Information
Journal Policies
Surgical Management of Urachal Adenocarcinoma: how to Find a Good Compromise between Functional and Oncological Result?
Ibrahim Mejdoub1, Youssef Mejdoub2, Mohamed Fourati1, Mohamed Amine Mseddi1, Sami Rekik1, Haitham Rejab2, Mourad Hadjslimen1, Nouri Rebai1, Mohamed Nabil Mhiri11
2. General surgery department, Habib Bourguiba University Hospital, Sfax, Tunisia.
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract:Urachal adenocarcinoma is a rare and aggressive pathology. Its long occult evolution is responsible for a delay diagnosis. Surgery, which is his only potentially curative treatment, was initially very extensive. The current trend is towards less heavy surgery. However, a higher local recurrence rate after partial cystectomy was reported. This weighs down the prognosis.
We report the case of a 54-year-old man with primary urachal adenocarcinoma treated with partial cystectomy, urachal block resection and bilateral lymphadenectomy. Five years after surgery, no recurrence through CT scan and ultrasound examination was observed.
1. Introduction
Urachal adenocarcinoma is a rare and aggressive tumor, accounting for less than 1% of all bladder cancers [1]. Currently, there is no consensus regarding the management of this uncommon malignancy. Earlier published case series have suggested en bloc radical cystectomy and wide excision of the urachus and umbilicus [1]. Recently, the standard procedure has leaned more toward partial cystectomy with urachal resection, but a very small bladder remnant may be left occasionally.
As an alternative to radical cystectomy, we opted instead to do partial cystectomy and augmentation cystoplasty with good oncological and voiding result.
2. Case Report
A 54-year-old diabetic male presented with two episodes of painless hematuria in 4 months, dysuria, urgency and frequent urination for 1 year. On physical examination, there were no positive physical findings. The urinary tract ultrasonography (US) revealed an abnormal echo in the bladder and routine urinalysis was positive for occult blood. Urine cytology was negative for malignant cells. The patient underwent cystoscopy that showed an irregular mass with eroded surface on dome and anterior wall with a limited bladder capacity of 300 ml. Transurethral resection of bladder tumor was performed showing histologic findings indicative of low grade mucinous adenocarcinoma. Given these findings, the differential diagnosis at the time included: Adenocarcinoma from other organs, particularly colorectum, urachal carcinoma and bladder primitive adenocarcinoma. Colonoscopy did not reveal evidence of primary cancer involving the colon.
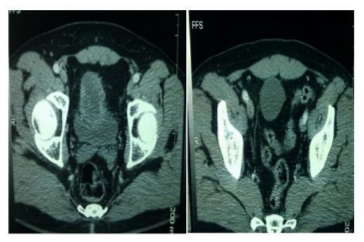
Contrast-enhanced computed tomography (CT) scan of the abdomen showed a circular hypodense mass located at the top and anterior wall of the bladde with heterogeneous enhancement of the mass. Without accompanying enlarged lymph nodes or other sign of metastatic disease. (Figure 1)
A partial cystectomy with excision of urachal and umbilicus with pelvic lymphadenectomy was done. Frozen section confirms negative surgical margins.
Almost whole of the supratrigonal bladder was excised, and the remaining bladder was very low capacity. Therefore, le patient underwent a bladder enlargement using 15 cm of ileum in U configuration. (Figure 2).
Final histopathology confirmed urachal carcinoma with negative margins and pelvic nodes being free of tumor. There were no post-operatitive complications. No adjuvant therapy was proposed due to complete resection with negative margins and absence of a secondary location. Postoperative recovery was uneventful. The patient was well-satisfied with voiding. The patient never had any nocturnal incontinence. After 5 years of follow-up, there was no evidence of local or systemic recurrence of tumor on cystoscopy, abdomen and chest CT.
3. DISCUSSION
The urachus is a vestigial structure of the allantois that generally disappears after birth. During embryogenesis, the allantois regresses to form the urachus, a tubular structure that connects the urinary bladder and the umbilicus. After the third trimester, the urachus usually involutes as a fibrous cord, which coalesces with the obliterated umbilical arteries and forms the median urachal ligament [2].
However, an urachal remnant, may persist in a third of adults [3]. it is characterized by a tubular or cystic muscular structure that is lined by epithelium, from which urachal cancers can arise [1].
Urachal carcinomas are rare, accounting for less than 1% of all bladder cancers.
While most bladder carcinomas are urothelial carcinoma, the vast majority of urachal carcinomas are adenocarcinoma, which typically produces abundant extracellular mucin and exhibit focal signet ring cell features [4].
Although it is most commonly found at the bladder dome, the urachal remnant can also be found anywhere along the bladder midline, including the posterior and anterior walls [1].
Often, patients present at the time of diagnosis with higher stage and poor prognosis, because of the rarity of symptoms at an early stage [5].
The disease is usually advanced when symptom appears, such as hematuria, mucous-like discharge, irritative voiding and umbilical pain.
Standard imaging workup for urachal cancer includes US, CT scan, and/or magnetic resonance imaging (MRI) evaluation of the abdomen and pelvis. On US, the tumor is observed as a soft tissue mass, which may consist of heterogeneity and calcification. While nonspecific, internal vascularity can sometimes be seen with Doppler imaging [5]. CT scan and MRI, on the other hand, are often used for local staging and evaluation of distant metastasis.
Thali-Schwab et al analyzed the results of 25 CT examinations of urachal adenocarcinomas and reported that calcification is the characteristic sign of urachal adenocarcinoma, particularly urachal mucinous adenocarcinoma [6].
In addition, cystoscopy is also recommended. Diagnosis of urachal carcinoma is usually confirmed by cystoscopy and biopsy.
Several staging systems are used; Sheldon, Mayo Clinic and TNM. Jasreman et al found that higher stage is associated with worse survival [1].
Surgery is the most effective option for localized disease. While radical cystectomy has traditionally been done, the gold standard surgical approach for the management of localized urachal cancer is an excision of the urachus, umbilicus, and partial cystectomy combined with bilateral pelvic lymphadenectomy.
However, Extension of microscopic disease beyond palpable margin is common and hence margin of 2–3 cm with multiple frozen sections is advocated by Donat and Harry [7].
After partial cystectomy, the importance of resection results in inadequate functional urinary reservoir with storage symptoms. Otherwise, neobladder is associated with high rates of persistent night time incontinence, particularly in the first 2 years, and this reduces quality of life and sexual function.
Oncological outcome after partial cystectomy, once negative margin is achieved is found to be equivalent to radical cystectomy [7].
We thus chose to perform bladder enlargement after partial cystectomy rather than radical cystectomy. It has many advantages: Technically less difficult surgery, use of smaller length of intestine, less metabolic complication, no ureter reimplantation, good continence, and less chance of requiring intermittent catheterization.
4. CONCLUSION
Few cases reported the use of bladder augmentation as in management of urchal carcinoma. After 5 year of follow-up, there was no evidence of local or systemic recurrence.
This technique may be a good alternative to radical cystectomy with neobladder. It gives a good capacity bladder with excellent continence with good short-term oncological result.
References
- Dhillon J, Liang Y, Kamat AM, Siefker-Radtke A, Dinney CP, Czerniak B, Guo CC. Urachal carcinoma: a pathologic and clinical study of 46 cases. Hum Pathol. 2015 Dec; 46(12): 1808–14. https://10.1016/j.humpath.2015.07.021.
- Schubert GE, Pavkovic MB, Bethke-Bedurftig BA. Tubular urachal remnants in adult bladders. J Urol. 1982; 127:40–2. [PubMed: 7057501].
- Zhang J, Wu J. Options for diagnosis and treatment of urachal carcinoma. Asia Pac J Clin Oncol. 2013; 9:117–22. https://doi.org/10.1111/ j.1743-7563.2012.01592.x.
- Dinney CP, McConkey DJ, Millikan RE, Wu X, Bar-Eli M, Adam L, Kamat AM, Siefker-Radtke AO, Tuziak T, Sabichi AL, Grossman HB, Benedict WF, Czerniak B. Focus on bladder cancer. Cancer Cell. 2004; 6:111–6. [PubMed: 15324694].
- Molina JR, Quevedo JF, Furth AF, Richardson RL, Zincke H, Burch PA. Predictors of survival from urachal cancer: a Mayo Clinic study of 49 cases. Cancer 2007; 110:2434-40. https://doi.org / 10.1002/cncr.23070.
- Thali-Schwab CM, Woodward PJ and Wagner BJ: Computed tomographic appearance of urachal adenocarcinomas: Review of 25 cases. Eur Radiol 15: 79-84, 2005. https://10.1007/ s00330-004-2408-z.
- Donat MS, Harry HW. Urachal tumors. In: Vogelzang NJ, Scardino PT, Shipley WU, Debruyne FM, Linehan WM, editors. Comprehensive Textbook of Genitourinary Oncology. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2006. pp. 893–8.