Information
Journal Policies
Acromegaly: Ominous Cause of Polycystic Ovary Syndrome
Manel jemel Hadiji1*, Mahdi Kalthoum2, Hajer Kandara3, Wafa Mimita4, Sonia Nagi5, Ines Kamoun6
2.Dr, National Institute of Nutrition and Food Technology Department of Endocrinology Tunis Tunisia.
3.MD, National Institute of Nutrition and Food Technology Department of Endocrinology Tunis Tunisia, Manar University Tunis Tunisia.
4.Dr, National Institute of Nutrition and Food Technology Department of Endocrinology Tunis Tunisia.
5.Pr, National Institute of Neurology Department of Neuroradiology Tunis Tunisia, Manar University Tunis Tunisia.
6.Pr, National Institute of Nutrition and Food Technology Department of Endocrinology Tunis Tunisia, Manar University Tunis Tunisia.
Copyright : © 2019 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Hirsutism though common in women of reproductive age, is classically associated with polycystic ovarian syndrome (PCOS). It is rarely seen as a prominent feature of acromegaly because of its lack of specificity and occurrence. We report a case of 28-year-old female with 3 year duration of aligoamenorrhea and hirsutism. She was followed by a gynecologist who retains the diagnosis of polycystic ovary syndrome (PCOS). After 5 years the patient complaints of increased hand finger and shoes size. She was referred to endocrine department for suspicion of Acromegaly. Clinical examination revealed acromegaloidism features with mandibular prognathism and moderate macroglossia wic. Biological investigation were significant for elevated insulin-like growth factor 1 (IGF-1) level (774 ng/ml normal: 98-290 ng/ml) and a growth hormone level not suppressed by a glucose challenge test. MRI brain revealed a pituitary macroadenoma (10.7x14 mm). The patient underwent an uncomplicated trans-sphenoidal resection of a pituitary macroadenoma. Immunohistochemistry demonstrated a GH tumor. The patient subsequently had normalization of growth hormone dynamics and regular menstrual cycles. Our case highlights the importance of a lookout for subtle features of acromegaly in patients with hirsuitism and going for hormonal investigation to make the diagnosis of acromegaly at an earlier stage of the disease.
growth hormone, hirsutism, polycystic ovarian syndrome, pituitary adenoma
1. Introduction
Hirsutism is among the most frequent medical complaints among women in reproductive age effecting 5-7% of the female population. It has a variety of etiologies, although it is most commonly associated with polycystic ovary syndrome (PCOS) [1]. However in rare cases, hirsutism may be the initial presentation of a more serious disorder like Cushing’s syndrome, adrenal or ovarian tumours, or acromegaly. Acromegaly is caused by chronic hypersecretion of growth hormone (GH) and insulin-like growth factor 1 (IGF-1) (2). Diagnosis of acromegaly in advanced stage is easy once the patient has developed disfiguring skeletal with signs of chronic acral overgrowth, such as frontal bossing, mandibular prognathism, and increased hand and shoe size (3,4). However diagnosis remains a challenge when the patient may have only subtle features of insulin resistance and PCOS in women, as only 1.1% of patients in a large retrospective review reported that it was the earliest sign of their disease (3).
This case describes a patient who presented with a clinical picture of chronic hirsutism secondary to a GH-secreting pituitary adenoma.
2. Case Report
A 28-year-old female presented to the Endocrinology department with complaints of longstanding complaints of increased facial hair, body hair and menstrual irregularities. She was not married and had no past medical history, medications, or significant family history. Menarche occurred at the age of 13, with progressive hair growth on her face and body after puberty necessitating shaving once to twice a week. More recently she complained of weight gain, increased sweating and increased hand finger and shoe size. There was no history of headache or vision abnormalities.
Physical examination revealed an overweight female 170 cm tall and weighing 84 kg (BMI 29.06 kg/m2) with hirsuitism (modified Ferriman Gallwey Score >8) and normal blood pressure. The patient was diagnosed with PCOS based on oligomenorrhea and hirsutism. Ultrasonography abdomen revealed enlarged bilateral ovaries, presence of multiple follicles. After 5 years the patient complaints of increased hand finger and shoes size. She was referred to endocrine department for suspicion of Acromegaly. She had the clinical appearance of acromegaly: bulbous lips, mandibular prognathism, macroglossia and enlarged nose.
The total testosterone, DHEAS were all within normal limits. Age adjusted, insulin-like growth factor-1 (IGF-1) was elevated at 774 ng/ml (normal: 98-290 ng/ml). A subsequent glucose tolerance test demonstrated a non suppressible growth hormone level, with a basal (9.29 ng/ml) and post glucose GH (5.59 ng/ml).
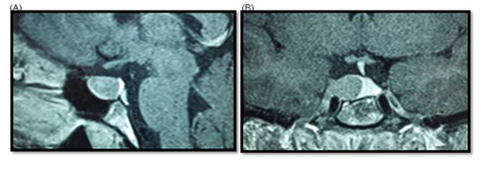
Brain magnetic resonance imaging (MRI) showed hyposignal WT2 pituitary macroadenoma (10.7 x 14 mm) with suprasell extension and no compression of the optic chiasm (Figure1). The patient underwent an uncomplicated trans-sphenoidal resection of a pituitary macroadenoma. Immunohistochemistry demonstrated a GH tumor. The patient subsequently had normalization of growth hormone dynamics and regular menstrual cycles.
3. Discussion
PCOS characterized by hyperandrogenic anovulation, is the most common metabolic abnormality in reproductive-aged women [1]. The Rotterdam consensus conference developed the following diagnostic criteria for PCOS: Diagnosis required the presence of 2 of these 3 findings: irregular cycles, clinical or biochemical evidence of hyperandrogenism, and multicystic-appearing ovaries on ultrasound, as well as no other underlying endocrine disorder. In our patient PCOS was diagnosed in view of clinical hyperandrogenism and menstrual irregularities. PCOS can be idiopathic or associated with other sever diseases such as acromegaly: in a series of patients with acromegaly, PCOS was found in up to 50% of patients [5].
Acromegaly is a rare disorder (estimated prevalence of 30 cases/ million). In 95% of cases acromegaly is due to a GH secreting pituitary adenoma [6]. and is associated with 2 to 5 fold increased in mortality as compared to the general population mainly due to the cardiovascular and respiratory consequences of the condition and less commonly due to the increased malignancy rate [4]. The diagnosis of acromegaly is often delayed due to the slow progression and absence of early clinical features. Acromegaly can be associated with hirsutism (24%) and hyperandrogenism although they are rarely the initial presentation of the disease [5]. There are five reported cases of PCOS associated with active acromegaly identified in our search of the literature (7-10). Each of these cases presented with severe hirsutism, and only three of five had menstrual irregularities. Four of five of the cases had polycystic ovaries on ultrasound and one had normal pelvic ultrasound (7-10).
The cause of hirsutism in acromegaly is not well known. In acromegaly, chronic elevated growth hormone levels result in elevated total and free IGF-1. Patients with acromegaly are often insulin resistant due to the insulin-antagonistic effects of elevated circulating growth hormone. GH directly and indirectly through increased IGF-1 is believed to increase ovarian androgen production which may have a role in the development of hirsuitism [11]. Moreover GH decreases sex hormone binding globulin levels, which leads to increased free testosterone levels in patients of acromegaly despite a normal testosterone levels [11].
The importance of this case is to highlight that hirsutism may rarely be the only prominent symptom of acromegaly. A lookout for subtle manifestations of acromegaly in patients with hirsutism may help us in diagnosing acromegaly at an earlier stage of the disease and avoiding its fatal complications.
4. Conclusion
In conclusion, we report a case of acromegaly due to a pituitary macroadenoma presenting with signs of severe hirsutism. This case highlights the need to consider acromegaly as part of the differential diagnosis of hirsutism before diagnosing relatively common PCOS. The similarity between PCOS and other endocrine diseases reinforces the importance of ruling out underlying endocrine abnormalities in patients with chronic hyperandrogenic clinical picture. Acromegaly is a sever life threatening disease and early diagnosis is crucial for reducing its associated morbidity and mortality.
References
- Azziz R, Sanchez LA, Knochenhauer ES, Moran C, Lazenby J, Stephens KC, et al. Androgen excess in women: Experience with over 1000 consecutive patients. J Clin Endocrinol Metab 2004;89:453-62.
- Melmed S, Braunstein GD, Horvath E, Ezrin C, Kovacs K. Pathophysiology of acromegaly. Endocr Rev. 1983;4:271-290.
- Reid TJ, Post KD, Bruce JN, Nabi Kanibir M, Reyes-Vidal CM, Freda PU. Features at diagnosis of 324 patients with acromegaly did not change from 1981 to 2006: acromegaly remains under-recognized and under-diagnosed. Clin Endocrinol (Oxf). 2010;72:203-208.
- Dineen R, Stewart PM, Sherlock M. Acromegaly. QJM. 2017;110:411-420.
- Kaltsas GA, Androulakis II, Tziveriotis K, Papadogias D, Tsikini A, Makras P, et al. Polycystic ovaries and the polycystic ovary syndrome phenotype in women with active acromegaly. Clin Endocrinol (Oxf) 2007;67:917-22.
- Duncan E, Wass JAH. Investigation protocol: acromegaly and its investigation. Clin Endocrinol (Oxf). 1999;50:285–293.
- Unal A, Sahin Y, Keleştimur F. Acromegaly with polycystic ovaries, hyperandrogenism, hirsutism, insulin resistance and acanthosis nigricans: a case report. Endocr J. 1993;40:207-211.
- Abdo S, Samaras K. Hair, sweat and tears. BMJ Case Rep. 2011;2011.
- Jain R, Dutta D, Shivaprasad K, et al. Acromegaly presenting as hirsuitism: Uncommon sinister aetiology of a common clinical sign. Indian J Endocrinol Metab. 2012;16(suppl 2):S297-S299.
- Ha D, Vinales KL. A hairy case: acromegaly presenting as hirsutism. Endocrine Society’s 97th Annual Meeting and Expo, March 5–8, 2015, San Diego, CA. Presentation Number: THR-420. Available at: http://press.endocrine. org/doi/abs/10.1210/endomeetings.2015. NP.2. THR-420#sthash.2nOnQJl3.dpuf. Accessed November 22, 2017.
- Kaltsas GA, Mukherjee JJ, Jenkins PJ, Satta MA, Islam N, Monson JP, et al. Menstrual irregularity in women with acromegaly. J Clin Endocrinol Metab 1999;84:2731-5.