Information
Journal Policies
Stratification of PSA Response to Empirical Antibiotic Therapy to Predict the Possibility of Prostate Cancer in TRUS Biopsy
Ginil Kumar P1, Abhishek Laddha2*, Datson P Abraham3, Appu Thomas4
2.Fellow in uro oncology, Amrita Institute of medical sciences and research center, Kochi, Kerala, India.
3.Consultant Urologist, Amrita Institute of medical sciences and research center, Kochi, Kerala, India.
4.Prof and head department of urology, Amrita Institute of medical sciences and research center, Kochi, Kerala, India.
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction: Aim of our study was to assess the response of the PSA to empirical antibiotics in patients with PSA 4 to 10 ng/dl and to correlate the prostate biopsy finding in relation to the PSA response following 3 weeks of antibiotic therapy.
Methods: A prospective study of 99 patients presenting to urology OPD at a single centre with elevated PSA levels with clinically normal Digital rectal examination (DRE) was done. All patients with no clinical evidence of prostatitis and prostate cancer were included in the study and were given 3 weeks of empirical antibiotic. All patients underwent TRUS biopsy irrespective of PSA values at 3 weeks.
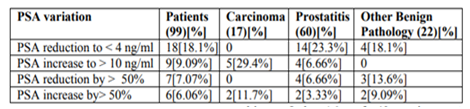
Result: Out of the total 99 patients, 17 patients with carcinoma prostate had a pre and post-antibiotic PSA of 8.78 ng/ ml and 10.04 ng/ml. The rest (82) patients had a pre and post treatment PSA 6.95 ng/ml and 5.84 ng/ml. Patients who had the reduction of PSA to less than 4ng/dl (n =18,18.1%) or reduction of PSA by more than 50 % (n=7, 7.07%) had no cancer detected on biopsy.
Conclusion: An empiric course of antibiotic therapy may be reasonable prior to prostate biopsy for patients with PSA range of 4-10 ng/ml in the geographical area where there is a low prevalence of prostate cancer. Reduction of PSA by 50 % from initial levels or PSA level less than 4 ng/dl after antibiotic may help in identifying patients which can be followed up in without immediate biopsy.
PSA, TRUS biopsy, Prostate cancer,Urology
1. Introduction
Prostate-specific antigen (PSA) is most common screening tool used for early detection of prostate cancer. Elevations in the serum PSA concentration can occur as a result of various factors limiting the specificity of PSA testing for prostate cancer. Elevation of PSA may occur as a result of various non-malignant conditions such as benign prostatic hyperplasia, inflammation, and infection. Correlation between acute and chronic prostatitis and increased serum PSA levels is well established[1,2]. Subclinical inflammation of the prostate could elevate serum PSA in patients without clinically detectable prostate cancer. Prostate cancer is found in only in 20 to 30 % of patients with PSA range of 4 to 10 ng/dl [3,4]. leading to unnecessary biopsy in rest of patients with associated morbidity. Prostatitis is a significant health problem with a prevalence rate of 11 – 16%. In geographical areas where there is low prevalence of prostate cancer and high probability of PSA elevation due to chronic prostatitis it may be prudent to consider a course of empirical antibiotics and assess the response to the treatment prior to embark on a biopsy.
The aim of our study was to stratify patients with PSA 4 to 10 ng/dl according to the PSA response to empirical antibiotic treatment and to accesses the possibility of prostate cancer detection depending on the change in PSA following antibiotic therapy. The incidence of chronic prostatitis and correlation with PSA was evaluated as well.
2. Methods
Patients presenting to urology OPD at the department of urology from November 2015 to May 2018 with elevated PSA levels in the range of 4 to 10 ng/dl with clinically normal Digital rectal examination (DRE) were included in the study. The study protocol, consent forms were approved by institutional ethics and scientific committee.
Patients who had any clinical suspicion of malignancy or infection on DRE, evidence of UTI (symptomatic or asymptomatic) were excluded from the study. Patients who had a history of acute or chronic urinary retention or history of catheter placement in recent past were also excluded. Patients who had any contraindication for TRUS biopsy like coagulopathy, painful perianal conditions were also excluded.
All patients were given detailed information regarding the objectives of study in their vernacular language and written consent was taken. PSA estimation was done in all patients on enrolment and after 3 weeks of an antibiotic course. (Tab. ofloxacin 400 mg once a day for 3 weeks from the date of initial PSA estimation, Doxycycline was an alternative drug for patients with a history of drug allergy to quinolones). Pre and post-antibiotic PSA values were used to calculate the PSA change.
PSA change was calculated according to the formula (PSA after antibiotic - initial PSA / initial PSA) x100. Independently from the value of the repeated PSA 3 weeks after antibiotic therapy, all patients were submitted to trans-rectal ultrasound guided standard template 12 core biopsy on the same day of review.
3. Results
A total of 99 patients were assessed for PSA change with antibiotic therapy. All patients received Ofloxacin as monotherapy for 3 weeks and tolerated it well without any interruption due to side effects. Mean age of patients in our study was 64 years (64.4 ± 6.68 years) with age range of 48 to 78 years. Mean prostate volume in our study was 35 cc (35.0 ± 17.0).
The mean pretreatment PSA was 7.26 ng/ml and the mean post-antibiotic PSA was 6.56 ng/ml with a PSA change of 9.78 %, p = 0.006 for the total 99 patients which shows an overall reduction.
There were 57 patients who showed a reduction in PSA after 3 weeks. The mean age of the patients in this group was 63.4 ± 6.77 years. The mean PSA change was 32 %± 18.2%, the prostate volume was 34 ± 18.3cc. The pre-treatment PSA 7.27ng/ml ± 1.76 and the post-treatment PSA, 4.96ng/ml ± 1.91 with p = 0.001.
18 (18.1%) patients showed a reduction of PSA to less than 4ng/ml and none among them had cancer detected on TRUS guided prostate biopsy. There were 7 patients with PSA (7.07%) reduction by more than 50%, they had a mean pre- and post-treatment PSA of 7.4ng/ml and 2.9ng/ml respectively and none of them had cancer detected on biopsy.
Out of 99 patients, 60 had chronic Prostatitis with a mean pretreatment PSA of 7.24 ng/ml. The mean post-antibiotic PSA in patients who had chronic Prostatitis and those who did not have chronic Prostatitis was 5.95 ng/ml and 7.51 ng/ml which was statistically significant p = 0.012 suggesting antibiotic had an influence on decreasing PSA in patients with Prostatitis. There was no statistical difference in the age and prostate volume, while the PSA change was statistically significant p = 0.002. (Table 1).
The post-antibiotic PSA had a significant correlation (Pearson’s correlation) with pretreatment PSA, p < 0.001. 44 of 57 patients with PSA reduction had chronic prostatitis on biopsy. Only 16 out of 42 patients with increased or unchanged PSA had chronic prostatitis and these patients could have had isolated foci of prostatitis and the PSA rise may be due to an inadequate antibiotic response. (Which supports our hypothesis that a response to antibiotics may predict the possibility of chronic prostatitis)
Out of the total 99, there were 17 patients with carcinoma prostate who had a pre and post treatment PSA of 8.78 ng/ml and 10.04 ng/ml. The rest (82) patients had a pre and post treatment PSA 6.95 ng/ml and 5.84 ng/ml.
The post-antibiotic therapy comparison of PSA between the carcinoma and the non-carcinoma group was statistically significant (p = 0.001), with definite rise in the PSA (10.04 ng/ml) in the carcinoma group. The PSA change also was found to be statistically significant p = 0.002. The post antibiotic PSA had significant correlation (Pearson’s) with pretreatment PSA, (p < 0.001 and PSA change, p < 0.001)
There were only 3 (5.3%) out of 57 patients who had carcinoma prostate with PSA reduction, while there was a significant rise of PSA in other 14 patients (33.3%) out of 42 patients with increased or unchanged PSA. The mild reduction in PSA in the three patients could have occurred due to focal prostatitis which would have responded to antibiotics.
4. Discussion
PSA is most common tool used for screening as well as early detection of prostate cancer. Patients presenting with PSA (4 – 10) ng/ml are routinely evaluated in outpatient clinic setting. In the countries like India where the incidence of carcinoma prostate is lower and incidence of prostatitis is relatively higher, there is significant possibility that the number of unnecessary biopsies are higher. The present indications for prostate biopsy are based on literature from western countries where there is high incidence of prostate cancer relative to that of prostatitis.
The present study analyses the effect of antibiotic therapy on PSA levels and whether a decrease in PSA could postpone or avoid the biopsy in certain patients and predict the possibility of chronic prostatitis versus prostate cancer It has recently been suggested that, in managing men with elevated PSA, the decision for biopsy based on one single value may be inappropriate. The prostate biopsy could, in fact, be avoided or postponed in men with normal DRE who have a normal age-specific repeated PSA, eventually after a course of antibiotics[5,6]. Nadler et al [7] demonstrated the presence of chronic inflammatory cells in 64.3% of men undergoing transrectal ultrasound biopsy for elevated PSA. Okada et al[8] assessed high PSA readings due to inflammation and, based on histological findings, concluded that acute inflammation within the prostate is a significant contributor to elevated serum PSA levels, especially in patients with small prostates. Statesman et al.[9] studied the inflammation in prostate biopsies in which there was no cancer and found inflammation in virtually every one of them, even in the ones without any signs of clinical prostatitis. These authors concluded that subclinical inflammation could cause PSA elevation, emphasizing that nearly half of all clinically asymptomatic men with an elevated PSA level have laboratory signs of prostatitis. They suggested that two weeks of ciprofloxacin administration would result in a drop in the elevated PSA levels of almost 50% of patients with lower urinary tract symptoms (LUTS) and normal DRE results, thus avoiding prostate biopsy. This approach, however, requires careful follow-up, especially for patients whose PSA levels fail to decrease to normal levels[9]. Brett et al.[10] found, in 300 randomly selected men, category IV prostatitis prevalence of 32.2% and serum PSA levels significantly higher (P - 0.0004) than in men without prostatitis.
In our study, the incidence of chronic prostatitis in the total patient group was 60 (60.6%). Out of 57 patients who had a PSA reduction with quinolones, 44(77%) patients had chronic prostatitis on biopsy. According to the literature, clinical success and microbiological eradication reaching 75% can be achieved with quinolone group antibiotic therapy in bacterial chronic prostatitis,[11]Therefore, although studies on larger series are required, starting directly with quinolone group antibiotics appears to be a good alternative.
Reduction in serum PSA level after antibiotic therapy is well documented in various studies. Stratification of response after the antibiotic is an important consideration that we propose in selected population to avoid or defer a biopsy. Reduction of PSA by 50 % from initial levels and/or PSA level less than 4 ng /dl after antibiotic may help in identifying patients which can be followed up in without immediate biopsy.
In the present study the rise in PSA from the baseline within 3 weeks has been strongly associated with the presence of cancer, 10(38%) out of 26 patients had a positive TRUS for carcinoma prostate. Flavio L. Heldwein [12] reported that patients with histologically proven carcinoma have more sustained absolute PSA increases than negative results (22.4% vs –5.3 ng/mL; P = 0.001). Recently, Stopiglia et al.[13] reported on 98 patients with type IV prostatitis who were randomly assigned to either ciprofloxacin or placebo. They found that a decrease in PSA was not associated with a diagnosis of carcinoma (31 vs 26.7%).
In the present study patients with a reduction of PSA of more than 50% have been found to have no cancer at biopsy. PSA reduction less than 40% showed only 3 patients with carcinoma prostate. The study by Serretta et al[14] has revealed that PSA reduction greater than 70% shows no cancer at biopsy. Our study in the present Indian scenario would suggest that a PSA reduction greater than 50% may be taken as a cut off for delaying the prostate biopsy as 6 out of 7 patients had a PSA fall below 4ng/ml. These patients should be on a close follow up, but larger volume studies are further needed to validate the statement.
In the series by Serrata et al [14] comparison of decreased PSA and unchanged/increased PSA revealed that 59 patients had decreased PSA out of which 12 (20.3%) had cancer prostate. 40 patients were in the unchanged + increased PSA group who had 16 (40%) cancer detected on biopsy (P - 0.02) which clearly estimated that the incidence of cancer prostate was high in the group with increased and unchanged PSA. PSA sensitivity was 75 and 100% and the negative predictive value was 77 and 100% respectively.
Scardino criticized the unjustified use of antibiotics in a group of patients and emphasized the various inherent disadvantages associated with this approach, such as cost, toxicity, and the promotion of resistant bacterial species development that exposed the patient to more resistant and aggressive sepsis should a biopsy eventually be done[15]. We believe if we carefully select patients with indeterminate PSA, reduction in number of people undergoing biopsy may be significant. But in countries like ours where there is higher prevalance of prostatitis compared to carcinoma of prostate, an empirical antibiotic course may not only reduce the biopsy rate but also will reduce the chance of post biopsy flare up of infection.
The drawback of our study is limited sample size and no control group. Further studies with larger sample size of patients with PSA level 4-10 ng/ml from areas where there is low prevalence of prostate cancer will help us to find an answer to the question if a course of empiric antibiotics will be useful in avoiding biopsy in the responders.
5. Conclusion
Prostatitis is a significant confounding factor which can affect PSA levels and may lead to unnecessary biopsy with associated morbidity. Stratification of patients based on PSA response to the empirical antibiotic may help in reducing unnecessary biopsy and the use of adjunctive PSA-based parameters for prostate cancer screening in patient population with low privalance of carcinoma of prostate Reduction of PSA by 50 % from initial levels or PSA level less than 4 ng /dl after antibiotic may help in identifying patients which can be followed up without immediate biopsy.
References
- Dalton DL. Elevated serum prostate-specific antigen due to acute bacterial prostatitis. Urology 1989; 33: 465–469. Epub 1989/06/01
- Neal Jr DE, Clejan S, Sarma D, Moon TD. Prostate specific antigen and prostatitis. I. Effect of prostatitis on serum PSA in the human and nonhuman primate. Prostate 1992; 20: 105–111. Epub 1992/01/11
- Keetch DW, Catalona WJ, Smith DS. Serial prostatic biopsies in men with persistently elevated serum PSA values. J Urol 1994; 151: 1571–1574. Epub 1994/06/01.
- Eskic¸orapc¸ SY, Baydar DE, Akbal C, Sofikerim M, Gunay M, Ekici S et al. An extended 10-core transrectal ultrasonography guided prostate biopsy protocol improves the detection of prostate cancer. EurUrol 2004; 45: 444–449. Epub 2004/03/26
- Hochreiter W, Wolfensberger P, Danuser H, Studer UE. Antibiotic treatment of asymptomatic inflammatory prostatitis in patients with elevated psa: can biopsies be avoided EurUrol 2004; 3 (Suppl 2): 204; Abstract 806.
- Singh R, Cahill D, Popert R, O’Brien TS. Repeating the measurement of prostate-specific antigen in symptomatic men can avoid unnecessary prostatic biopsy. BJU Int 2003; 92: 932–935. Epub 2003/11/25
- Nadler RB, Humphrey PA, Smith DS, et al. Effect of inflammation and benign prostatic hyperplasia on elevated serum prostate specific antigen levels. J Urol 1995; 154(2 Pt 1):407–13
- Okada K, Kojima M, Naya Y, Kamoi K, Yokoyama K, Takamatsu T, et al. Correlation of histological inflammation in needle biopsy specimens with serum prostate- specific antigen levels in men with negative biopsy for prostate cancer. Urology. 2000;55(6):892-8. Epub 2000/ 06/07.
- Schatteman PH, Hoekx L, Wyndaele JJ, Jeuris W, Van Marck E. Inflammation in prostate biopsies of men without prostatic malignancy or clinical prostatitis: correlation with total serum PSA and PSA density. Eur Urol. 2000;37(4):404-12. Epub 2000/04/15.
- Brett S, Carver BS, Bozeman CB, Williams BJ, Venable DD. The prevalence of men with National Institutes of Health category IV prostatitis and association with serum prostate specific antigen. J Urol 2003; 169: 589–591.
- Bundrick W, Heron SP, Ray P, Schiff WM, Tennenberg AM, Wiesinger BA, et al. Levofloxacin versus ciprofloxacin in the treatment of chronic bacterial prostatitis: a randomized double-blind multicenter study. Urology. 2003;62(3):537-41. Epub 2003/08/30.
- Heldwein FL, Teloken PE, Hartmann AA, Rhoden EL, Teloken C. Antibiotics and observation have a similar impact on asymptomatic patients with a raised PSA. BJU Int.107(10):1576-81. Epub 2011/01/20.
- Stopiglia RM, Ferreira U, Silva MM, Jr., Matheus WE, Denardi F, Reis LO. Prostate specific antigen decrease and prostate cancer diagnosis: antibiotic versus placebo prospective randomized clinical trial. J Urol.183 (3):940-4. Epub 2010/01/22.
- Serretta V, Catanese A, Daricello G, Liotta R, Allegro R, Martorana A, et al. PSA reduction (after antibiotics) permits to avoid or postpone prostate biopsy in selected patients. Prostate Cancer Prostatic Dis. 2008; 11(2):148-52. Epub 2007/07/20.
- Scardino PT. The responsible use of antibiotics for an elevated PSA level. Nat ClinPract Urol. 2007; 4(1):1. Epub 2007/01/11.