]. On the other hand, several factors such as follow-up difficulties, faith to exercise, and suspense of regularity and accuracy constitute hidden aspects of HBE programs. Age, gender, occupation, motivation, education level, intellectual status, disability level and previous exercise experiences influence adherence to HBE [3-6].
There are several studies and reviews that emphasize the benefits of home-based exercises in musculoskeletal conditions[7-10]. Fransen et al. indicated that HBE is significantly efficient in reducing pain and improving physical functions in knee osteoarthritis [8]. Another review about subacromial impingement syndrome states that HBE and corticosteroid injection are equally effective in low grade shoulder pain [9].
Performing the exercises adequately and properly as prescribed is an overlooked aspect of unsupervised HBE programs. World Health Organization defines the term adherence as “the extent to which a person’s behaviour – taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider” [11]. To date, there are several studies investigating adherence to HBE, and poor adherence was revealed as a major problem of HBE. Unfortunately, the rate of adherence to unsupervised HBE is known to be about 50% in musculoskeletal rehabilitation programs [5,6,12-16]. This fact directly influences the real success rate of HBE therapy [1].
On the other hand, adherence to HBE rehabilitation is evaluated mostly with subjective self-report scales [17]. Moreover, even if the patients adhere to the number and frequency of their exercises accurately, it is hard to be sure if they perform their exercises adequately/properly as instructed. There are few studies investigating about the accuracy of performing the exercises correctly [15]. Therefore, the aim of this study was to investigate the performing accuracy of HBE and further effectiveness of HBE rehabilitation in patients with musculoskeletal disorders.
2. Methods
This study was approved by Zonguldak Bülent Ecevit University Clinical Researches Ethical Committee (approval id number: 2018-106-11/04). All patients was informed about the details of the study and signed an informed consent form.
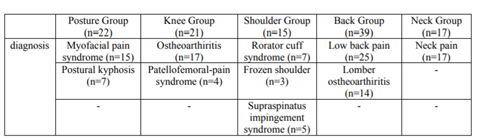
One hundred and fourteen participants who applied to the outpatient clinic of physiotherapy and rehabilitation, and recommended HBE for musculoskeletal problems were included to the study. Five different groups were designed as posture exercise group (n=22), knee exercise group (n=21), shoulder exercise group (n=15), back exercise group (n=39), and neck exercise group (n=17). The diagnoses of the participants were presented in Table 1.
Inclusion criteria were, being age between 18-65, being literate, having a-full cooperation, and being diverted to a HBE program for posture, knee, shoulder, back, or neck problems. Exclusion criteria were, any neurological disorders, and receiving any HBE therapy previously.
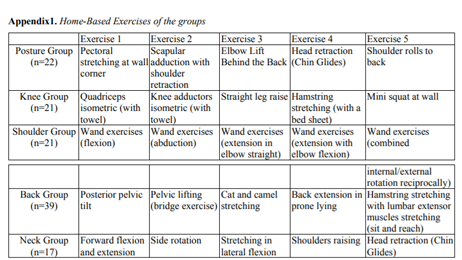
All participants were instructed a HBE program according to his/her group by the same experienced physiotherapist. For each group, five different exercises were instructed to the participants. Before the instruction; physiotherapist make a short conversation about the benefits of HBE. Each exercise was instructed briefly, then, demonstrated the by the physiotherapist at first, and finally performed by the patient. An adequate number of set and repetitions was ordered to patient. HBE was prescribed preferably in each day/week frequency and a total of six weeks. Also an explanatory and illustrative brochure about the exercise program was given to the patient. The details of the exercise program was described in Appendix 1.
At the end of six weeks, a control appointment date was given to the patients. Patients were required to show and perform their exercises. A five-point scale was used to determine the performing accuracy score of the exercise (0= do not remember exercise, 1=perform the exercise irrelevantly, 2=perform the exercise partially but compensate, 3=perform the exercise almost precisely, 4=perform the exercise precisely). The scores of each exercise were recorded, and the score of the each group’s exercise program was obtained by dividing the sum score of the exercises by five. All the assessments were accomplished by the same physiotherapist.
The pain intensity of the patients was measured with visual analogue scale (VAS) before and after six weeks HBE therapy.
Data was evaluated using the Statistical Package for Social Science 18 (SPSS Inc., Chicago, IL, USA) program for Windows. The significance level was set to p< 0.05. Normality tests (visual and analytical) showed that numerical data did not distribute normally. Age, BMI, and performing accuracy of the groups, and performing accuracy of the exercises in each group were compared using the Kruskal-Wallis test. The Mann-Whitney U test with Bonferroni correction was used with a presumption of p=0.0005 for significant pairwise comparisons. The Wilcoxon test was used to compare to change in pain intensity of the groups between baseline and six weeks. Chi-square test was used to compare gender distribution among the groups.
3. Results
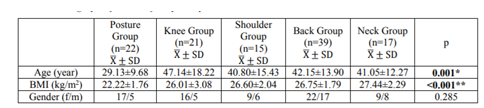
The demographic data were presented in Table 2. Mean age of the posture group was significantly lower compared to knee, back, and neck groups (p< 0.001). Also a significant difference was found in body mass index of posture group compared to other groups (p< 0.001).
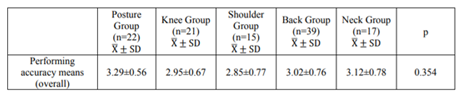
Means and standard deviations of the performing accuracy scores according to groups was shown in Table 3. There were no difference in performing accuracy scores of HBE among the groups (p>0.05). The lowest mean of performing accuracy score was determined in shoulder group.
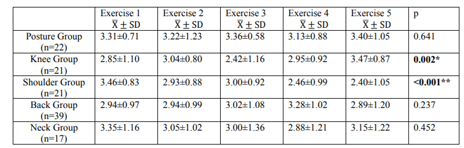
Means and standard deviations of each exercise’s performing accuracy score were demonstrated in Table 4. There were significant differences among performing accuracy scores of the exercises in knee and shoulder group (p< 0.05).
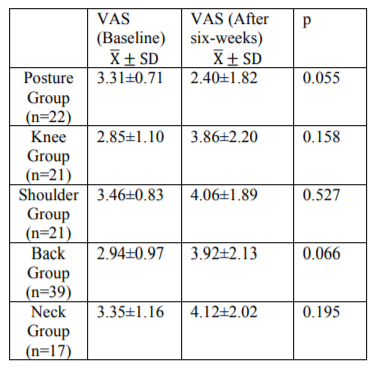
Results of pain intensity were shown in Table 5. No significant difference was found in any group after six-week HBE program (p>0.05).
4. Discussion
This cross-sectional study aimed to determine the performing accuracy of HBE. Our results revealed that patients performed most of their home exercises with a compensation. The worse performing accuracy were found in shoulder and knee groups; in “straight leg raise”, “wand exercises-extension with elbow flexion”, and wand exercises-combined internal/external rotation reciprocally” exercises. The patients in posture group performed the exercises better than others. Finally, our results showed that six-week HBE program was not effective in reducing the pain in musculoskeletal problems.
Home-based exercises for musculoskeletal disorders have been assessed with the aspect of adherence or compliance in several studies [3,12,18,19], however, the literature was limited about the performing accuracy of HBE to compare with our results. Faber et al. investigated whether healthy students perform shoulder abduction home exercise correctly with an elastic band after two weeks. They found that most of the participants could not perform the exercise correctly as instructed [15].
Home-based exercises are utilized in physiotherapy outpatient clinics with a wide spectrum for the management of musculoskeletal problems [20-23]. Applying the exercise correctly is crucial for providing adequate benefit. There are several parameters that can affect the exercise learning such as socio-cultural status, faith to exercise, previous experiences, complexity of the exercises and teaching attitudes of the physiotherapists. Chan and Can evaluated the patients’ HBE adherence level, and they pointed that the time spent on instructing the exercises to the patients was effective for the adherence [12].
In order to perform an exercise adequately, subjects should not compensate with an irrelevant movement. To our results, performing accuracy was lower in straight leg raise and wand exercises. Straight leg raise exercise consists of several stages (leg rise with quadriceps isometric contraction and ankle dorsiflexion), and requires more attention and muscle strength. Wand exercises are usually prescribed to increase shoulder range of motion, but they are prone to compensated with trunk movements. Performing accuracy of posture group was better than other groups. The posture group were younger than the other groups, and posture exercises are easier to learn and more simple according to the others. These may explain the better performing accuracy of posture group.
HBE are prescribed to increase the mobility, restoring muscle strength, improve function and also alleviating the pain [24,25]. Our study revealed that pain intensity remained similar after six-week HBE. The therapeutic effect of HBE is seem to be suspicious in pain management according to this result.
This study has some limitations. Posture group were younger than other groups, so this difference might affect their performing accuracy. Also, we did not evaluate whether the participants performed their HBE regularly (set/ repetition/frequency) as prescribed.
5. Conclusion
In conclusion, this study exhibited that the performing accuracy of HBE in patients with musculoskeletal problems was low to moderate. Most of the home exercises were performed with some compensations. Posture exercises were tended to have better performing accuracy. HBE was seem to be ineffective in pain management. Regular audit may be recommended for reducing compensations and improving therapeutic effect of HBE in patients with musculoskeletal disorders.
References
- J. PK, M. HD. A model to increase rehabilitation adherence to home exercise programmes in patients with varying levels of self-efficacy. Musculoskeletal Care 2018, 16(1):233-237.
- Picorelli AM, Pereira LS, Pereira DS, Felicio D, Sherrington C. Adherence to exercise programs for older people is influenced by program characteristics and personal factors: a systematic review. Journal of physiotherapy 2014, 60(3):151-156.
- Slade S, Patel S, Underwood M, Keating J. What are patient beliefs and perceptions about exercise for non-specific chronic low back pain: a systematic review of qualitative research. Physiotherapy 2015, 101:e1407.
- Bachmann C, Oesch P, Bachmann S. Recommendations for Improving Adherence to Home-Based Exercise: A Systematic Review. Phys Med Rehab Kuror 2018, 28(01):20-31.
- Medina-Mirapeix F, Escolar-Reina P, Gascon-Canovas JJ, Montilla-Herrador J, Jimeno-Serrano FJ, Collins SM. Predictive factors of adherence to frequency and duration components in home exercise programs for neck and low back pain: an observational study. BMC musculoskeletal disorders 2009, 10:155.
- Mailloux J, Finno M, Rainville J. Long-Term Exercise Adherence in the Elderly with Chronic Low Back Pain. American Journal of Physical Medicine & Rehabilitation 2006, 85(2):120-126.
- Hennig T, Hæhre L, Hornburg VT, Mowinckel P, Norli ES, Kjeken I. Effect of home-based hand exercises in women with hand osteoarthritis: a randomised controlled trial. Annals of the Rheumatic Diseases 2015, 74(8):1501-1508.
- Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee: a Cochrane systematic review. British Journal of Sports Medicine 2015.
- Abdulla SY, Southerst D, Côté P, Shearer HM, Sutton D, Randhawa K et al. Is exercise effective for the management of subacromial impingement syndrome and other soft tissue injuries of the shoulder? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Manual Therapy 2015, 20(5):646-656.
- Liang H, Zhang H, Ji H, Wang C. Effects of home-based exercise intervention on health-related quality of life for patients with ankylosing spondylitis: a meta-analysis. Clinical Rheumatology 2015, 34(10):1737-1744.
- Sabaté E. Adherence to long-term therapies: evidence for action: World Health Organization; 2003.
- Chan D, Can F. Patients’ adherence/compliance to physical therapy home exercises. Fizyoterapi Rehabilitasyon 2010, 21(3):132-139.
- Forkan R, Pumper B, Smyth N, Wirkkala H, Ciol MA, Shumway-Cook A. Exercise Adherence Following Physical Therapy Intervention in Older Adults With Impaired Balance. Physical Therapy 2006, 86(3):401-410.
- H. vGC, H. PBWJ, M. KGIJ, Jack RW, D. MG, M. vEJT, Marco P, P. MS. Effects of exercise adherence on physical function among overweight older adults with knee osteoarthritis. Arthritis Care & Research 2005, 53(1):24-32.
- Faber M, Andersen MH, Sevel C, Thorborg K, Bandholm T, Rathleff M. The majority are not performing home-exercises correctly two weeks after their initial instruction—an assessor-blinded study. PeerJ 2015, 3:e1102.
- Jakobsen MD, Sundstrup E, Brandt M, Jay K, Aagaard P, Andersen LL. Effect of workplace-versus home-based physical exercise on musculoskeletal pain among healthcare workers: a cluster randomized controlled trial. Scandinavian journal of work, environment & health 2015, 41(2):153-163.
- Bollen JC, Dean SG, Siegert RJ, Howe TE, Goodwin VA. A systematic review of measures of self-reported adherence to unsupervised home-based rehabilitation exercise programmes, and their psychometric properties. BMJ Open 2014, 4(6).
- Bonnechere B, Jansen B, Omelina L, Jan SVS. Do Patients Perform Their Exercises at Home and why (not)? A Survey on Patient Habits during Rehabilitation Exercises. Ulutas Med J 2016, 2(1):41-46.
- F. PM, Cindy V, G. SF, R. TJW, Joost D, H. DBD. Exercise adherence improving long-term patient outcome in patients with osteoarthritis of the hip and/or knee. Arthritis Care & Research 2010, 62(8):1087-1094.
- Bennell KL, Campbell PK, Egerton T, Metcalf B, Kasza J, Forbes A et al. Telephone Coaching to Enhance a Home-Based Physical Activity Program for Knee Osteoarthritis: A Randomized Clinical Trial. Arthritis Care & Research 2017, 69(1):84-94.
- Latham NK, Harris B, Bean JF, et al. Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture: A randomized clinical trial. JAMA 2014, 311(7):700-708.
- Uhl TL, Rice T, Papotto B, Butterfield TA. Effectiveness of a Home-Based Eccentric-Exercise Program on the Torque-Angle Relationship of the Shoulder External Rotators: A Pilot Study. Journal of Sport Rehabilitation 2017, 26(2):141-150.
- Buker N, Kitis A, Akkaya S, Akkaya N. Comparison of the results of supervised physiotherapy program and home-based exercise program in patients treated with arthroscopicassisted mini-open rotator cuff repair. Eklem Hastalik Cerrahisi 2011, 22(3):134-139.
- Ludewig PM, Borstad JD. Effects of a home exercise programme on shoulder pain and functional status in construction workers. Occupational and Environmental Medicine 2003, 60(11):841-849.
- Mintken PE, McDevitt AW, Cleland JA, Boyles RE, Beardslee AR, Burns SA et al. Cervicothoracic Manual Therapy Plus Exercise Therapy Versus Exercise Therapy Alone in the Management of Individuals With Shoulder Pain: A Multicenter Randomized Controlled Trial. Journal of Orthopaedic & Sports Physical Therapy 2016, 46(8):617-628.