Information
Journal Policies
Determinants of Cervical Cancer Screening Uptake among Female Medical Students at the Copperbelt University, Micheal Chilufya Sata School of Medicine, Zambia
Kabelenga Elijah1,2*, Mwanakasale Victor1, Siziya Seter1
2.Ndola College of Nursing and Midwifery, Private Agency, Ndola 10101, Zambia.
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
In Zambia, cervical cancer screening is offered to any woman aged between 25 and 49 years for free at many public health facilities countrywide. However, no study has been conducted on determinants of cervical cancer screening uptake among medical students in public universities. The aim of this study was to examine determinants of cervical cancer screening uptake among female medical students at the Copperbelt University, Micheal Chilufya Sata School of Medicine (MCS-SOM). This was a cross sectional study in which 72 female medical students at the Copperbelt University, MCS-SOM were recruited. Variables that were statistically significantly associated with the outcome in bivariate analyses were considered in a logistic multivariate regression analysis. Only 22 (30.6%) participants were screened for cervical cancer. In bivariate analysis, determinants of cervical cancer screening uptake were marital status, Gravidity, unprotected vaginal sex and attitude. In logistic multivariate analysis, only students who have been pregnant before were 3.3 times (AOR=3.27; 95% CI [1.654, 6.461]) more likely to be screened compared to those who have never been. Our study has demonstrated that gravidity was the only determinant of cervical cancer screening uptake among female medical students. We recommend further studies in this area by giving emphasis on its correlates.
Cervical cancer screening, Determinants, Gravidity, Uptake,Clinical Case Reports
1. Introduction
Cervical cancer is a public health concern that is causing high morbidity and mortality among woman. Globally, it is the second most common cancer in women [1]. Although not in itself a sexually transmitted infection, cervical cancer is highly linked to preventable human papilloma virus (HPV) type 16 and 18 which is sexually transmitted [2]. In 2014, World Health Organisation (WHO) estimated that 70% of all cervical cancer cases reported throughout the world are caused by only HPV types 16 and 18 [3]. An estimated 70,000 new cervical cancer cases occur annually in sub-Saharan Africa, the majority (10) of these African countries are found in the Southern African development Community (SADC) [1,3,4]. In 2014, Zambia was ranked 4th globally and 3rd in Africa from 6th in 2002 with cervical cancer burdern [4,5].The country also ranks cervical cancer the first most common cancers among women aged 15 and 44 years. Yearly an estimated 2, 330 Zambian women are diagnosed with cervical cancer and 1, 380 die from the disease [6,7].
Many factors have been found to predispose to cervical cancer in Zambia. These include HPV type 16 and 18 with the prevalence among women estimated at 68.8 %, smoking, number of sex life partners, parity, fertility rate, HIV infections, insertion of herbs in vagina, genetic predisposition and early engagement in penetrative sexual activity [2,8,9].
Cervical pre-cancer goes through many stages before it becomes cancer. It becomes cancer when the abnormal cells spread below the epithelial layer down into the deeper tissues (stroma) of the cervix, a process called invasion [2]. Cervical cancer screening is the process of detection of precancerous cervical lesions in otherwise healthy women before the lesions develop into cancer [2,6]. These precancerous lesions can be treated easily or removed to stop cervical cancer from developing. Because these precancerous lesions take many years to develop into cervical cancer, even periodic screening can detect almost all lesions before they progress to cancer [2]. According to WHO 2014 guidelines on screening and treatment of cervical cancer, screening is aimed at all females in the target age group, followed by treatment of detected precancerous lesions so that the majority of cervical cancers are prevented. WHO further recommend that at least one cervical cancer screening be performed on any female who is 30 to 49 years old. However, this can be extended to females younger than 30 years provided there is evidence of a high risk for CIN [6]. In Zambia, any women aged between 25 and 49 years are supposed to undergo cervical cancer screening every after 3 to 5 years [2]. Cervical cancer screening tests are available globally and differ according to the available resources and government recommendations. The screen and treat is one simplified approach that has been developed and accepted by WHO. It uses visual inspection with acetic acid (VIA) and immediate cryotherapy for secondary prevention of cervical cancer. This approach has been adopted and is now being used in countries with limited resources such as Zambia [12,13]. Visual cervical screening is a method where there is visual inspection of cervical epithelium with acetic acid (VIA). It is a simple screening procedure that is performed by a nurse [4]. In Zambia, the Cervical Cancer Prevention Program in Zambia (CCPPZ) was started in 2006. It introduced and scaled-up screening for cervical cancer using the single-visit approach of screening women with VIA and treating eligible lesions with cryotherapy.
The government of Zambia through Ministry of Health has put in efforts to minimize cervical cancer morbidity and mortality by rolling out free cervical cancer screening to many public health facilities countrywide. However, according to our knowledge no study has been conducted on determinants cervical cancer screening uptake among medical students in public univeristies in Zambia. The aim of this study was to examine determinants of cervical cancer screening uptake among female medical students at The Copperbelt Univeristy, Micheal Chilufya Sata School of Medicne in Ndola district, Zambia.
2. Methodology
A cross sectional study was conducted among female medical students at the Copperbelt University, Ndola Campus from May to July, 2017. Simple random sampling technique with help of random sampling table was utilised to select a total of 72 female medical students of the Copperbelt University, Micheal Chilufya Sata School of Medicine using a standardised pre tested questionnaire that focused on selected determinats of cervical cancer screening age, marital status and gravid, cervical cancer risk factors (unprotected sex, sex debut, male partner cirmcision, condom use), knowledge level of risk factors, signs and symptoms and preventive measures as well as attitude towards screening. Sample size was calculated using a formula by Yamane [14]. Only female medical students in clinical years were included in the study. Preclinical students and those who had deferred their studies to later years were excluded. Ethical clearance to conduct the study was sought and granted from Tropical Diseases Research Centre (TDRC) Ethics Committee IRB Registration Number: 00002911 and FWA Number: 00003729. Permission to conduct the study among female medical students was sought from The Dean of students, Copperbelt University. The study did not pose any risk to the participants and confidentiality was maintained. Informed consent was obtained from participants before being enrolled into the study. Data collection tools were viewed only by approved research personnel. The questionnaires were numbered first. Responses to open questions in the questionnaires were coded before being entered into Microsoft Excel and analysed using SPSS version 21 statistical software. Proportions of various variables were compared using Chi square test and only results yielding a p-value of less than 0.05 (p=0.05) were considered to be of statistical significant. Variables that were statistically significantly associated with the outcome in bivariate analyses were considered in a logistic multivariate regression analyses using a backward variable selection method. Adjusted odds ratio (AOR) with its 95% confidence intervals (CI) is reported.
3. Results
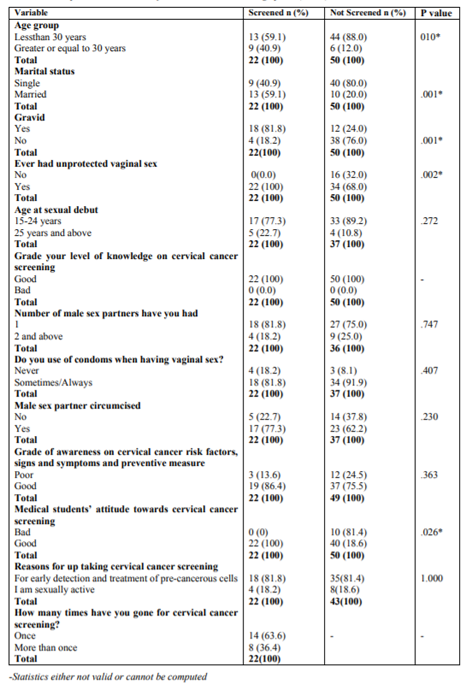
A total of 76 participants were enrolled but only 72 completed the questionnaire at a response rate of 94.7%. Table 1 summarises determinants of participants of cervical cancer screening uptake. The majority (79.2%) of the participants were below 30 of years. Sixty eight percent were single. Out of 72 participants, 22 (30.6%) undertook cervical cancer screening and 14 of the 22 had gone for screening only once.
Participants in the aged 30 years or less were more likely not to be screened compared to those aged 30 years or older (p=.010). Single participants were more likely not to be screened compared with married participants (p=0.001). Participants who had been pregnant before were more likely to be screened compared to participants who had never been pregnant before (p=0.001). All the study participants had good knowledge on cervical cancer screening services. Females students who had never had unprotected vaginal sex were less likely to have been screened compared to those who had unprotected vaginal sex (P=0.002). Most (84.7%) of the particpants were aged below 25 year when they first had their first sexual intercourse. About 3 in 4 (77.6%) of the participants had 1 male sex partner. Condoms were never used by 11.9% of the participants. About two thirds (67.8%) of the participants had male sex partners who were circumcised. Overall, 78.9% of the participants had good grade of awareness on cervical cancer risk factors, signs and symptoms and preventive measures. In addition, most (81.5%) of the participants stated early detection and treatment of pre-cancerous cells as the reason for undergoing vervical cancer screening. Medical students who had bad attitude towards cervical cancer screening were more likely not to be screened compared to those who had good attitude (p=0.026).
The results of multivarient analysis showed that after adjusting for unproted vaginal sex and attitude, only gravidity remained significant predictor of cervical cancer screening uptake. Students who have been pregnant before were 3.3 times (AOR 3.27, 95% CI: [1.654, 6.461]) more likely to be screened compared to those who have never been.
4. Discussion
Cervical cancer screening tests are available globally and differ according to the available resources and government recommendations. The screen and treat using visual inspection with acetic acid (VIA) is one simplified approach and accepted by WHO and currently adopted in Zambia [12,13].
In contextualizing the study its worthy to note that the participants were female undergraduate medical students in their clinical years. The greater proportion of the participants (59; 82%) fell within 20-29 years. This finding is consistent with the findings in the Zambia Demographic and Health Survey (ZDHS) of 2013 -2014 which found that a total of 13.9% of the Zambian population are females aged 20-29 years [15]. This finding is similar to what was found in a similar study conducted in Ilorin, North Central Nigeria [16] and in a study conducted among Female University Students from 25 Low, Middle Income and Emerging Economy Countries [17]. This finding is also consistent with findings of similar studies that were conducted on similar topics among university female students in South Africa and Mizan Tepi University, Ethiopia 2016 [18,19]. This age structure shows that the sample consisted young population which could have higher fertility and calls for provision of reproductive health services to meet their sexual and reproductive health needs.
However despite many factors being cited as indicators for seeking cervical cancer screening by many writers [2,9,10], this study has demonstated that only gravidity triggered partcipants to go for cervical cancer screening. This finding is similar to what was found in a similar study by Mbewe in Katete district of Zambia where women who had been pregnant before went for cervical cancer screening than those who have never been [9]. In addition, in a population-based study on the risk of cervical cancer and cervical intraepithelial neoplasia among grand multiparous women in Finland by Hinkula and others found an increased incidence of Cervical cancer (CC) and cervical intraepithelial neoplasia (CIN) among young multigravida women to have causal association to HPV 16 than those who have never been pregnant before [20]. Similary, in a study by Louie et al in 2009 found age at first pregnacy highly interrelated and had similar invasive cervical carcinoma (ICC) risk estimates [21]. In a similar study in 2014 by Wongwatcharanukul and his colleagues on factors affecting cervical cancer screening uptake by Hmong Hill tribe women in Thailand found previous pregnancy as one of the perceived risks of developing cervical cancer among women who went for cervical cancer screening[22]. Furthermore, the International Agency for Research on Cancer (IARC) has cited that early childbearing is a risk factor for cervical carcinogenesis because of the cervical trauma experienced during early age at first pregnancy (AFP) and subsequent high-parity births [23]. This view is also supported by American cancer Society on the causes, treatment and prevention of cervical cancer and other publications by other writers including WHO [2,4,24]. The current finding could be attributed to the knowledge held by such students were they associate unprotected vaginal sex to HPV 16 and 18 virus exposure and trauma experienced during delivery, which are viewed as risk factors to cervical cancer development. This could have facilited positive attitudes in the participants hence going for screening.
5. Limitation Of The Study
Gravidity was adjusted for the other two variables, unprotected vaginal sex and positive attitude maybe because of the problem of small sample size.
6. Conclusion And Recommendation
Interestingly this study has shown that despite partcipants’s good awrenessness and attitude towards cervical cancer screening, only gravidity was the only determinant for free cervical cancer screening uptake. We recommend researchers to do further studies in this area by giving emphasis on its correlates.
References
- Chitashi, NS. Quality of life in Zambian cervical cancer women post chemo-radiology. South Africa: University of Johannesburg (Unpublished masters dissertation). Pp. 22 (2012)
- Parham GP, Mwanahamuntu, MH & Hicks, LM.). A Manual for Physicians, Nurse Practitioners, and Managers: Custom Publication of the African Centre of Excellence for Women’s Cancer Control. 2nd edition. Zambia: Lusaka. Pp. 42 – 44. (2014).
- WHO. Comprehensive cervical cancer control, A guide to essential practice. WHO: Geneva 2014. (20/02/16).
- Parham GP, Mwanahamuntu MH, Kapambwe S et al. Population-Level Scale-Up of Cervical Cancer Prevention Services in a Low-Resource Setting: Development, Implementation, and Evaluation of the Cervical Cancer Prevention Program in Zambia. PLOS one 2015; 1-19.
- Southern Africa Litigation Centre (SALC). Tackling Cervical Cancer: Improving Access to Cervical Cancer Services for Women in Southern Africa. Southern Africa Litigation Centre. http://www.southernafricalitigationcentre.org/w p-content/uploads/2017/08/CERVICAL-CANCER-Report1.pdf 2012. 8 (9). (25/01/ 2016).
- Afri dev. Info. Africa Cervical Cancer Multi Indicator Incidence & Mortality Scorecard. Information & Analysis on Health, Population, Human & Social Development 2014. (25/01/2016).
- Institut Català d’Oncologia (ICO). ICO Information Centre on HPV and Cancer - HPV Information Centre. Spain: Barcelona 2017. (20/02/16).
- Zambian Cancer Society. Cancer in Zambia. http://www.zambiancancersociety.org 2015. (20/01/16).
- Mbewe, A. A study to determine women's knowledge and practices towards cervical cancer at St. Francis hospital in Katete. Lusaka: Ridgeway campus. http://dspace.unza.zm:80 80/xmlui/handle/123456789/3810 2008. (21/01/ 2016).
- Parham GP. Cervical Cancer Prevention Program in Zambia. Lusaka: CIDRZ/UAB 2012. (20/02/2016).
- Cervical Cancer Prevention Program in Zambia (CCPPZ). Free Cervical Cancer Screening Clinics are located in every Zambian Province. http://www.acewcc.org 2015. (21/01/2016).
- WHO. Guidelines for screening and treatment of precancerous lesions for cervical cancer prevention. WHO: Geneva 2013.
- Mwanahamuntu MH, Sahasrabuddhe VV, Blevins M,et al. Utilization of Cervical Cancer Screening Services and Trends in Screening Positivity Rates in a ‘Screen-And- Treat’ Program Integrated with HIV/AIDS Care in Zambia. PLoS ONE 2013; 8 (9).
- Yamane T. Statistics, An Introductory Analysis, 2nd Ed. New York: Harper and Row (1967).
- Zambia Demographic and Health survey (ZDHS) 2013 - 2014. House hold population by Age and sex. Lusaka: Zambia 2015.
- Idowu A, Olowookere,SAFagbemi, AT et al. Determinants of Cervical Cancer Screening Uptake among Women in Ilorin, North Central Nigeria: A Community-Based Study. Journal of Cancer Epidemiology 2015; 2016:1-8.
- Pengpid S & Peltzer K. Attitudes and Practice of Cervical Cancer Screening among Female University Students from 25 Low, Middle Income and Emerging Economy Countries. Asian Pac J Cancer Prev 2015; 15 (17): 7235-7239.
- Hoque ME, Ghuman S, Coopoosmay R, et al. Cervical Cancer Screening among University Students in South Africa: A Theory Based Study 2014. PLoS ONE 9 (11).
- Mulatu K, Motma A, Seid M, et al. Assessment of Knowledge, Attitude and Pratice on Cervical Cancer Screening among Female Students of Mizan Tepi University, Ethiopia, 2016. Cancer Biol Ther Oncol 2017; (1):1.
- Hinkula M, Pukkala E, Kyyronen P, et al. A population-based study on the risk of cervical cancer and cervical intraepithelial neoplasia among grand multiparous women in Finland British Journal of Cancer 2004; 90: 1025–1029.
- Louie KS, deSanjose S, Diaz M et al. Early age at first sexual intercourse and early pregnancy are risk factors for cervical cancer in developing countries British Journal of Cancer 2009; 100: 1191 – 1197
- Wongwatcharanukul L, Promthet S, Bradshaw P et al. Factors Affecting Cervical Cancer Screening Uptake by Hmong Hill tribe Women in Thailand. Asian Pac J Cancer Prev, 2014; 15 (8): 3753-3756
- IARC. IARC Monogr Eval Carcinogen Risks Hum. Human Papillomaviruses, International Agency for Research on Cancer: Lyon 2007: 90
- American cancer society. (2017).Causes, Risk factors and Prevention of cervical cancer. https://www.cancer.org/cancer/cervical-cancer/causes-risks-prevention/risk-factors.html. Accessed: 23/02/ 2018.