Information
Journal Policies
Retrospective Study of HIV and Tuberculosis Co-Infection among HIV Sero-Positive Patients in Kano, Nigeria
Muhammad Ali1*, Muhammad S Abdallah2
2.Desert Research Monitoring and Control Centre, Yobe State University Damaturu, Nigeria.
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The HIV/Tuberculosis co-infection is a major public health problem in many parts of the world. The study was aimed at determining the prevalence of HIV/Tuberculosis Co-infection among HIV Sero-positive patients attending HIV some health centres in Kano State Nigeria. This is a retrospective study involving 286 of case files of HIV sero-positive patients attending Murtala Muhammad Specialist Hospital and Infectious Disease Hospital Kano State between July and December, 2016. The results showed that 32 out of 286 HIV sero positive subjects (11.2 %) were co-infected with HIV and Tuberculosis. With respect to age of subjects the highest prevalence of co-infection was observed among patients aged 31-40 years 37.5%. The burden of the co-infection was more on males, 56% than females (44%). The prevalence of co-infection is higher among married individuals, 40.6% than the single individuals, 25%, divorced and widows with 18.7% and 15.6 subjects respectively. By educational status, co-infection rate was higher among subjects who lack formal education, 46.8% when compared with those having tertiary education 37.5% and secondary education 15.7%. Also those who live in urban centres have highest co-infection, 40.6%, while those in semi-urban and rural centres have a total of 34.4% and 25% subjects respectively. By social status, the co-infection is highest among students category, 8 25%. The trend of co-infection by the subjects is statistically not significant at p< 0.05.
HIV, Tuberculosis, co-infection, prevalence, retrospective,Immunology and Vaccines
1. Introduction
Human Immune deficiency Virus (HIV) is a retro virus identified as the etiologic agent for acquired immune deficiency syndrome (AIDS), while tuberculosis (TB) is an air borne infection caused by the tubercle bacillus mycobacterium tuberculosis (MTB) [1,2]. TB is a global health priority being a killer disease that manifest in its pulmonary form in up to 70% of cases or as extra pulmonary affecting all parts of the body [3]. Africa is facing the worst tuberculosis epidemic since the advent of the antibiotics era. Driven by a generalized human immune deficiency virus (HIV) epidemic and compounded by weak health care systems, inadequate diagnostic laboratories and conditions that promote transmission of infectious agents, the devastating situation has become exacerbated by the emergence of drug-resistant strains of mycobacterium tuberculosis [4,5]. HIV and TB are two leading causes of death and continue to be serious problems in developing countries [6].
Worldwide, the human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) epidemic has been accompanied by a severe epidemic of tuberculosis [7]. HIV infection is the leading risk factor for TB. HIV promotes progression of latent or recent infections of mycobacterium tuberculosis to active disease and also increases the rate of occurrence of TB [8]. People living with HIV may also be more susceptible to TB infection because Human Immunodeficiency Virus (HIV) has paved way for the resurgence of Mycobacterium tuberculosis infection[9]. While HIV is the most powerful risk factor for the progression of M tuberculosis infection to TB disease, TB accelerates the progression of HIV infection to AIDS and shortens the survival of such patients [10]. HIV is the first and TB is the second leading cause of death from infectious disease Worldwide [11]. Globally 2 billion people are estimated to be latently infected with tuberculosis [12]; whilst, there are an estimated 35.3 million people living with HIV, 70% of who live in sub-Saharan Africa [13]. Annually, there are an estimated 8.7 million (range 8.3-9.0 million) new cases of TB, and 2.5 million new HIV infections [12,13]. Of the 8.7 million new cases of TB in 2011, 1.1 million (13%) were among people living with HIV [13].
The two are intricately linked to malnutrition, unemployment, poverty, drug abuse and alcoholism and have also been referred to as the ‘Cursed Duet’. De Riemark et al. [14] noted that HIV infection has a major impact on the risk of TB. This viral infection is characterized by a progressive depletion of CD4+T lymphocytes. This results in the destruction of the immune system leaving the victim vulnerable to a host of opportunistic infection, neurological disorders or malignancies [15,16]. HIV is known to increase the risk of reactivation in people with latent tuberculosis and also increases the risk of subsequent episodes of TB from exogenous re-infection [17].
There have been several studies of the prevalence of HIV in TB patients in different parts of Nigeria, with prevalences of 6.1% in Jos, [18] 12.7% in Ife [19], 19% in Maiduguri, [20] and 28.1% in Ibadan [21]; the national median is 17.0% [22]. Elsewhere in Africa, higher prevalences of 33.2%, 3.6%, and 57.1% were reported in Chad [23], Tanzania [24] and Ethiopia [25] respectively. In a study conducted by Iliyasu and Babashani [8] on prevalence and prediction of TB co-infection among HIV sero-positive patients attending Aminu Kano Teaching Hospital, Northern Nigeria, a total of 1320 HIV/AIDS patients had complete records and were reviewed, among which 138 (10.5%) were co-infected with TB. Prevalence and known risk factors for Tuberculosis among HIV infected patients vary from one setting to another [26]. The global prevalence of Tuberculosis-HIV is reported to be 0.18% [27], with reports of 17% in Nigeria [22] and 19.0% in Durban South Africa [28]. Despite these high prevalences of co-infection and its attendant problems to the global community, only a little is being done to address HIV and Tuberculosis co-infection. The WHO reports that only 2.4% of all people living with HIV or AIDS are even being tested for Tuberculosis [29]. The present study is aiming to determine the HIV and TB co-infection among HIV sero-positive patients attending some tertiary hospitals in Kano, Nigeria.
2. Material And Methods
The study was conducted following ethical approval obtained from the Health Services Management Board, Kano State based on the consent of Ethical Committee of Murtala Muhammad Specialist Hospital and Infectious Disease Hospital Kano State.
Kano State is one of the largest states of the Nigerian federation. It is located in North Western Nigeria. On map Kano is located on Longitude 8°30'E and latitude 12° N. the state has a total area of 20,131 km2. The metropolis of the state comprises of 6 Local Governments (Kano municipal Fagge, Dala, Gwale, Tarauni and Nassarawa) with total area of 137 km2 It has a total area of 20,131 km2 and population of 2,163,25 within the metropolis as at 2006. The climate of Kano has been described as ‘AW’ type as identified by Koppen’s climatic classification [30].
The study was a retrospective review of cases of HIV and Tuberculosis recorded between July and December, 2016 from Murtala Muhammad Specialist Hospital and Infectious Disease Hospital Kano State were reviewed and used for the study. Relevant information such as age, sex, socio economic status, immunization status and clinical presentation of the subjects for period of 6 months were retrieved and reviewed for analysis. A total of 286 patients that were diagnosed with HIV and enrolled in the study centre were considered in the present study.
At the study centre HIV infection was diagnosed based on suggestive clinical symptoms and positive spot test for HIV antibodies. Blood samples were collected from all of the consenting patients and screened for the presence of HIV-I and HIV-2 using a chromatographic qualitative ELISA test kit according to the manufacturer’s instructions. All ELISA positive samples were further confirmed by Western Blot. The diagnosis of tuberculosis was made using a combination of the following; history of cough greater than three weeks, contact with adult with chronic cough/confirmed TB, weight loss, fever greater than one month, and abnormal chest radiograph, positive mantoux test of > 5mm in diameter, identification of acid fast bacilli (AFB) in sputum, gastric or body fluids, and non-response to conventional antibiotics. The incidence of HIV/TB co-infection was determined as a proportion of HIV sero-positive individuals to the total number of patients under consideration and expressed as a percentage.
The data was analyzed using Statistical Package for Social Science (SPSS) 2010 version software. Quantitative variables were summarized using the appropriate summary indices while categorical variables were tabulated using frequencies and percentages. The chi-square test was used for testing the significance of differences between categorical variables. A p value of less than 0.05 was considered as statistically significant.
3. Results
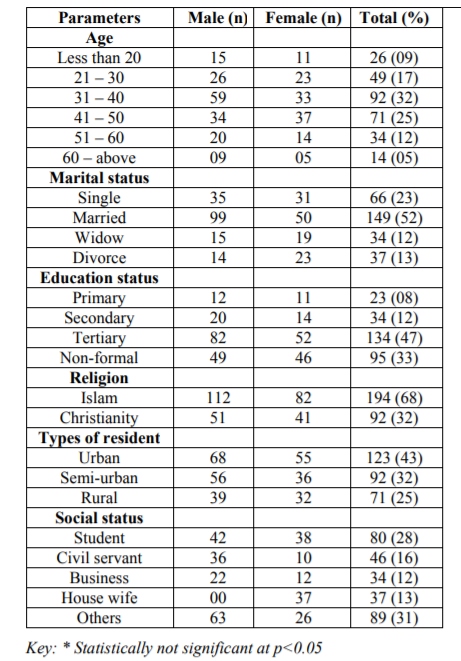
The demographic distribution of HIV sero-prevalence subjects used in this study is presented in Table 1. A total record of 286 subjects was reviewed in this study. Of the case files reviewed, 163 (57%) of the patients were males and 123 (43%) were females. Subject age ranged from less than 20 to above 60 years.
Majority of the subjects (32%) aged between 31 to 40 years, and few subjects were found in the age category above 60 years and below 20 years. Most of the subjects were Muslim which accounted for 68% while Christian subjects accounted for 32%. A total of 123 of the subjects (43%) were from urban centres while 92 subjects (32%) and 71 subjects (25%) were from semi-urban and rural centres respectively. A total of 149 (52%) subjects were married, 34 (12%) were widowed, 66 (23%) were single, and 37 (13%) were divorced. Majority of the subjects (134) attended tertiary institution which accounted for 47%, 34 (12%) attended secondary schools, 23 (08%) attended primary schools while 95 (33%) lack formal education.
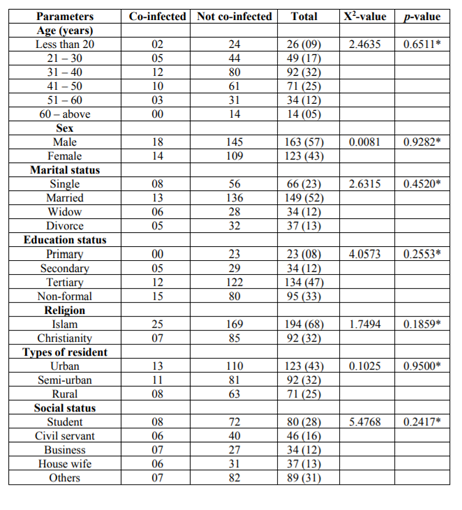
The prevalence of HIV/Tuberculosis co-infection among HIV sero-positive subjects is presented in Table 2. The results showed that 32 subjects accounted for 11.2 % were co-infected with HIV and Tuberculosis. With respect to age of subjects the highest prevalence of co-infection was observed among patients aged 31-40 years 12(37.5%), this was followed by those 41-50 years 10(31.2%) while no prevalence occurred among those 61 years of above. This trend was statistically not significant, (X2 = 2.4635, p = 0.6511). The burden of the co-infection was more on males, 18 (56%) than females, 14 (44%). The prevalence of co-infection is higher among married individuals, 13(40.6%) than the single individuals, 08(25%), divorced and widows with 6 and 5 subjects respectively. By educational status, co-infection rate was higher among subjects who lack formal education, 15 (46.8%) when compared with those having tertiary education 12 (37.5) and secondary education 5 (15.7%). Also those who live in urban centres have highest co-infection, 13 (40.6%), while those in semi-urban and rural centres have a total of 11 (34.4%) and 8 (25%) subjects respectively. By social status, the co-infection is highest among students category, 8 (25%), the trend of co-infection by social status of the subjects is statistically not significant at p< 0.05.
4. Discussion
The HIV/Tuberculosis co-infection is a major public health problem in many parts of the world. The present study investigates the prevalence of Tuberculosis among HIV sero-positive patients at some health centres in Kano Nigeria. A total of 286 cases of patients recorded between July and December, 2016 that were diagnosed with HIV and enrolled in the study centre were reviewed and considered in the present study.
In the present study, 11.2% of HIV sero-positive subjects were co-infected with Tuberculosis. Several studies were conducted on HIV and Tuberculosis by Many researchers. The finding of this study was in conformity with several finding found in many health centres in Nigeria. Reports of similar studies in Nigeria ranged from 12.0% in Ile-Ife [19], 10.0% in Kano [8], 23.6 at Nguru [31], 10.5% and 14.9% among children and adults respectively in Sagamu [32], 10.8% in Irrua [33], 6.1% among those aged 20-40 years in Jos [18] and 4.2% in Oyo [34]. Others reported 28.12% in Ibadan [21], 19.0% in a semi arid region of Nigeria [35] and 16.6% in Delta state in a population suspected of TB and HIV [36]. The differences in prevalence in the other Nigerian studies reported could be due to selection factors; some of the studies were conducted before free antiretroviral drugs were provided in government hospitals while in some others the variations in prevalence may be due to differences in methodology used.
The age distribution reveals highest prevalence to be in the age group 31-40yrs (37.5%) followed by 41- 50yrs (31.2%). The higher prevalence of HIV co-infection among TB patients observed among the above age group in this study is consistent with the findings of other studies [37,38]. This age prevalence of TB co-infection among HIV patients probably reflects the age-specific prevalence of HIV in the community. This may be related to patients being in a sexually active age group in which both TB and HIV prevail most. The other possible explanation for this may be their increased family, organizational, and societal responsibilities as people in this age group involve themselves in various extraneous daily activities in order to win the socio-economic hardship which increases the frequency of their contact with other patients in their society [39].
According to the present study, there was a significantly higher prevalence of HIV/ Tuberculosis co-infection, found among males than females (although the burden of the disease was more among the female population). This was in conformity with the pattern reported in Port-Harcourt [40] and Jos [18], but in contrast with a study done in Nassarawa state [41] which revealed that females had a significantly higher co-infection rate than their male counterparts. Several studies have shown that male gender is associated with TB-HIV co-infection [25]. This association might further be explained by the X-chromosome susceptibility gene contributing to excess of males with TB in Some African populations as suggested by WHO [42].
Based on the finding of this study, there is likely that HIV and tuberculosis are diseases common among those with low socio economic status who cannot afford good nutrition, healthcare, and are vulnerable to all forms of sexual abuse, and poor living conditions including poor housing and overcrowding, which are known risk factors for developing both diseases. The low prevalence (18.7%) recorded among civil servants might be attributed to the fact that most of them are educated and enlightened as such they are aware of HIV/TB control and prevention techniques. In this study, subjects residing in the urban area had the highest prevalence of 42.7%. This is due to the fact that most urban dwellers engage in promiscuous activities, making them vulnerable to HIV and Tuberculosis.
5. Conclusion
The finding of this study revealed that the relevant prevalence of Tuberculosis among HIV sero-positive is 11.2%. The burden is higher among males than females and age category of 31-40 was found to be most infected. In this study, subjects residing in the urban area had the highest prevalence of when compared to rural dwellers. This moderately prevalence of Tuberculosis among HIV positive patients is of grave public health concern. Therefore, there is need to develop strategies to combat HIV/ Tuberculosis co-infection.
Acknowledgments
The author gratefully acknowledge the assistance of Dr. Marta Ballova, Ing. Konrad Balla, Livuska Ballova and Ing. Jozef Balla.
References
- Esgender M. Human Immunodeficiency Virus in the Developing World Advanced Virus Resistivity. 1999; 53:71-88
- Mahar D., Borgdoff M., Boerma T. HIV related Tuberculosis: How well are we doing with the current control efforts? Int J Tuberc Dis. 1999; 9: 17-24.
- Harries AD., Mbewe LNO., Salanifoni FML., Nyngulu DS., Randal JT., Nunn P., Tuberculosis Programme Changes and treatment outcomes in patient with smear positive pulmonary tuberculosis in Blantyre, Malawi. Lancet. 1996; 347:807-809
- Okonko IO, Soleye FA, Adeniyi FO. Okerentugba P.O. HIV and TB co-infection among patients on directly observed treatment of short course in Abeokuta, Ogun state, Nigeria. Nature and Science. 2012; 10(6): 10-14
- Chaisson RE, Martinson NA. Tuberculosis in Africa – Combating an HIV-Driver crises. The New England Journal of Medicine. 2008; 358 (11): 1089-1092.
- Baltussen R, Dye C, Floyd K. Cost effectiveness analysis of strategies for tuberculosis control in developing countries. Brit Med J. 2005; 10:1136.
- World Health Organization (WHO). Frequently asked questions about TB and HIV. [cited 2014 28th march]. Available from: www.whoint/tb/ hiv/faq.
- Iliyasu Z, Babashani M. Prevalence and prediction of TB co-infection among HIV seropostitive patients attending Aminu Kano Teaching Hospital, Northern Nigeria. J. Epid. 2009; 19(2): 81-87.
- Stop TB Partnership. Talking Points-TB/HIV. [updated 2007 June; cited 2014 28 March]. Avai lable from: www.stoptborg/ng/tbhiv/assessed documents/tbhivtalkingpoints.pdf.
- Devi SB, Naorem S, Singh TJ, Sing KB, Prasad L and Devi TS. HIV and TB Co-infection: A Study from RIMS Hospital Manipur. Journal, Indian Acad Clin Med, 2005; 6(3) 219-222.
- Venturini, Turkora A, Chiappini E, Gallli L, de Martino M, Thorne C. Tuberculosis and HIV co-infection in children. BMC Infectious Diseases. 2014; 14 suppl(1): S1-S5.
- World Health Organization (WHO). Global tuberculosis. [cited 2014 25 March]. Available from: http://apps.who.int/ iris/bitstream/ 10665/ 75938/1 /979241564502–eng.pdf.
- Global Report: UNAIDS report on the global AIDS, epidemic 2013. [cited 2014 28 March]. Available from: http://www.unaids.org/en/ media/unaids/contentassests/documents/epidem ic ology2013/gr2013/UNAIDS-Global-Report-2013- eng.pdf.
- De Riemer K, Kawamura LM, Hopewell PC and Daley CI. Quantitative Impact of HIV Infection on TB Dynamics. Am J Crit Care Med, 2007; 176(9):936-944
- Mims C, Dockrell HM, Goering RV, Roitt I, Wakelun D and Zuckerman M. Medical Microbiology, 3rd Edition. Edinburgh. Mosby Publishers Ltd. 2004; 660 p.
- Soon T and Alexandra ML. Haematological Aspects of HIV Syndrome. Williams Hematology (7th Edition) McGraw Hill, New York. Pp 1105-1108, 2006.
- Pennap GR, Makpa S and Ogbu S. Prevalence of HIV/AIDS among Tuberculosis Patients seen in a Rural Clinic in Nigeria. Trakia Journal of Sciences, 2011; 9(2): pp 40-44
- Anteyi EA, Idoko JA, Ukoli CO, Bello CS. Clinical pattern of human immunodeficiency virus infection (HIV) in pulmonary tuberculosis patients in Jos, Nigeria. Afr J Med Med Sci. 1996; 25(4):317–21.
- Onipede AO, Idigbe O, Ako-Nai AK, Omojola O, Oyelese AO, Aboderin AO, et al. Sero-prevalence of HIV antibodies in tuberculosis patients in Ile-Ife, Nigeria. East Afr Med J. 1999 Mar;76(3):127–32.
- Moses AE, Adelowo KA, Ajayi BB. Prevalence of HIV-1 infection among patients with leprosy and pulmonary tuberculosis in a semi-arid region, Nigeria. J R Soc Health. 2003; 123(2):117–9.
- Ige OM, Sogaolu OM, Ogunlade OA. Pattern of presentation of tuberculosis and the hospital prevalence of tuberculosis and HIVco-infection in University College Hospital, Ibadan: a review of five years (1998–2002). Afr J Med Med Sci. 2005; 34(4):329–33.
- Odaibo GN, Gboun MF, Ekanem EE, Gwarzo SN, Saliu I, Egbewunmi SA, et al. HIV infection among patients with pulmonary tuberculosis in Nigeria. Afr J Med Med Sci. 2006; 35 Suppl:93– 8.
- Tosi CH, Ngamgro MN, Djimadoum N, Richard V, Ngangro MN, Djimadoum N, et al. Study of HIV seroprevalence in patients with pulmonary tuberculosis in 1999 in Chad. Med Trop (Mars). 2002; 62(6):627–33.
- Range N, Magnussen P, Mugomela A, Malenganisho W, Changalucha J, Temu MM, et al. HIV and parasitic coinfections in tuberculosis patients: a cross-sectional study in Mwanza, Tanzania. Ann Trop Med Parasitol. 2007; 101(4):343–51.
- Bruchfeld J, Aderaye G, Palme IB, Bjorvatn B, Britton S, Feleke Y, et al. Evaluation of outpatients with suspected pulmonary tuberculosis in a high HIV prevalence setting in Ethiopia: clinical, diagnostic and epidemiological characteristics. Scand J Infect Dis. 2002; 34(5):331–7.
- Rao VG, Gopi PG, Bhat J, Yadav R, Selvakumar N., et al. Selected risk factors associated with pulmonary tuberculosis among Saharia tribe of Madhya Pradesh, Central India. Eur J. Public Health. 2009; 22:271-273
- Sterling TR, Lau B, Zhang J, Freeman A, Bosch RJ, et al. Risk factors for tuberculosis after highly active antiretroviral therapy initiation in the United states and Canada: Implications for tuberculosis screening. J. Infect Dis. 2011; 204:893-901.
- Agbaji O, Ebonyi AO, Meloni ST, Anejo-Okopi JA, Akanbi MO, et al. Factors associated with Pulmonary Tuberculosis – HIV co-infection in treatment – Naive Adults in Jos, North Central Nigeria. J. AIDS Clin. Res 2013; 4:222. Doi:10.4172/2155-61/3.1000222.
- Basset IV, Wang B, Chetty S, Giddy J, Losina E, et al. Intensive tuberculosis screening for HIV infected patients starting antiretroviral therapy in Durban South Africa. Clin Infect Dis. 2010; 51:823-829.
- National Population Commission (NPC). National population census result, 2006 Abuja Nigeria
- Yusuph H, Lailani SB and Ahedjo A. Prevalence of HIV in TB patients in Nguru, North Eastern Nigeria. Sahel Med J, 2005; 8(3): 65-67.
- Daniel OJ, Salako AA, Oluwole FA, Alausa OK and Oladapo OT. HIV seroprevalence among newly diagnosed adult PTB patients in Sagamu. Nigerian J Med, 2005; 13(4): 393-397.
- Nwobu GO, Okodua MA and Tatfeng YM. Comparative study of HIV Associated Pulmonary Tuberculosis in Chest Clinics from Two Regions of Edo State, Nigeria. Online J Hlth Allied Scs.2004;3:4 URL: http://www. ojhas. org/ issue 11/2004-3-4.htm
- Uche A and Alozie O. Emerging Prevalence of HIV among TB patients in Benin City, Nigeria. International Conference on AIDS. 2004, July 11-16; Abstract no. TUPeD5203, 2004.
- Moses AE, Adelowo KA.and Ajayi BB. Prevalence of HIV-1 infection among patients with Leprosy and Pulmonary Tuberculosis in a semi arid region, Nigeria. J R Soc Promot Hlth. 2003; 123(2): 117 – 119.
- Jemikalajah JD and Okogun GA, Health point prevalence of HIV and Pulmonary Tuberculosis among patients in various parts of Delta State, Nigeria. Saudi Med J. 2009; 30(3); 387-391.
- Kassu A, Mengistu G, Ayele B, Diro E, Mekonnen F, Ketema D, Moges F, Mesfin T, Getachew A, Ergicho B. Coinfection and clinical manifestations of tuberculosis in human immunodeficiency virus infected and uninfected adults at a teaching hospital, Northwest Ethiopia. J Microbiol Immunol Infect 2007, 40:116-22.
- Olaniran O, R E Hassan-Olajokun, MA Oyovwevotu RA and Agunlejika. Prevalence of Tuberculosis among HIV/AIDS Patients In Obafemi Awolowo University Teaching Hospital Complex Oauthc, ILE IFE. Int J Biol Med Res., 2011; 2(4): 874 -877
- Tadesse, S. and Tadesse, T. HIV co-infection among tuberculosis patients in Dabat, Northwest Ethiopia. J. Inf. Dis. Imm., 2013; 5(3):29-32
- Salami AK, Oluboyo PO. Hospital prevalence of pulmonary tuberculosis and infection with HIV in Ilorin. West Afr J of Med., 2002; 21(1):50-55
- Gyar SD, Dauda E and Reuben CR. Prevalence of Tuberculosis in HIV/AIDS Patients in Lafia, Central Nigeria Int. J.Curr. Microbiol. App.Sci (2014) 3(6) 831-838
- Global Tuberculosis Control: Surveillance, Planning, finance: WHO report 2008. WHO/HTM/TB/2008 .393.