Information
Journal Policies
Clinical Relevance of Bimanual Palpation in Bladder Cancer Patients Referred to a Tertiary Reference Centre
Mette Holberg Sorensen1, Jorgen Bjerggaard Jensen1
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background: Patients diagnosed with muscle-invasive bladder cancer (MIBC) or high-risk non muscle-invasive bladder cancer (NMIBC), are often referred to specialized uro-oncological centres for further treatment. At some centres, the patients are examined through an uro-oncological assessment including cystoscopy and bimanual palpation (BP) of the pelvis in general anaesthesia to detect an inoperable tumour. The aim of this study was to compare the results of BP at the referring hospital with the results at a tertiary reference center.
Materials and Methods: Medical records from 156 patients referred to a single tertiary referral centre for cystectomy, were reviewed retrospectively. Data from the referring hospital regarding results of BP, pathologic examination of tumour tissue from the transurethral resection of the bladder (TURBT) and anaesthetic assessment were compared with corresponding data from the reference centre. In analysis of the validity of BP, a total of 96 patients who underwent cystectomy or explorative laparotomy were included.
Results: A fixed tumour was found in 5 (5%) of the analysed patients, all had minimum T2 tumour at the primary TURBT specimen. In 2 of these 5 patients, the tumour was already described as fixed or possible fixed at referring hospital. In additionally 2 patients, BP was not described or not performed at the referring hospital. Only in one patient with MIBC, the tumour was described as potentially mobile at referring hospital but was evaluated as fixed at the reference centre.
Conclusion: Information from referring hospital regarding BP is correct in 98% of patient where the tumour is described as non-palpable or mobile. In these cases, a BP in general anaesthesia before radical cystectomy can be omitted.
Bimanual palpation; bladder cancer; cystectomy; preoperative assessment, Subject classification codes: Cancer, Bladder, Urology
1. Introduction
Current standard in diagnosis and clinical staging of MIBC and high-risk NMIBC comprises imaging of the urinary bladder tract by computed tomography (CT, or positron emission tomography-CT (PET-CT) scan of thorax, abdomen and pelvis for nodal involvement and distant metastasis, pathology review of tumour tissue after transurethral resection (TURBT) performed at the referring hospital, cystoscopy and bimanual palpation (BP) with the patient in general anaesthesia [1]. In addition, an anaesthetic assessment of whether the patient is suitable for radical surgical treatment will be made. Patients from the Central Denmark Region diagnosed with muscle-invasive bladder cancer (MIBC) or high- risk non-muscle-invasive bladder cancer (NMIBC) are referred to the Department of Urology, Aarhus University Hospital (AUH) for further evaluation and treatment. Until recently, all patients referred to AUH underwent an uro-oncological assessment including BP in general anaesthesia irrespectively of findings described at the primary TURBT from the referring department. BP of anaesthetized patients can be decisive of whether patients with bladder cancer are suitable for radical local treatment. A fixed tumour (clinically T4b) excludes the patient from primary radical cystectomy and radiotherapy. Instead, systemic chemotherapy should be initiated if not contraindicated. As a necessary part of the patient assessment at the referring hospital all patients are, however,
2. Materials and Methods
Medical records from 156 bladder cancer patients referred to AUH for cystectomy from March 2012 to June 2014 were reviewed retrospectively. Data from the referring hospital regarding results of BP, pathologic examination of tumour tissue (histological type and T-stage) from the primary TURBT and anaesthetic assessment of the patient were registered. These data were compared to data recorded at AUH regarding BP at the reference centre, pathological central review of the primary TURBT specimen and anaesthetic assessment of the patient.
All pathological reviews were done by a single experienced uropatologist at the reference centre. When evaluating the quality of BP, information as to whether the patient was operable at the time of cystectomy or explorative laparotomy or if BP had revealed a clearly fixed tumour in not operated patients, was used as reference. All patients referred to AUH (n=156) were included when comparing local pathology versus central review pathology results. For the analysis of the validity of BP, only patients where BP was decisive for further treatment, were included (n=96). Thus, patients with distant metastasis (n=21), patients receiving conservative treatment (n=17), patients receiving radiation therapy (n=20), patients who died before treatment (n=1), and patients refusing treatment (n=1) were excluded. When comparing anaesthetic assessments, only patients who underwent radical cystectomy were included (n=91). Of the patients undergoing cystectomy, 23 (25%) underwent neoadjuvant chemotherapy. All of these had mobile tumour at BP.
3. RESULTS
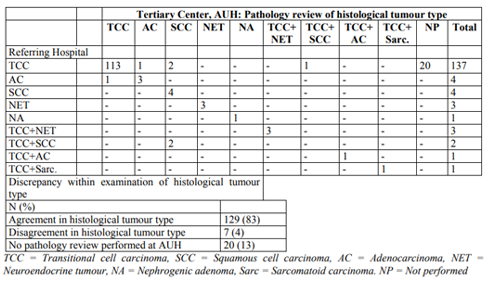
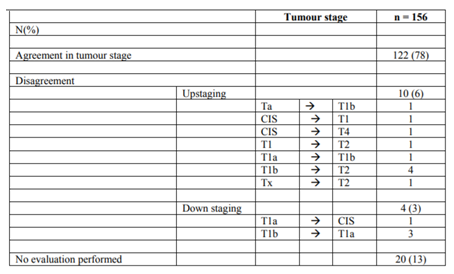
The distribution and correlation between histological tumour type found in the primary TURBT specimen at the referring hospital and the review pathology at AUH are shown in Table 1. Referring and central histological examination were identical in 129 (83%) of the patients. In 7 (4%) of 156 patients, pathology review changed the diagnosis from one histological type to another, but this had no influence on the treatment decision in any of these patients. Table 2 shows the review pathology at AUH on tumour stage of the primary TURBT specimen compared to the result at referring hospital. In 122 of the tumours (78%) there was agreement in the tumour stage. Pathology review up-staged the tumour T-stage in 10 of the 156 cases (6%) and in six patient’s pathology review changed the diagnosis from a Table2. Central review pathology on tumour stage superficial to a muscle invasive tumour of stage T2 or greater. In four patients (3%), the tumour stage was down-staged at pathology review. No down-staging from muscle-invasive to non- muscle-invasive tumour was seen. In 20 patients (13%), no pathology review was performed at AUH.
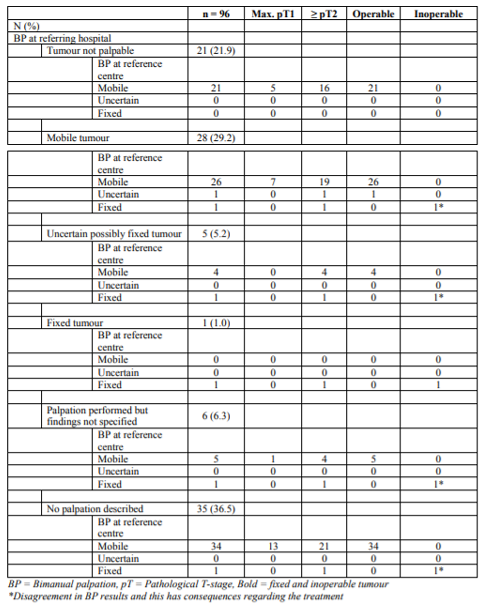
Of 156 patients, only 88 (56%) underwent BP at the referring hospital. In the remaining 68 patients (44%), BP was not performed or at least not documented in the clinical file. In Table 3, patients were stratified into six groups according to the BP findings at the referring hospital and findings at the reference centre. The BP findings were identical at referring hospital and at the reference centre when the tumour was described as not palpable tumour or fixed tumour at the referring hospital. Out of a total of 28 patients (29%) in whom BP at referring hospital suggested a mobile tumour, one tumour was found to be fixed at BP at the tertiary reference centre and therefore excluded from radical cystectomy. In five patients (5%), the BP findings at the referring hospital suggested an uncertain possibly fixed tumour, the BP at the tertiary centre revealed a fixed tumour in one of these cases. When no palpation was performed (n=35) or the palpation was not specified (n=6) at the referring hospital, the BP at the reference centre revealed a fixed tumour in two cases.
4. Discussion
Both national Danish and international guidelines define BP as an integral part of routine pre-treatment evaluation in order to obtain information about mobility of the tumour [1,2]. No palpable tumour at BP indicates a NMIBC or a superficial T2 tumour whereas an immobile mass suggests a T4b tumour. Mobile masses felt by BP, indicates T2 or T3 tumour, for both radical cystectomy is the gold standard treatment [2]. In this study, we evaluated the value of BP at the referring hospital compared to the BP at a tertiary referral centre. When compared with the results at cystectomy, all mobile tumours found on BP at the reference centre, were operable, thus indicating that the BP was accurate. However, it is not clear from the present study whether patients not undergoing cystectomy based on finding of a fixed tumour potentially would have been operable.
In the literature, the accuracy and quality of BP has only scarcely been reported. Thus, only two studies have been made about the accuracy of BP. Mehrsai et al. [3], compared the results of BP with the pathologic results in 32 patients, who had undergone radical cystectomy. They found that BP had a specificity of 82%, sensitivity of 46%, positive predictive value of 70%, and negative predictive value of 63% in estimating extra vesical involvement of tumour [3].
Ploeg et al. [4] aimed to determinate the accuracy of clinical staging through BP. The study included 335 patients who underwent BP and cystectomy. Preoperative tumour-stage determined through BP was compared with post-cystectomy pathologic tumour-stage. They found that accurate staging through BP was observed in 58%. Four of 9 patients who had a suspected T4b tumour on BP but who underwent cystectomy anyway, appeared to have operable tumours at cystectomy. Discrepancy was observed in 42% of the patients: in 11% clinical over-staging and in 31% clinical under-staging. Thus, the study concluded that some caution is warranted when interpreting the findings at BP [4].
Abundant evidence is found in the literature regarding discrepancies between clinical T-stage based on the pathologic examination of the primary TURBT specimen and other diagnostics including BP and pathological outcomes in the cystectomy specimen in MIBC and high risk NMIBC [5-7]. Shari at et al. reported that in 42% of 778 patients, clinical under-staging occurred and clinical over-staging in 22% [6]. McLaughlin et al. found that of 141 patients undergoing cystectomy, 54% were up-staged on the pathological stage in the cystectomy specimen [5]. Thus, the results in the literature suggest that the preoperative clinical staging in bladder cancer is inaccurate and therefore the imaging options and studies play an important role in staging of bladder cancer.
Abdominal and pelvic CT is the most commonly used imaging modality. Unfortunately, CT is unable to differentiate the different layers (lamina propria, superficial and deep muscle) of the bladder [8]. Thus, CT has a limited accuracy in preoperative local tumour staging [9]. When staging the primary tumour, CT under-stage tumour stage in 10-39% and over-stage in 6- 34% [10]. When comparing CT with magnetic resonance imaging (MRI) techniques, MRI seems clinically better with a reported staging accuracy of 62–85% compared with 35–55% in CT studies [8,11]. A major problem is that over- staging occurs when investigating locally invasive bladder cancer with MRI. Tekes et al. reported 32% over-staging [13] and Liedberg et al. 49% over-staging when MRI results were compared with the pathological tumour stage in the cystectomy specimen [12]. With these findings in mind, we cannot rely exclusively on imaging. Thus, the preoperative clinical T-stage based on pathologic examination of the TURBT specimen and BP is still important.
Out of 156 patients in the present study, only 88 (56%) underwent BP at the referring hospital. This implies that in the remaining 44%, the national and international guidelines were not followed or at least the execution and findings of BP were not registered in the clinical files. Both possibilities give cause for concern because guidelines report the most actual insights in the best clinical practice, and correct registration in the patient files is inherent to good medical practice.
Our study had a weakness regarding the evaluation of the quality of BP. Evaluation was only possible in 91 (95%) patients who underwent radical cystectomy. Five patients who had a fixed tumour on BP at the reference centre were not treated with radical cystectomy. Therefore, no judgement could be made about the exact tumour stage.
5. Conclusions
The information from referring hospital regarding BP is valid in cases where the tumour is described as non-palpable or mobile. In these cases, the patients can avoid an additional procedure in general anaesthesia prior to cystectomy. If in doubt or a fixed tumour is described at referring hospital, a BP remains relevant. The study also shows that referring departments generally need to be better to perform and describe BP at the primary TURBT.
References
- http://www.skejby.net/Webudgaven/DaBlaCa2 010.htm.
- Witjes JA, Compérat E, Cowan NC, et al. EAU guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2013 guidelines. Eur Urol. 2014;65(4):778-792.
- Mehrsai, A., Mansoori, D. TM. A Comparison between Clinical and Pathologic Staging in Patients with Bladder Cancer Reading Tools. Urol Journal, North Am. 2004:22-26.
- Ploeg M, Kiemeney LALM, Smits GA, et al. Discrepancy between clinical staging through bimanual palpation and pathological staging after cystectomy. UrolOncol. 2009;30(3):247- 251.
- McLaughlin S, Shephard J, Wallen E, Maygarden S, Carson CC, Pruthi RS. Comparison of the clinical and pathologic staging in patients undergoing radical cystectomy for bladder cancer. IntBraz J Urol. 2007;33(1):25-31; discussion 31-32.
- Shariat SF, Palapattu GS, Karakiewicz PI, et al. Discrepancy between Clinical and Pathologic Stage: Impact on Prognosis after Radical Cystectomy. Eur Urol. 2007;51(1):137-151.
- Dutta SC, Smith JA, Shappell SB, et al. Clinical under staging of high risk nonmuscle invasive urothelial carcinoma treated with radical cystectomy. J Urol. 2001;166(2):490- 493.
- Ng CS. Radiologic diagnosis and staging of renal and bladder cancer. SeminRoentgenol. 2006;41(2):121-138.
- Baltaci S, Resorlu B, Yagci C, et al. Computerized tomography for detecting perivesical infiltration and lymph node metastasis in invasive bladder carcinoma. Urol Int. 2008;81(4):399-402.
- Bostrom P, W.G. van Rhijn B, Fleshner N, et al. Staging and Staging Errors in Bladder Cancer. Eur Urol. 2010;9(1):2-9.
- McKibben MJ, Woods ME. Preoperative Imaging for Staging Bladder Cancer. CurrUrol Rep. 2015;16(4).
- Liedberg F, Bendahl P-O, Davidsson T, et al. Preoperative staging of locally advanced bladder cancer before radical cystectomy using 3 tesla magnetic resonance imaging with a standardized protocol. Scand J Urol. 2013;47(2):108-112.
- Tekes A, Kamel I, Imam K, et al. Dynamic MRI of bladder cancer: evaluation of staging accuracy. AJR Am J Roentgenol. 2005;184 (1):121-127.