Information
Journal Policies
Squamous Cell Carcinoma of Vaginal Vault with Liver, Adrenal and Brain Metastases: Report of an Uncommon Presentation
Abhishek Purkayastha1*, Sankalp Singh1, Niharika Bisht1, Prabha Shankar Mishra2, Azhar Husain3
2.Department of Onco-Pathology, Command Hospital (Southern Command), Pune, India
3.Department of Nuclear Medicine, Command Hospital (Southern Command), Pune, India
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Squamous cell carcinoma (SqCC) of vaginal vault post total abdominal hysterectomy may arise from either any remnant of cervix or from vagina, but the exact origin is difficult to decipher. SqCC of vaginal vault with metastases to liver, adrenal and brain without local recurrence is very uncommon and rarely heard of. We hereby report a 57 year-old-female who had underwent total abdominal hysterectomy 15 years ago developed SqCC of the vaginal vault and was treated with concurrent chemo -radiotherapy. Response assessment imaging with positron emission tomography scan 3 months post therapy showed complete resolution of the vault primary but appearance of metastatic lesion in liver and adrenal which were proven from image guided fine needle cytology. She was started on p alliative chemotherapy and functional imaging after 5 cycles of chemotherapy showed complete resolution of the metastatic lesions. However, within one month she presented with severe headache and vomiting. Magnetic resonance imaging of brain revealed multiple intracranial metastatic lesions for which she received palliative whole brain radiotherapy to which she responded significantly and has been kept on follow -up and supportive care. This case is being presented to highlight the interesting and unusual case scenario we encountered, the clinical course of the disease, the management aspects and overall prognosis.
Squamous cell carcinoma, vaginal vault, cervix, vagina, metastases, liver, adrenal, brain,Cancer Science
1. Introduction
The most common locations for distant metastases from SqCC of cervix are the lung (21%), bone (16%), para-aortic lymph-nodes (11%), abdomen (8%) followed by supra-clavicular lymph-nodes (7%) [1] while liver metastases are relatively rare, being reported in 1.2% to 4% of cases only [1-3]. Adrenal metastases from primary SqCC cervix are rarely reported in literature [4] while brain metastases are extremely rare [1,5,6] with an incidence of 0.4%-1.2% [7-10]. Similarly, SqCC of vagina most commonly metastasizes to lung, bone and least commonly to liver while adrenal and brain metastases are rarely heard of [11]. Distant metastases from cervical or vaginal cancer are usually due to recurrent disease but the present case is one such unusual presentation where a locally controlled early stage SqCC of vaginal vault disseminated within 3months after initial definitive treatment to liver and adrenal without involving the more common metastatic sites and finally to brain after complete metabolic resolution of previous lesion within a span of 4 months, indicating the aggressive nature of this disease and a poor prognosis of these patients. This case also posed a diagnostic and therapeutic dilemma as to which line of treatment to follow, whether as a case of SqCC of cervix or SqCC of vagina.
2. Case Report
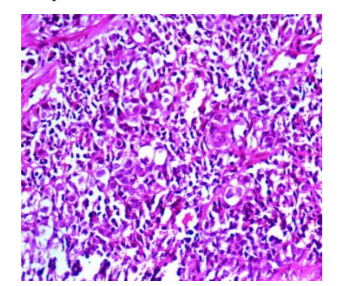
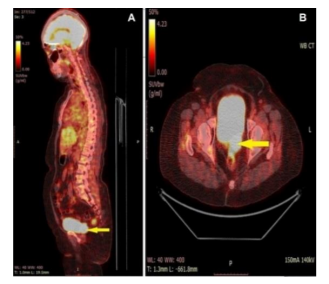
A 57-year-old female, a known diabetic on oral hypoglycemic agents with a history of TAH 15 years ago for fibroid uterus presented with complaints of discharge and bleeding per vaginum of 2 weeks duration. Gynaecological examination revealed an indurated, exophytic lesion measuring approximately 4 x 3 cm involving superior third of vaginal canal extending till middle third which bled on touch with bilateral parametrial involvement. Biopsy from the vault lesion showed poorly differentiated SqCC (Figure 1). WB-18-FDG-PET/CT scan showed a 3.3 x 4.2 x 2.6 cm soft tissue density FDG avid lesion seen involving the vaginal vault with a SUV of 16.99. Bilateral parametrial involvement was seen without extension to pelvic wall. No other distant organ involvement was present (Figure 2).
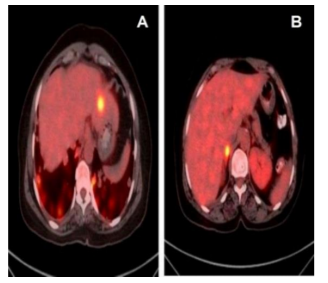
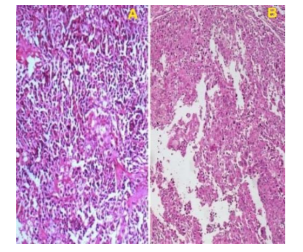
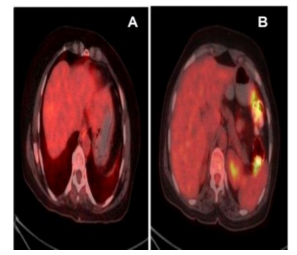
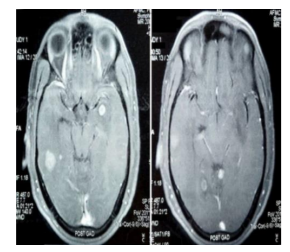
Patient was diagnosed as a case of SqC of vaginal vault FIGO stage IIB and was treated with EBRT to a dose of 50.4 Gy in 28 fractions along with 6 cycles of concurrent cisplatin 60 mg weekly followed by ICRT which she tolerated well. She was kept on follow-up and a response assessment after 3 months with WB-18-FDG-PET/CT scan revealed resolution of the vault lesion but a FDG avid lesion in the left lobe of liver measuring 2.6 cm with a SUV of 8.96 and FDG avid bulky right adrenal measuring 1.8 cm with SUV of 8.19 suggestive of metastatic lesions (Figure 3). Image guided FNAC from the liver and adrenal lesion was performed which showed metastases from SqCC(Figure 4). Patient was asymptomatic for any signs of liver or adrenal metastases and was maintaining a KPS of 70%. She was diagnosed as case of metastatic carcinoma of vaginal vault and was planned for 6 cycles of palliative chemotherapy 3 weekly paclitaxel 175 mg/m2 and carboplatin AUC 5. Post 3 cycles of palliative chemotherapy response assessment with functional imaging WB-18-FDG-PET/CT scan showed complete metabolic resolution of liver and adrenal lesions (Figure 5). She was further continued on chemotherapy but before her 5th cycle she presented with severe headache and vomiting. MRI of brain was done which showed multiple intracranial metastases mainly in the supratentorial region (Figure 6) for which she was treated with palliative WBRT to a dose of 30 Gy in 10 fractions. She responded well to WBRT with significant improvement in her symptoms and performance status and is presently kept under supportive care with close follow-up.
3. Discussion
Carcinoma of cervix is the fourth most common cancer affecting women worldwide [12,13] and leading cause of cancer related deaths in developing countries [14,15]. SqCC of cervix accounts for 90% of all cervical cancers and adenocarcinoma accounts for approximately 7%-10% of cases [1]. Carcinoma of vagina is a rare malignancy accounting for 1%-2% of all gynecological malignancies [10]. SqCC of vagina accounts for around 79% cases while remaining are comprised of other pathologies [10]. Malignant diseases of the vagina are either primary vaginal cancers or metastatic cancers from adjacent or distant organs. Primary vaginal cancers are defined as arising solely from the vagina, with no involvement of the external cervical os proximally or the vulva distally. According to FIGO, a vaginal lesion involving the external os of the cervix should be considered cervical cancer and treated as such; a tumor involving both the vulva and the vagina should be considered vulvar cancer.
Primary SqCC of cervix most commonly disseminate to the lung (21%), bone (16%), para-aortic lymph-nodes (11%), abdomen (8%) followed by supra-clavicular lymph-nodes (7%) [1], while liver metastases are relatively rare being reported in 1.2% to 4% of cases only . Metastatic involvement of adrenals by primary SqCC cervix is rare and those reported are mainly from adenocarcinoma of cervix [16]. On the contrary, distant metastases due to recurrent SqCC are commonly seen in para-aortic nodes (62%), liver (33%), lung (33 to 38%), peritoneum (5% to 27%), adrenal gland (14% to 16%), intestines (12%) and skin (10%) . Cancer that forms in squamous cells, the thin, flat cells lining the vagina constitutes the SqCC of vagina which spreads slowly and usually stays near the vagina, but may spread to the lungs, bone or liver. Adenocarcinoma begins in glandular or secretory cells in the lining of the vagina and release fluids such as mucus. Adenocarcinoma is more likely than SqCC to spread to the lungs and lymph nodes. Literature search on SqCC of vagina with adrenal metastases were inconclusive without any concrete report.
Brain metastases from SqCC cervix are extremely rare with an incidence of 0.4% to 1.2% the most common gynaecological malignancy being choriocarcinoma with an incidence of 35% [17]. Brain metastases generally occur via hematogenous route with supratentorial location being the most common site due to vascularity and the spatial characteristics of this region [5] and poorly differentiated SqCC being the most common primary as was seen in our case also. The median duration for manifestation of brain metastasis from time of diagnosis of SqCC has been reported to be around 18 months [18,19] while the median age of diagnosis around 52 years [20]. The first incidence of brain metastases from SqCC cervix was reported way back in 1949 by Henriksenin a necropsy study [21], after which there have been sporadic cases reported in world literature though the incidence has been on a rising trend over the years due to prolonged survival owing to highly improved diagnostic techniques and therapeutic measures like precision surgery, conformal radiation techniques and novel chemotherapeutic drugs. Extensive review of literature in pubmed also showed no proper reporting of SqCC of vagina with brain metastases which indicates the rarity of this occurrence.
TAH involves the removal of the uterus along with entire cervix as was done in our case. The malignant growth occurred at the post TAH vaginal vault where presence of any cervical remnant although remote but not impossible. This case posed a diagnostic and therapeutic dilemma for us as to which line of treatment to be used, whether as a case of SqCC of cervix or SqCC of vagina as both malignancies have predominantly squamous cell histology, both have the common etiological agent HPV and both have very fine parameters for differentiation as discussed above. Grossly, SqCC of vagina presents as a nodular, ulcerated, indurated, exophyticor endophytic mass lesion along the vaginal walls to involve either the cervix or vulva. It is actually difficult to distinguish histologically a primary vaginal SqCC from a cervical SqCC, although the majority of vaginal lesions are moderately differentiated [11] and our case had poorly differentiated histology seen more in cervical cases. Taking all evaluation parameters into consideration it was decided to treat her on lines of SqCC of cervix as it is the most common pathology of this region as compared to carcinoma vagina because about 80% of vaginal cancers are metastatic, primarily from the cervix or endometrium while spread from the vulva, ovaries, choriocarcinoma, recto-sigmoid, and bladder are less common. These cancers usually invade the vagina directly. Cancers from distant sites that metastasize to the vagina through the blood or lymphatic system also occur, including colon cancer, renal cell carcinoma, melanoma, and breast cancer. Therefore she was initially treated with single agent chemotherapy cisplatin instead of triple regimen of cisplatin, 5-fluorouracil and mitomycin-c used in vaginal carcinoma with EBRT.
Regarding the management aspects of solitary metastases to liver from primary SqCC cervix, surgery has been attempted with good results [22]. The indications for metastasectomy or hepatectomy of solitary liver metastases from colorectal cancer and neuro-endocrine tumors have shown relatively good prognoses, whereas the same for NCNNLM remain controversial owing to the limited number of cases and the heterogeneity of the primary diseases [23]. Isolated adrenal metastasis from primary SqCC of cervix has been managed with adrenalectomy but may later develop primary adrenalin sufficiency or Addison’s disease .Other treatment options for isolated adrenal metastasis is SBRT and image guided percutaneous ablation [24]In our case as the patient developed both liver and adrenal metastases from SqCC, no surgical intervention was contemplated and was treated with palliative systemic therapy to which she showed complete metabolic response. For brain metastasis management usually involves palliative EBRT in the form of WBRT, surgery, or both depending on the clinical scenario. Surgical intervention is done in cases with a solitary intracranial lesion located at an amenable site or in cases with diagnostic dilemma and in cases where the metastatic lesion cause mass effect and raised intracranial tension. Patients with multiple, or inoperable lesions are usually treated with palliative WBRT with significant improvement in their symptoms as was done in our case. Surgical excision of the solitary lesion combined with adjuvant EBRT yields a better survival than radiotherapy alone. WBRT plus SRS boost to resection site as compared to WBRT alone has shown to improve local control and survival however, though the prognosis remains dismal. Most studies have reported a median survival of only a few months, but there are a few reports of long-term, disease-free survival in these patients
4. Conclusion
Dissemination to distant sites from advanced invasive SqCC cervix has been reported in the literature and most of these data based on necropsy studies with an incidence of 22.4% [25]. SqCC of cervix or vagina disseminating via haematogenous route without involving the lymphatic pathway are rare, however synchronous involvement of adrenal is rarer followed by metastases to brain is an extremely rare scenario with a poor prognosis and a median survival from diagnosis to death about 2.3 months . The diagnosis of liver metastasis should always be considered whenever any patient earlier treated for SqCC cervix or vagina presents with vague abdominal discomfort or weight loss, dark-coloured urine, jaundice, pain in the right shoulder, pain in the upper right abdomen, nausea, vomiting, confusion, sweats, fever and an enlarged liver. Adrenal metastases are generally asymptomatic but may present with back pain, abdominal pain, haemorrhage into the abdomen and adrenal insufficiency or Addison's disease causing hypotension, hypoglycemia, hyponatremia and hyperkalemia. In asymptomatic patients like our case, the role of WB-18-FDG-PET/CT scan becomes extremely important in detecting silent metastasis and therefore further management. SqCC is more often FDG avid than adenocarcinoma [1] and PET/CT provides highly accurate localization of focal radiotracer uptake, which significantly improves the diagnostic accuracy compared with PET or CT alone [1]. This case describes the rarity, mode of presentation, high degree of clinical suspicion required in detecting uncommon metastases, importance of functional imaging and multimodality treatment exhibited with significant therapeutic effect.
References
- Perez CA, Thorstad WL. Perez and Brady’s Principles and Practice of Radiation Oncology. 6th ed. Philadelphia: Lippincott Williams and Wilkins, Walters Kluwer Business; 2013. p . 1358- 1359.
- S. Tangjitgamol, C. F. Levenback, U. Beller and J. J. Kavanagh. Role of Surgical Resection for Lung, Liver, and Central Nervous System Metastases in Patients with Gynecological Cancer: A Literature Review. International Journal of Gynecological Cancer 2004; 14(3): 399-422.
- Ramia JM, De La Plaza R, Quiñones J, Veguillas P, Adel F, Parreño JG. Liver Metastases from Gynecological Cancers: Time to Resection? Surgical Science 2012; 3:120-5.
- Theivasikamani D, Srinivasan L, Bakthavachalam R. Adrenal gland metastases - an unusual manifestation of cancer cervix. Int J ReprodContraceptObstetGynecol 2017; 6(9):4150-3.
- Amita M, Sudeep G, Rekha W, Yogesh K, Hemant T. Brain Metastases From Cervical Carcinoma – A Case Report. Medscape General Medicine 2005;7(1):26.
- Aggarwal T, Sawke N, Sawke G. Intracranial metastases from carcinoma of the cervix: A rare case report. Clin Cancer Investig J 2014;3:573-5
- Setoodeh R, Hakam A, Shan Y. Cerebral metastases of cervical cancer, report of twocases and review of the literature. Int J ClinExpPathol 2012;5(7):710-4.
- Ikeda S-i, Yamada T, Katsumata N, Hida K,Tanemura K, Tsunematu R, Ohmi K, Sonoda T,Ikeda H, Nomura K. Cerebral Metastases in Patientswith Uterine Cervical Cancer. Japanese Journal of Clinical Oncology 1998; 28: 27-9.
- Cormio G, Pellegrino A, Landoni F, Regallo M,Zanetta G, Colombo A, Mangioni C. Brain metastasesfrom cervical carcinoma. Tumori1996; 82: 394-6.
- Chura JC, Shukla K, Argenta PA. Brain metastasesfrom cervical carcinoma. Int J Gynecol Cancer 2007; 17: 141-6.
- Perez CA, Thorstad WL. Perez and Brady’s Principles and Practice of Radiation Oncology. 6th ed. Philadelphia: Lippincott Williams and Wilkins, Walters Kluwer Business; 2013. p. 1465-1491.
- Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin 2005; 55: 7108-74
- Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J ClinOncol 2006; 24: 2137-50.
- CervicalCancer:EstimatedIncidence, Mortality and Prevalence Worldwide in 2012. International Agency for Research on cancer and World Health Organization; 2012.
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Can J Clin 2011;61: 69-90.
- Baron M, Hamou L, Laberge S, Callonnec F, Tielmans A, Dessogne P. Metastatic spread of gynaecological neoplasms to the adrenal gland: case reports with a review of the literature Eur J GynaecolOncol 2008;29(5):523-6.
- Yordan EL Jr, Schlaerth J, Gaddis O, Morrow CP. Radiation therapy in the management of gestational choriocarcinoma metastatic to the central nervous system. ObstetGynecol 1987;69:627-30
- Peters P, Bandi H, Efendy J, Perez-Smith A, Olson S. Rapid growth of cervical cancer metastasis in the brain. J ClinNeurosci 2010;17:1211-2.
- Brown Iii JV, Epstein HD, Kim R, Micha JP, Rettenmaier MA, Mattison JA, et al. Rapid manifestation of CNS metastatic disease in a cervical carcinoma patient: A case report. Oncology 2007;73:273-6.
- Cormio G, Pellegrino A, Landoni F, Regallo M, Zanetta G, Colombo A, et al. Brain metastases from cervical carcinoma. Tumori 1996;82: 394-6.
- Henriksen E. The lymphatic spread of carcinoma of the cervix and of the body of the uterus; a study of 420 necropsies. Am J ObstetGynecol 1949;58: 924-42.
- Bacalbașa N, Balescu I. Surgical Approach of Cervical Cancer Liver Metastases: Case Report. Journal of Surgery [Jurnalul de chirurgie] 2015; 11(2): 385-7
- Takemura N, Saiura A. Role of surgical resection for non-colorectal non-neuroendocrine liver metastases. World Journal of Hepatology 2017; 9(5): 242-51.
- Frenk, N., Daye, D., Tuncali, K. et al. Local Control and Survival After Image-Guided PercutaneousAblationofAdrenal Metastases . Journal of Vascular and Interventional Radiology 2018. 29(2):276-84.
- Marcial-Rojas RA, Meigs JV. Cancer of the cervix uteri: A review of 169necropsied cases. Am J Pathol 1955; 31: 1077-82.