Information
Journal Policies
ARC Journal of Hematology
Volume-1 Issue-1, 2016, Page No: 24-27
Hematological Malignancies of the Breast: Short Series of Cases and Discussion
S. Mitri, F.P. Duhoux, E. Van Den Neste, C. Galant, P. Saussoy, M. Berliere*
Clinique du Sein – Institut Roi Albert II, Avenue Hippocrate, 10, 1200 Brussels – Belgium
Citation : Khojasteh HN. Biology of Bonemetastasis and Clinical Medicine. ARC Journal of Hematology. 2016;1(1):18–23.
Copyright : © 2016 Khojasteh HN. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background: Haematological malignancies of the breast are a rare and heterogeneous entity.
Material and Methods: We are reporting a short series of four consecutive cases treated in our breast clinic. Therapeutic options are discussed. All the patients presented with a breast mass. The first case was finally considered as a follicular lymphoma (FL) and the differential diagnosis was made with a mucosa-associated lymphoid tissue (MALT) lymphoma. The patient only underwent a surgical biopsy to obtain the precise diagnosis. The second patient was diagnosed with a chronic lymphocytic leukemia with acutization and was treated with chlorambucil and rituximab. The third patient had a diffuse large B-cell lymphoma (DLBCL). She received no treatment because of her age and comorbidities. The fourth patient was diagnosed with a mixed phenotype acute leukemia (MPAL). Her treatment consisted of hyper-CVAD allograft and prophylactic irradiation of the central nervous system.
Results: The four patients are still alive.
Discussion and Conclusion: Except if the diagnosis is uncertain, surgery is not recommended in the therapeutic strategy. Chemotherapy combined with rituximab in selected cases, represents the best therapeutic option.
Keywords: Haematological Malignancies Of The Breast, Chemotherapy, Radiotherapy, Rituximab, Follicular Lymphoma, Lymphocytic Leukemia, Diffuse Large B Cell Lymphoma.
1.Introduction
Hematological malignancies of the breast (lymphomas and leukemias) are a rare entity, probably because of the paucity of lymphoid tissue in the breast as compared to other organs like the bowels and the lungs. Breast lymphomas can be subdivided into primary or secondary breast lymphomas. Primary breast lymphoma (PBL) has a reported incidence range of 0.04-0.5% among all breast malignancies and of less than 2 % of non-Hodgkin lymphomas (NHL). Secondary breast lymphoma is even less frequent, with a reported incidence of 0.07 % [1].
The diagnostic criteria for PBL were described by Wiseman and Liao in 1972 and are still in use today. PBL is defined as a lymphomatous infiltrate into breast tissue, without evidence of widespread lymphoma and with clinical occurrence in the breast. Ipsilateral involvement is allowed if it develops simultaneously with the primary breast tumor. Breast lymphomas are diagnosed by pathological findings because the clinical presentation and radiographic features of breast malignancies and carcinoma are similar. Multiple therapeutic options including surgery, chemotherapy and radiation have been tested in the treatment of breast lymphomas. The use of combined chemotherapy with immunotherapy followed or not by radiotherapy seems to be the optimal treatment choice for aggressive lymphomas [1-4].
We are presenting a small series of four consecutive breast hematological malignancies diagnosed in our breast clinic. This study has been approved by our local ethics committee (2016/416).
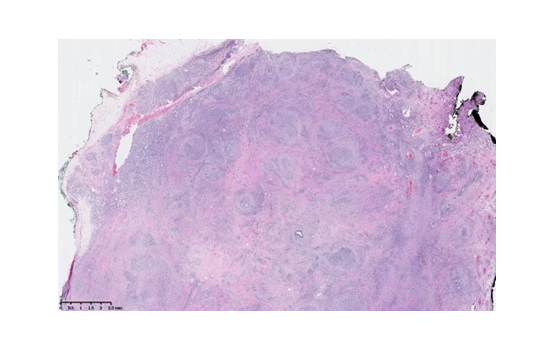
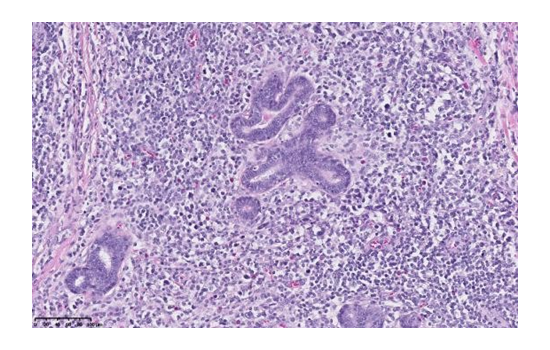
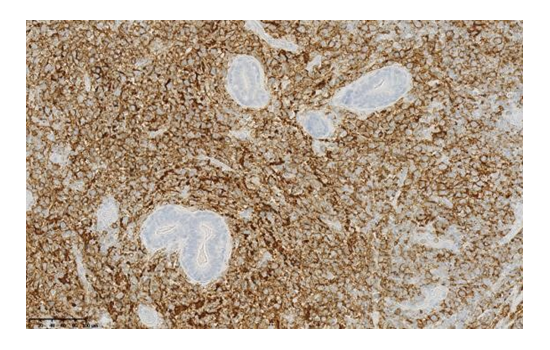
A 32-year-old woman self-palpated a painless lump in her left breast. The mammogram demonstrated a homogeneous increased tissue density in the left breast. A mass of 50 mm was found by ultrasonography. Magnetic resonance imaging (MRI) confirmed this mass of 59 mm as well as one suspect axillary lymph node. The biopsy was compatible with a mucosa-associated lymphoid tissue (MALT) but the diagnosis remained uncertain. The immunophenotype of the cells was CD3-, CD20+ and CD10-. The CT-scan and the PET-scan showed no evidence of disease dissemination. The patient presented no general symptoms. She underwent a tumorectomy in order to obtain a complete prognostic and genetic analysis of the tumor. The histological analysis showed a low grade follicular lymphoma (Figures 1, 2 and 3).
The molecular karyotype was complex with numerous genomic imbalances, mainly deletions recurring in mature B-cell lymphoma but not specific. However, the 1p36 deletion is described in follicular lymphomas, most of the time without BCL2 rearrangement. It was decided not to administer any adjuvant treatment because the resection was complete. The MRI after twenty months showed no recurrence in the breast. There was also no biological sign of relapse.
An 84-year-old woman was admitted to the hospital with a right axillary mass. The patient complained of asthenia and nocturnal sweating. Blood tests were performed and showed an increased lymphocyte count, increased lactate dehydrogenase (LDH) levels and an increased lymphocyte count by monoclonal CD5+, CD23+, CD20+, CD200+ B cells for which the Matutes-Catosky scoring was 3 out of 5. A biopsy of the axillary lymph node revealed a lymphomatous deposit of a chronic lymphocytic leukemia without any signs of transformation. The cytogenetic analysis showed a 14q deletion. The PET-CT demonstrated multiple hypermetabolic lymph nodes and an oversized spleen. After 5 months, blood tests revealed a doubling of the lymphocytosis. The patient started cytostatic treatment with chlorambucil and rituximab. The breast mass quickly disappeared after the initiation of chemotherapy.
An 86-year-old woman had a surgical resection of a small right supra-mammary subcutaneous mass in 2012. The histological analysis showed a BCL2+ follicular lymphoma which could either be primitive or secondary. Proliferation index Ki67 was high. The genetics analysis showed an amplification of the MALLT1 and BCL2 loci on 18q21 but no rearrangement. The LDH levels and the complete blood count were normal. In January 2014, a lump reappeared in the scar and the biopsy showed a cutaneous infiltration by a follicular lymphoma.
In September 2014, the patient self-palpated a mass in the superior quadrant of her right breast. The ultrasonography and the mammogram demonstrated a condensation of the glandular tissue measuring 25x20x18mm in her right breast. A biopsy was performed. The histopathological and immunohistochemical findings allowed for the diagnosis of a diffuse large B-cell lymphoma (DLBCL) with positive CD10, CD20, BCL2, BCL6 and C-myc. The patient had no B symptoms and the LDH levels were normal. The final diagnosis was thus a transformed diffuse large B-cell lymphoma (DLBCL) emanating from a recurring subcutaneous follicular lymphoma. The patient was not prescribed any cytotoxic treatment because she had no general symptoms and a treatment could have worsened her physical condition. The breast mass remained unchanged after 12 months of follow up.
A 41-year-old woman presented with a hard mass of approximately 15 mm in her right breast. The biopsy showed little cells compatible with a lymphoma or a lobular carcinoma.
The immunohistochemical findings showed negative E-cadherin, CD20 and CD3 and negative hormonal receptors.
Careful interrogation of the patient revealed that she had been complaining about lower back pain for a few months. The CT and the PET-scan showed a tissue infiltration in the eleventh thoracic vertebra of the spine. The biological analyses revealed a hyperleucocytosis with blast cells. LDH levels were also increased. The bone marrow aspirate was consistent with a mixed phenotype acute leukemia (MPAL). In fact, the immunophenotyping by flow cytometry showed CD34+ Tdt+ HLADR+ blast cells with a co-expression of myeloid (MPO and CD33) and lymphoid (CD79a, CD19 and CD10) markers. This mixed phenotype was confirmed by immunohistochemistry. Cytogenetic findings showed an abnormal cellular clone harboring the t(9;22)(q34;q11.2) translocation and molecular biology confirmed the presence of a p210 BCR-ABL1 fusion gene by Rtq-PCR. The patient was thus diagnosed with chronic myeloid leukemia transforming into a Phi+ MPAL. She received a treatment consisting of 3 cycles of Hyper-CVAD chemotherapy (cyclophosphamide, vincristine, doxorubicin and dexamethasone) with central nervous system (CNS) prophylaxis, as well as a consolidation by allograft after an intensification by cyclophosphamide and total body irradiation. One month after the allograft complete chimerism was observed, however with a persisting BCR-ABL fusion gene.
Treatment with dasatinib was started one month later because the BCR-ABL1 fusion gene could still be detected. The patient eventually went into molecular remission of 4.5 because the BCR-ABL1 fusion gene could still be detected and is still taking dasatinib with no signs of graft-versus-host- disease.
2. Discussion
Although the incidence of breast lymphoma varies between studies, it is clear that PBL is a rare subtype of extra-nodal lymphoma. Secondary breast lymphomas are less well represented in the literature and often included in articles on PBL. Breast lymphomas usually present clinically as a unilateral, mobile, painless mass, which grows rapidly. B-symptoms are rare [1]. Most studies have reported a predilection for involvement of the right breast, as in our cases, but VE.Duncan et al. reported the opposite. The more common prognostic factors are stage and histological grade.
Although all histological subtypes of lymphoma have been described in the breast, 80% of breast lymphomas are CD20+ B-cell lymphomas. The most prevalent subtype is DLBCL (50%) for primary as well as for secondary cases; follicular lymphomas (FL) account for 15 % and MALT lymphomas account for 12% of malignant lymphomas of the breast. The two most frequent histological subtypes of breast lymphoma are represented among the four cases referred to in this paper, namely DLBCL and FL.
Singh et al. reported one case of acute myeloid leukemia when he studied the importance of fine needle aspiration cytology in diagnosing breast lymphoma. However, no case of chronic myeloid leukemia or MPAL in the breast is described in the literature. VE Dunkan et al. [1] described one case of small lymphocytic lymphoma. We also found some reports of the combination of lymphoma with a metastatic breast cancer in axillary lymph nodes. The synchronous malignancies reported in the breast include small lymphocytic lymphoma and acute myeloid leukemia.
Since 1990, the use of surgical resection in the management of breast lymphoma has declined [5]. William et al. reviewed all published cases of PBL from 1972 to 2005 and they concluded that mastectomy offers no benefit in the treatment of PBL: there was no benefit in survival or recurrence risk when the treatment included a mastectomy. Surgery should be limited to a biopsy to establish a histological diagnosis. MALT lymphoma or uncertain diagnosis are the only exceptions [3].
In most reports, patients with aggressive lymphomas have received chemotherapy. Anthracycline- based chemotherapy (CHOP, i.e. cyclophosphamide, doxorubicin, vincristine,and prednisone) with rituximab is currently the best treatment option for DLBCL, in combination or not with radiotherapy. Rituximab improves the response rate, disease -free and overall survival in patients with DLBCL [6]. Caon et al. [2] reported an increase in the five-year overall survival rate from 49% to 78 % for patients with aggressive lymphoma whose treatment included rituximab. The place of radiotherapy is discussed according to the response to chemotherapy and included in the therapeutical strategy according to the criteria of the MINt study [7].
In our series, case 1 was finally considered as a FL and the patient was treated by surgery: adjuvant therapy was not considered necessary and there was no relapse observed after 20 months. The second case was a chronic lymphocytic leukemia with acutization and the patient received chemotherapy with rituximab. Our only case of DLBCL (case 3) was not very aggressive, and no treatment was given, as it could have worsened the physical condition of the elderly patient who was 86-year old. The patient with MPAL (case 4) was treated with hyper-CVAD chemotherapy with CNS prophylaxis, as well as a consolidation by allograft.
The central nervous system is the most frequent site of distant relapse with a rate varying between 3 and 27 % in the literature. CNS prophylaxis is controversial in patients with breast lymphoma [l]. Caon et al. [2], in their retrospective sudy, described no CNS relapse in the patients who received rituximab. This could reflect the improved rate of control of the lymphoma with this treatment. There is more risk of CNS recurrence in patients with high LDH levels and more than one extranodal involvement and in patients with MPAL.
3. Conclusion
Hematological malignancies of the breast are a rare heterogenous entity. The most frequent histopathologic subtype is DLBCL. Combined therapy is the standard treatment for patients with PBL. The most frequent chemotherapy regimen includes CHOP with rituximab. Except for rare cases of MALT lymphomas or uncertain diagnosis after biopsy, surgery is not recommended because it offers no benefit in survival or recurrence risk and because accurate diagnosis is generally possible using micro- and macrobiopsies.
References
- Duncan VE, Reddy V, Jhala NC, Chienq DC, Jhala DC. Non-Hodgkin lymphoma of the breast: a review of 18 primary and secondary cases. Annals of Diagnostic Pathology 2006; 10:144-8.
- Caon J, Wai ES, Hart J, Alexander C, Truong PT, Sehn LH, Connors JM. Treatment and outcomes of primary breast lymphoma. Clinical Breast Cancer 2012; 12: pp 412-9.
- Mastuda I, Watanabe T, Enomoto Y, Takatsuka Y, Mihoshi Y, Hirota S. Spontaneous regression of primary extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue colliding with invasive ductal carcinoma of breast: a case report. Int J Clin Exp Pathol. 2014; Sep. 157(10): pp 7020-7.
- Aviles A, Castadena C, Neri N , Cleto S, Nambo J.. Rituximab and dose dense chemotherapy in primary breast lymphoma. Haematologica 2007; 92: pp 1147-8.
- Mouna B, SaberB, Tijani El H, Hind M, Amina T, Hassan E.. Primary malignant non-hodgkin's lymphoma of the breast: a study of seven cases and literature review. World Journal of Surgical Oncology 2012; 10: pp 151.
- Coiffier B, Lepage E, Brière J, Herbrecht R, Tilly H, Bouabdallah R et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large -B-cell lymphoma. N Engl J Med. 2002; Jan 24; 346(4): pp 235-42.
- Pfreundschuch M, Kuhnt E,Trumper L,Osterborg A , Timeny M, Sheperdd L et al. CHOP-like chemotherapy plus rituximab versus CHOP-like chemotherapy alone in young patients with good-prognosis diffuse large B-cell lymphoma:6-year results of an open -label randomised study of the :Mab Thera International Trial(MINt) Group. Lancet oncol 2011; 12(11): pp 1013-22.