Information
Journal Policies
Cushing's Syndrome Related a Giant Adrenal Adenoma
Moh Adi Soedarso1*, Erik Prabowo2, Danu Sulistyowati3, A Gunawan Santoso4, Devia E Listiana5, K Hery Nugroho6
2.Digestive Division, Surgery Department, Academic Medical Center Dr. Kariadi Hospital, Diponegoro University, Indonesia
3.Anesthesia Department, Academic Medical Center Dr. Kariadi Hospital, Diponegoro University, Indonesia
4.Radiology Department, Academic Medical Center Dr. Kariadi Hospital, Diponegoro University, Indonesia
5.Pathology Anatomy Department, Academic Medical Center Dr. Kariadi Hospital, Diponegoro University, Indonesia
6.Endocrinology Division, Internal Medicine Department, Academic Medical Center Dr. Kariadi Hospital, Diponegoro University, Indonesia
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
A large adrenal adenoma case that shows a complete picture of Cushing's syndrome. Clinically led to malignant right adrenal tumor. Endocrine manipulation, laparoscopic adrenalectomy surgery performed. No event adrenal crisis, syndrome disappear.
Adrenal adenoma, Cushing’s syndrome, laparoscopic adrenalectomy,Urology
1. Introduction
Adrenal adenomas are responsibility of approximately 10-15% of cases of Cushing’s syndrome. It can be either ACTH-dependent (pituitary adenoma or ACTH independent (extra pituitary adenoma). Multidisciplinary approach: endocrine manipulation, surgery, specific anesthetic procedure is needed in management of this case.
2. Case Report
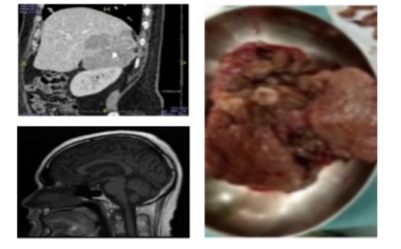
A 20-year-old man was admitted for evaluation of Cushing’s syndrome. He presented history of headache, fatique, mood disorder, hypertension (Blood Pressure 170/120 mmHg), moon face, buffalo hump, striae rubrae. Cortisol serum laboratory increased 33,53 µgr/dl (Normal range: 3,09 – 16,6µgr/dl). Abdominal CT Scan showed a right adrenal mass diameter 10,53 x 6,83 cm, heterogeneous pattern with calcified and necrotized area.
Level of ACTH < 5 pg/ml (Normal range: 6 – 50 pg/ml), absence hypothalamus pituitary defect in brain MRI angiography led to the primary site on adrenal (figure 1, bottom-left).
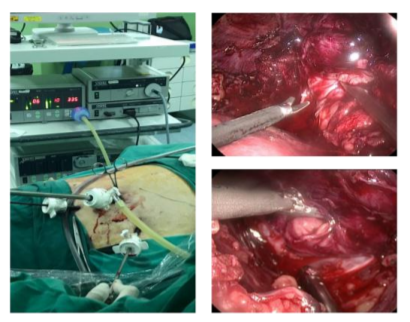
Manipulation with ketoconazole 600 mg daily to treat hypercortisolemia. The patient underwent laparoscopic right adrenalectomy. Preparation of hydrocortisone 100 mg during anesthesia-surgery to prevent occurrence adrenal crisis.
Patient position LLD, 11mm trocar port with 0, 30-degree optic, 2 port 5mm for working element. Harmonic ultrasoundshear used to dissection, hemoLock clip to control vascular. Right subcostal incision makes to remove adrenal gland. EBL 1000 cc, close monitoring in ICU ward. 5
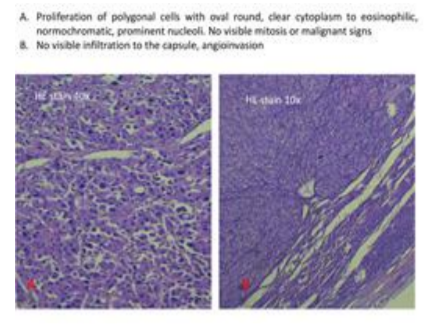
Hydrocortison continued 5 days after surgery. Ventilatory support remove in 2 day after surgery. Fifth day condition stabil without sign of adrenal crisis, patient send to elective ward. Gross specimen appear giant adrenal, 15 x 10 cm (figure1,right). Cortex area has a solid elasticity consistency. Some areas of necrosis are suspected of malignancy. But systematic microscopic investigations shown no visible mitosis or malignant signs (figure 3 A)
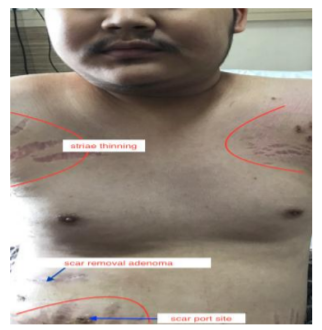
On the fifth day after surgical intervention, postoperative cortisol level at 12 µgr/dl. Seventh day, surgical wound healing well with minimum dose NSAID orally. Striae thining, gynecomastia, buffalo hump, moon face reduced.
The patient was regularly followed up at Endocrine division, Internal medicine department. Moon face have been eliminated, no striae and good mood condition. Blood pressure was 130/ 70 mmHg (without antihypertensive drugs) and cortisol serum was 4,52 µgr/dL and independent from steroid medication.
3. Discussion
We manipulated with ketoconazole by considering the hypothalamic adrenal pituitary axis to overcome due to excess cortisol. Endocrinologist can make a normal cortisol titer, and laparoscopic surgery can be performed. Another problem is that both clinical and heterogeneous physical imaging and large > 8 cm should be suspected and managed as a case of malignancy. Ibrahim, Agrusa also Zografos reported that laparoscopic adrenalectomy for giant size adrenal to be feasible and safe so we did this procedure.
Gross specimens also show heterogeneous features, there is a solid chewy part and calcification microscopic histopathology examination does not show specific malignancy signs. Also the area of necrosis that was originally thought to be strong focus malignancy we examined carefully only showed a dead cell collection.
Post-operative Cushing's symptom disappears, normotension without antihypertension, weakness, bad emotion, thinning striae. Buffalo hump, obesity, gynaecomasti in next follow-up seems to be reduced. This convinced us that these patients were purely functional benign lessions of the giant adrenal.
4. Conclusion
Multidisciplinary approach including endocrine treatment, prevention adrenal crisis and laparoscopic adrenalectomy procedure have good result for Cushing’s syndrome due to adenoma of giant adrenal gland.
References
- Nieman LK, Bilier BM, Finding JW. The diagnosis of Cushing’s syndrome: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008: 93:1526-40
- Castinetti F, Guignat L,,Giraud P et al.Ketoconazole in Cushing’s disease: is it worth a try?. J Clin Endocrinol Metab.2014;99:1623
- Aggarwl S,Yadav S Sharma AP, Sethi V. Laparoscopic bilateral transperitoneal adrenalectomy for Cushing’s syndrome: surgical challenges and lessons learnt. SurglaparoscEndoscPercutanTech.2013;23(3):32 4-8
- Debillon E, Velayoudom-Cephise FL, Salenave S. Unilateral adrenalectomy as a first line treatment of Cushing’s syndrome in patients with primary bilateral macronodular adrenal hyperplasia. J Clin Endocrinol Metab. 2015 Dec; 100(12):4417-24. http://dx.doi.org/10.1210/jc.2015-2662.Epub 2015 Oct 9
- Zografos George N et al. Laparoscopic resection of Large Adrenal Tumor: Journal of the Society of Laparoscopic Surgeon. (2010) 14:364-368. DOI: 10.4293/108680810X12924466007160
- Agrusa A et al. Laparoscopic adrenalectomy for Large adrenal masses: Single team experience. International Journal of Surgery 12(2014). http://dx.doi.org/10.1016/j.ijsu.2014.05.050
- Bozkurt H Ibrahim et al. Laparoscopic adrenalectomy for a Large adrenal masses: Is it really more complicated? KJMS. 2015. http://dx.doi.org/10.1016/j.kjms.2015.09.005