Information
Journal Policies
Risk of Acute Lung Injury Associated with Nitrofurantoin Use for Urinary Tract Infection
Rajasreepai Ramachandrapai MD1, Raghesh Varot Kangath MD1*
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
We herein report a case of acute lung injury following treatment with Nitrofurantoin for a urinary tract infection. Patient presented with symptoms of sepsis and rash that improved with steroids. This case emphasizes the need to consider Nitrofurantoin induced drug reaction in patients presenting with symptoms of acute lung injury following exposure to Nitrofurantoin.
Nitrofurantoin, acute lung injury, DRESS syndrome, fever,Urology
1. Introduction
The diagnosis of nitrofurantoin related lung injury requires a high clinical suspicion because of the atypical presentation and associated co-morbidities. It is under reported and misdiagnosed by clinicians leading to worsening of patient condition and prolonged hospitalizations.
The incidence of nitrofurantoin associated lung injury (acute and chronic) is reported in the literature as less than 1% of patients treated with Nitrofurantoin and 85 % of these cases are reported in women [1] that are treated for urinary tract infection. In a case control study three cases were reported with acute lung injury among 16101 patients treated with the first course of oral nitrofurantoin [2]. Bronchiolitis obliterans organizing pneumonia has been reported in patients on nitrofurantoin. In a case of Dress syndrome patient who took nitrofurantoin developed circulatory and renal failure along with eosinophilia and a rash [3].
Nitrofurantoin is one of the drugs causing lung injury from a list of over 350 offending agents described in literature over the last few decades from pubmed. The Groupe d'Etudes de la Pathologie Pulmonaire Iatrogene (GEPPI), a clinical study group, provides information regarding drug induced lung injury, collects and updates literature on drug-induced lung disease. The objective of this group is to publish updated lists of offending compounds and to provide warnings when adverse effects of drugs are recognized [4].
The awareness of drug induced pulmonary disease is increasing among primary care physicians and hospitalists. Still it is not uncommon to misdiagnose nitrofurantoin related lung injury as pneumonia and subsequent treatment with antibiotics. Because most of them have underlying urinary infection, some symptoms like fever, rash and hypotension are diagnosed as urinary infection with sepsis rather than as drug fever.
2. Case Description
A 71 year old female with history of type II diabetes mellitus admitted with shortness of breath, fever, and progressive rash. Four days prior to admission, she was seen by her primary care physician who prescribed nitrofurantoin for urinary infection. After the second dose of antibiotics the following day, patient developed persisting fever of 102, lethargy, and rash. The fever was associated with chills. On the third day of fever, she noticed the rash - described as pruritic, non-scaling diffuse reddish areas over her thighs and lower abdomen. In addition, the patient also had generalized malaise and nausea during the same time period as the rash.
Her chronic medical conditions include well control type II diabetic mellitus and hypertension while taking Quinapril, Hydrocholorothiazide, Glipizide and recently added Nitrofurantoin. She is allergic to Sulphur containing drugs which causes pruritis of the feet. She had a twenty pack year history of smoking; quit 10 years ago, and no alcohol or substance abuse.
When first presented to the emergency department, she was lethargic, but arousable. Her temperature was 102° F, pulse rate of 100 beats/min, and blood pressure of 70/40 mmHg. Multiple maculopapular rashes with a maximum diameter of 3cm were seen over the thighs and lower abdomen with no desquamation or vesicles. Patient has dry mucous membranes without jaundice. Heart sounds were normal without murmurs, rubs, or gallop. Respiratory efforts were appropriate but with crackles over bilateral bases of the lungs. Her bowel sounds were normal without abdominal distention, tenderness, mass, or rigidity. Extremities showed no edema with normal pulsations. Neurologically, the patient was alert, awake, oriented to person, place, time, and situation without any focal deficit.
Lab data on admission showed a white blood cell count of 19000. Aspartate aminotransferase and alanine aminotransferase were 112/ 130. Serum eosinophils were elevated at 12 %. Urine analysis and microscopic examination was negative for white blood cells, negative for leukocyte esterate or nitrite with 4 white blood cells in the urine. Chest x-ray report showed bilateral patchy airspace disease. Further laboratory data obtained over the course of the hospital stay including blood cultures, sputum culture, urine streptococcal and legionella antigens, antinuclear antibody, ANCA, Ebstein Barr virus and Hepatitis B and C were negative.
With a presumptive diagnosis of septicemia from atypical and/or community acquired pneumonia she was started on ceftriaxone and azithromycin, along with intravenous normal saline. However the antibiotics were discontinued on the second hospital day, as the diagnosis of an infection seemed unlikely with clinical history, exam, and diagnostic testing. The distribution of the rash had changed during the hospital day. The rash disappeared from thighs and abdomen on third hospital day after receiving intravenous steroids and appeared on upper extremities, neck and upper chest and back. By the fourth day, the rash on the trunk had resolved and was limited to the extremities; however, the palms and soles were always spared. The distribution suggested a centrifugal nature of spread. The rash and fever resolved on fourth hospital day. During the fifth day, patients fever had abated, rash had resolved, the pulmonary exam showed improvement and the patient was hemodynamically stable and the steroids were tapered off; Patient was discharged home off antibiotics.
Given the scenario of recent nitrofurantoin use and symptoms suggestive of acute lung injury (cough, fever), and the way the hospital course had evolved (eosinophilia, transaminitis, pulmonary infiltrates with resolution 48 hours after stoppage of nitrofurantoin, a drug induced fever with an acute pulmonary reaction seemed to be most conclusive explanation for her symptoms with Nitrofurantion being the presumed offending agent.
3. Discussion
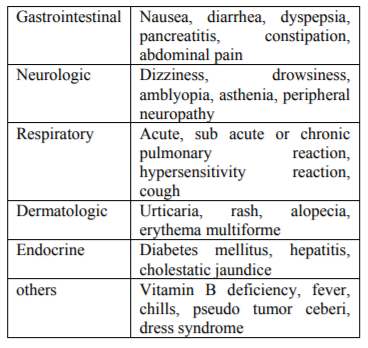
Common side effects include acute fever, lung injury, and gastric upset and while effects to chronic therapy include hepatotoxicity, hemolytic anemia especially in neonates, acute lung injury is a non-dose related bizarre idiosyncratic reaction to nitrofurantoin. In clinical trials of Macrobid, the most frequent clinical adverse events that were reported as possibly or probably drug-related were nausea (8%), headache (6%), and flatulence (1.5%). Some of the side effects are listed in Table 1 by the organ system involved [2].
The exact pathophysiologic mechanism in nitrofurantoin related lung injury is not known and is thought to be contributed by hypersensitivity reaction in acute and immune mediated mechanism in chronic lung injury. The lung reactions to nitrofurantoin can be classified as acute, sub acute and chronic depending on the onset of symptoms and duration of drug therapy.
Nitrofurantoin is a bactericidal drug used in treatment of Escherichia Coli or Staphylococcus Saprophyticus infections of the lower urinary tract. It acts by inhibiting bacterial cell wall synthesis and by inhibiting bacterial acetyl coenzyme A activity and is a preferred drug for lower urinary tract infections due to sustained susceptibilities to gram positive and negative bacteria compared to other antimicrobial agents. The lack of clinically significant bacterial resistance development to nitrofurantoin is likely due to the combination of nitrofurantoin's multiple sites of attack and mechanisms of action.
Acute pulmonary reactions, which are the most common type of lung injury with Nitrofurantoin (83%), present as fever, chills, cough, and shortness of breath, serum eosinophilia, and elevated erythrocyte sedimentation rate and pulmonary infiltrates on X-ray.
Pathological findings include mild interstitial inflammation, fibrinous alveolar exudates, focal hemorrhage and vasculitis. Ventilation-perfusion lung imaging shows transient reverse ventilation-perfusion mismatch in acute nitrofurantoin lung toxicity which resolves after 24 to 48 hours of stopping the drug [5]. About 47 % of patients with acute lung injury had reversal of the symptoms 2 weeks after stopping the nitrofurantoin.
In subacute reaction, fever is less pronounced and develops within few weeks of nitrofurantoin therapy. Lab findings might show elevation of Ig G, ANA titers and mild eosinophilia. It resolves slower than acute reaction after discontinuation of the drug.
Chronic nitrofurantoin reaction of lung occurs in patients on the drug for over six months for prophylaxis of urinary tract infections and presents with malaise, dyspnea on exertion, cough and altered pulmonary function. Fever and eosinophilia are less pronounced than acute or subacute. X-ray might show diffuse interstitial pneumonitis or fibrosis.
Reticular pattern and traction bronchiectasis in Chest X- ray are commonly seen in chronic nitrofurantoin toxicity. Lung biopsy shows lymphocytic interstitial inflammation with fibrosis. Pulmonary function tests show a restrictive pattern with decreased total lung capacity (TLC), forced vital capacity (FVC), and single-breath carbon monoxide diffusion capacity (DLCO). Although DLCO is always reduced, normal lung volumes may be seen. Chronic nitrofurantoin toxicity of lung can persist permanently even after discontinuation of nitrofuration and steroid therapy with an 8-10% mortality as compared to 0.5% with acute lung injury [6].
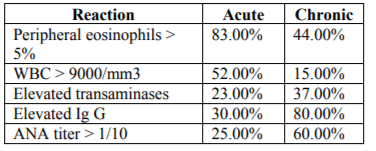
Lab findings in acute and chronic nitrofurantoin toxicity are summarized in Table 2[1].
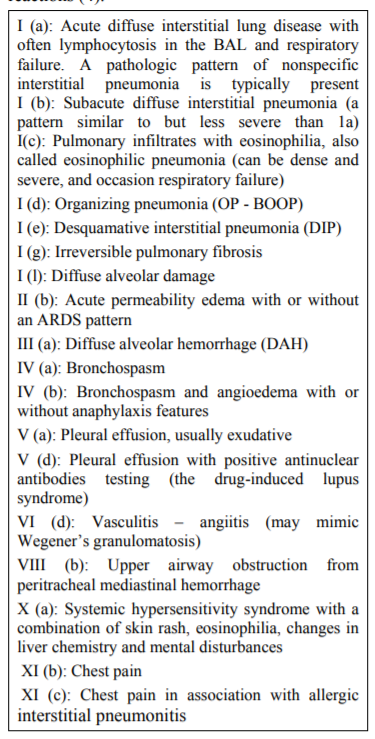
The various patterns of lung injury reported with Nitrofurantoin as per the Groupe d'Etudes de la Pathologie Pulmonaire Iatrogene (GEPPI) is listed as follows. The injuries in lung are classified into different groups based on type of reactions [4].
The major problem with all imaging is that drug-related lung toxicity has a nonspecific appearance, and similar patterns have been described with many interstitial lung diseases.
Bronchoalveolar lavage is helpful to exclude infectious etiologies, but the findings in nitrofurantoin associated lung injury are nonspecific. Lung toxicity resulting from various drugs can induce similar changes and in patients taking drug combinations, the imaging findings alone may not reveal the culprit. There are no specific markers that can distinguish drug induced lung injury from interstitial fibrosis due to infections, sarcoidosis, idiopathic interstitial fibrosis or pneumoconiosis.
The first step should be to stop the offending drug (nitrofurantoin) and supportive management like fluid resuscitation and acetaminophen for fever. Steroids are indicated in severe cases of acute and chronic nitrofurantoin related lung injury like hypoxemic respiratory failure or in failure of resolution of symptoms with supportive care.
4. Conclusion
Drug induced lung disease is a major cause of iatrogenic injury. As most patients with Nitrofurantoin have underlying urinary tract infection, a common mistake would be to make a diagnosis of septicemia or pneumonia with systemic inflammatory response instead of drug fever with lung injury. Acute pulmonary toxicity has been described in patients who showed no pulmonary reaction with previous nitrofurantoin exposures[7].
The key lies in early diagnosis and stoppage of the offending drug. Also, drug induced etiologies need to be considered in patients newly diagnosed with interstitial fibrosis but a direct causal relationship is often difficult to establish
References
- B. Vahid & B. M. Wildemore: Nitrofurantoin Pulmonary Toxicity: A Brief Review. The Internet Journal of Pulmonary Medicine. 2006 Volume 6 Number 2
- Jick SS, Jick H, Walker AM, Hunter JR. Hospitalization for pulmonary reactions following nitrofurantoin use. Chest 1989; 96: 512-515
- Velema MS, Voerman HJ Dress syndrome caused by nitrofurantoin Neth J Med 2009 April; 67 (4):147-9.http://www.pneumotox.com/index. php?fich=accueil&lg=en
- Lee NK, Slavin JD Jr, Spencer RP. Ventilation-perfusion lung imaging in nitrofurantoin-related pulmonary reaction. Clin Nucl Med 1992; 17 :94-96
- Schwarz MI, King TE. Interstitial lung disease. 4th Ed. Hamilton, Ontario; Lewiston, NY: BC Decker; 2003
- Bucknall CE, Adamson MR, Banham SW. Nonfatal pulmonary hemorrhage associated with nitrofurantoin. Thorax 1987; 42:475-476.