Information
Journal Policies
Isolated Prostate Tuberculosis. Report of 3 Case
Othmane Yddoussalah1*,Alae Touzani1,Tarik Karmouni1,Khalid Elkhader1,Abdellatif Koutani1,Ahmed Ibn Attya Andaloussi1
Copyright :© 2017 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
We report in this article three cases of isolated prostatic tuberculosis. Prostate tuberculosis is a rare disease, particularly in its isolated form. This urogenital localization seems to be secondary to a haematogenous dissemination. They are 3 patients aged 28, 82 and 65 aged respectively. The symptomatology revealing is not specific and remains dominated by the signs of obstruction of the lower urinary tract. Biological and radiological examinations only provide evidence of strong presumptions, and only the pathologic study of guided echo-guided biopsies or transurethral cuttings of the prostate confirms the diagnosis. The treatment is based on chemotherapy anti-tuberculosis.
Prostate; Tuberculosis,Urology
1. Introduction
The first description of prostatic tuberculosis was made in 1882 by Jasmin [1]. The isolated form is extremely rare, as evidenced by the scarcity of observations published in the literature. While urogenital tuberculosis (UGT) is common, isolated prostatic involvement is rare, even in countries with high TB endemicity. Through a retrospective analysis of 3 cases collected in the "B" urology ward of the Ibn Sina Hospital in Rabat, we discuss the epidemiological, diagnostic and therapeutic aspects of this pathology.
2. Observations
Patient 28 years old, from Cameroon in Morocco since childhood, having a history of gonorrhea 10 years ago, supported for pain and an increase in the size of the left testis for a month and a half. We find the notion of a feverish evening with sweats. The patient claims to be ethnic with weight loss. The clinical examination is in favor of an inflammatory lesion of the left epididymis. The rectal examination finds a very firm prostate increased volume and sensitive which also evokes an infection. The ultrasound found homogeneous testes with inflammatory or tumor formation corresponding to the left epididymis. The chest radio is normal.
Biologically, the markers are negative: alpha feta protein = 5.1 (N 10) - negative HCG. The PSA is increased to 7.94. The serology HIV, TPHA VDRL and chlamydia are negative. ECBU is sterile, with no lockout or microscopic hematuria. The count is normal. The CRP is 18. Despite treatment with Ofloxacin for 1 month, the inflammation of the bursa increases with the appearance of disarray. A surgical scrotal exploration found an abscess of the epididymis that will be flattened with biopsies. Endorectal biopsies of the prostate are performing at the same time.
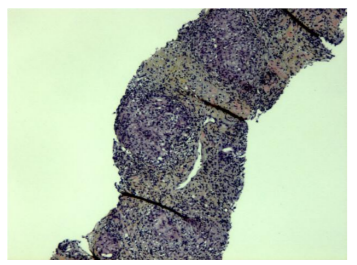
Epidididymal biopsy: epididymal localization of nonspecific inflammation. Prostate biopsy: Prostatic localization of granulomatous epithelioid and gigantocellular inflammation without necrosis, nevertheless suggestive of tuberculosis; absence of AFB (Figure 1).
The patient is treated with 6 months of quadritherapy with a favorable evolution of the clinical signs. The palpation of the stock exchanges improves with the persistence of an indurated aspect of the epididymis. At 6 months of follow-up, the patient remains dysuric, but micturely controlled by alpha blocking treatment.
Mr B. An aged 82, having as antecedents: Notion of undocumented broncho-pneumopathy, no concept of tuberculosis or tuberculous contagion, presented pain of the right hypochondrium.
For the past year, the patient has been reported urinary obstructive signs such as dysuria, diurnal and nocturnal pollakiuria, urinary urgency and micturition, all of which evolve in a context of apyrexia and unquenchable slimming. Clinical examination: Patient in good general condition, rectal examination: Homogenous hypertrophied prostate, estimated at 40g, flexible. Examination of the external genitalia: normal.
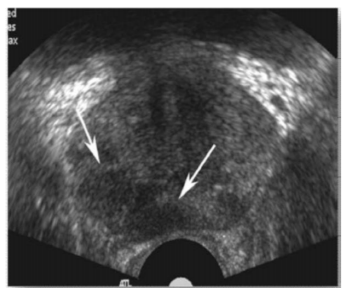
Endorectal ultrasonography shows an enlarged prostate with often irregular boundaries and a heterogeneous extractor with hypoechogenic foci (Figure 2). These lesions are localized in the peripheral zone of the prostate.
Transurethral resection of the prostate (TURP) was performed, and the pathological study was in favor of adenomatous hypertrophy with prostatic follicular causes tuberculosis.
An antibacillary treatment of 6 months was instituted according to the following diagram: 2 RHZ / 4RH.Revu one year later, the evolution was favorable with amendment of the urinary signs and improvement of the renal function.
Mr BH 65 years old, chronic smoking He underwent a transrectal prostate biopsy before been seen in our training, following a PSA test which revealed a high level of 50 ng / ml, and whose pathological study was for prostate adenocarcinoma with a Gleason score of 7 (4 + 3).Thus, the patient was admitted to the service for a (RTUP) with castration. The anatomopathological analysis was in favor of a prostatic adenocarcinoma, Gleason score (4 + 4) infiltrating more than 50% of the sample received, with lesion of tuberculous prostatitis. An antibacillary treatment over a period of 6 months was referred to the nearest health center for further antibacillary treatment. Since then, he has been lost sight of.
3. Discussion
Urogenital tuberculosis are a relatively common pathology and is the 4th extra-pulmonary localization of tuberculosis after localization: lymph node, osteoarticular and digestible, with a frequency of 15 to 30% of extra-pulmonary forms [2]. However, prostatic tuberculosis remains a rare entity and especially in its isolated form, this rarity is underlined by the majority of authors.
The age of onset is very variable according to the different series of studies. In fact, during the past 15 years, the age extremes of immune competent patients with prostatic tuberculosis ranged from 26 to 85 years [3].
All our patients are of low socioeconomic level, of rural origin. These conditions are determining factors in the outbreak and spread of the disease. Prostatic involvement is often secondary to tuberculosis of the upper urinary tract [4,5]. But it can also be primitive or secondary to epididymal or bladder tuberculosis. The risk of prostate contamination, during BCG therapy, has also been mentioned by some authors.
Clinically, the signs of obstruction of the lower body are often in the foreground. Indeed, the patient may present for dysuria, pollakuria or perineal gravity. The clinical examination is very important, the purpose of which is to seek an attack on the internal genital organs. The digital rectal examination may show a prostate increased in volume, elastic consistency, firm or stony or nodular. Nevertheless, digital rectal examination data have no specific character and can be confused with an adenoma or prostatic cancer [6,7].
The biological assessment aims essentially to find the BK in the urine or in the seminal fluid. His research in seminal fluid seems to give better results [4]. ECBU has a large part in the diagnostic process. Although it is mostly sterile, the discovery of aseptic pyuria strongly suggests tuberculosis. Currently, the polymerase chain reaction (PCR), which allows a rapid identification of the bacillus by the detection of DNA fragments in the urine, with a sensitivity and specificity much better than the culture of urine[8]. Only this technique, booming, is not common practice given its high cost.
Ultrasound often finds a prostate enlarged in volume, heterogeneous appearance with sometimes areas of calcification and necrosis. Endorectal ultrasound gives a thinner image and guides the biopsy [4]. As for CT, it can reveal multiple hypodense lesions on different prostatic lobes. However, other non-tuberculous prostatic abscesses may give similar features [9].
It turns out that no clinical, biological or radiological signs are specific to prostatic tuberculosis, and only the histopathological study will provide diagnostic certainty, microscopically, the appearance depends on two opposite processes: one of destruction and castration creating curves, the other of defense by fibrosis limiting the extension of the lesions. It is this last process that leads to obstructive phenomena [4]. The microscopic appearance is that of a typical epitheliogigantocellular granuloma with characteristic caseous necrosis [10].
Therapeutically, antituberculous chemotherapy has radically transformed the management of urogenital tuberculosis, and is currently the basis of treatment for this condition. In this framework, the WHO and in its 3rd edition (2003), recommends in the treatment of the urogenital tuberculosis a 6-month therapeutic regimen based on 4 antibacillaires: 2 RHZE / 4 RH. With the possibility of omitting Ethambutol during the initial phase for HIV-negative patients with a non-serious form of extra-pulmonary tuberculosis [11].
The surgical treatment (essentially consists of a TURP) finds its indications in the case where there is an obstruction of the lower urinary tract failure of medical treatment or the occurrence of complications. In our study, RTUP was performed in 2 patients.
4. Conclusion
Prostate tuberculosis are a condition rarely reported in the literature. No clinical, biological or radiological signs are specific to this pathology, and often pose the problem of differential diagnosis with benign prostatic hypertrophy and prostate cancer. The treatment is mainly medical and it is based on antibacillary chemotherapy. Indications for surgery are currently very small. The fact remains that the best treatment is prevention. This prevention is based on vaccination with BCG, improvement of hygiene conditions and the fight against poverty and illiteracy.
Consent Of Patients
Written informed consent was obtained from the patient’s next of kin for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Authors’ Contributions
O. Yddoussalah wrote the manuscript. All authors read and approved the final manuscript.
References
- Benjelloun S , Meziane E, Meziane F, Elmrini M. La tuberculose urogénitale , Notre expérience à propos de 58 cas.acta-urologica Belgica 1987;55(4):566–77.
- MNIF, H. LOUSSAIEF, L. BEN HASSINE, M. CHEBIL, M. AYED. Les aspects évolutifs de la tuberculose urogénitale, à propos de 60 cas. Annales d’urologie. 1998; 32(5):283-9
- VERMON M PAIS, ANDREW A WAGNER. Prostatitis tuberculous. 2007; www.emedicine.com updated: jul 19.
- Benchekroun A, Iken A , Qarro A , Aelalj H , Nouini Y, Benslimane L, et al . La tuberculose prostatique. À propos de 2 cas. Ann Urol.2003 ;37 :120—2.
- Wang JH, Sheu MH, Lee RC. Tuberculosis of the prostate: MR appearance. J Comput Assist Tomogr. 1997 ;21 : 639—40.
- Tazi K, Nouri M , Elkhadir K , Elghorfi A , Ibnattya A , Hachimi M , et al . La tuberculose prostatique Àpropos de 2 cas. Ann Urol.1999;33(4): 274–6.
- Sporer A, Oppeinheimer G. Tuberculosis of prostate gland and semi-nal vesicules. J Urol. 1957 ;78(3) :278–86.
- KOUTLIDIS N, FILLION A, MICHEL F. Tuberculose urogénitale. EMC urologie. [18-078-A-10], 2009.
- Kulchavenya E, Khomyakov V. Male genital tuberculosis in Siberians. World J Urol. 2006; 24:74—8.
- Rabii R, Fekak H, El Manni A, Joual A, Benjelloun S, El Mrini M. Fistule prostato- rectale tuberculeuse. Prog Urol. 2002 ;12: 684—6.
- Organisation mondiale de la santé : « Le traitement de la tuberculose : Principes à l’intention des programmes nationaux » ; 3ème édition, 2003