Information
Journal Policies
Complications and Problems of Penile Prosthetic Surgery in a Series of 530 Cases Operated on by the Same Surgeon in Italy
Diego Pozza1*, Carlotta Pozza2
2.Department of FPM, Sapienza University, Rome, Italy.
Citation : Diego Pozza, Carlotta Pozza. "Complications and Problems of Penile Prosthetic Surgery in a Series of 530 Cases Operated on by the Same Surgeon in Italy". ARC Journal of Urology.2017;2(2):1–11.
Copyright : © 2017 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Penile prosthetic surgery enables completely spontaneous penetrative sex and hence is the definitive solution for men with erectility’s function. Like all procedures requiring the insertion of exogenous material into the body, penile prosthetic surgery is associated with potentially serious complications, mainly due to infection or malfunction of the implant. While major complications may lead to the removal of the implant and thus the unfortunate failure of the surgeon's proposed treatment and disappointment of the patient's expectations, a number of more minor problems may arise which can be resolved without having to resort to removal. The author presents a variety of medical and surgical procedures, based on his more than 30 years (1984-2016) of experience of penile prosthetic surgery, which may be implemented to avoid implant failure.
Erectile Dysfunction, Penile Prostheses, Semi rigid Prostheses, Inflatable Prostheses
Cf: Ceftriaxone
Cp: Ciprofloxacin
Gm: Gentamycin
AMI: Acute MyocardialInfarction
HPP: Hydraulic Penile Prosthesis
CVOD: Corporal Veno Occlusive Dysfunction
1. Introduction
Penile prosthetic surgery is not particularly invasive but, given the critical and specific nature of erectile function, must produce a result which the patient finds both aesthetically and functionally acceptable [1, 2].
One of the most common and feared complications is infection, considered the worst complication in prosthetic surgery [3] and difficult to eradicate with common antibiotic therapy [4, 5]. The formation of an avascular biofilm [6,7] surrounding the prosthesis can harbor bacteria and inhibit the action of antibiotics and macrophages that would otherwise eliminate them; this almost always requires the implant's removal [8] due to the risk of generalized systemic infection.
Another common complication is the mechanical breakdown of Inflatable Penile implants (IPP) [9], which can cause them to malfunction. In this case, the implant must be removed and replaced with a different system. Given the relatively frequent occurrence of IPP break down, leading manufacturers guarantee their replacement in the event of mal function. However, the emotional effects and financial cost of a new surgical procedure, which may not be covered by health insurance, are a significant factor for patients [9].
Other complications involve the reaction of the tissues affected by the implant, with the development of oedema, lymphangitis [10], scrotal effusion, serous and bloody effusion [11,12],local and regional hyposensitivity, reduced shaft size and urinary problems, which may require further surgery, with no guarantee of success.
The presence of a reservoir in the peritoneal cavity or peri-vesical space can cause intestinal herniation, torsion and perforation, haematoma of the abdominal wall and bladder perforation [13-14]. New, low profile reservoirs, AMS Conceal [15] and Coloplast Cloverleaf [16] which are easier to insert and more adaptable, have recently been introduced.
Another not infrequent complication is caused by the incorrect sizing of the cavernous spaces, which can lead to the insertion of inappropriate cylinders. These could erode or perforate the corpora cavernosa or affect the symmetry of the penis (SST effect) [17].
There are also generic complications seen with surgery in general, and highly dependent on the surgeon's experience. Perforation of the crura and tips of the corpora cavernosa, septum, urethra, scrotum, spermatic vessels and abdominal wall can lead to major consequences for the implant and the patient if not immediately recognized and corrected [18].
The risks associated with the patient should not be over looked. The presence of diabetes, urinary tract infections, blood coagulation disorders, immune depression, duration of hospitalisation, inappropriate surgical technique and prolonged surgery time should all be assessed [19]. A psychological assessment is also important, to understand if the patient is aware not only of the benefits of a penile implant but also of its impact on his personal and relational life (use of loose clothing, practice of nudism, swimming, sports and gym activities, cycling or competitive motorcycling, medical follow-up and examinations).Prosthetic infections are a complex problem. If not immediately resolved on initial antibiotic treatment, removal of the infected implant is considered mandatory. Most infections are caused by gram-positive bacteria found on the skin, such as Staphylococci, Pseudomonas, Escherichia Coli, S. Aureus and Proteus. Infections are one of the leading causes of implant failure. For practical and above all economic reasons (given the high cost of IPP, the replacement of which might not be covered by health insurance), various "salvage" procedures have been proposed for reusing the same IPP after antibiotic "disinfection" [20].
To avoid contamination, through the air or by other means, of the penile implant, various measures have been used since the 1970s. These include separation of the operating area from the rest of the operating theatre, use of nasal antibiotics (neomycin), restriction of individuals present in the operating theatre, operating theatre not previously used for other patients and procedures, extreme care in the timing of regional hair removal (immediately before surgery), use of chlorhexidine-alcohol skin preparation, thorough washing of hands, double gloving and continuous flushing of the operating field with antibiotic solution [21,22].The use of IPP impregnated with antibiotics (Minocycline-Rifampicin) such as AMS 700 with InhibiZone, antibiotic surface treatment [23,24], or with a Coloplast hydrophilic coating, which absorbs and releases antibiotic onto the implant cylinders during preparation in the operating theatre, has led to a significant reduction in the rate of infections, but not to their elimination [25].
2.Results
A total of 530 penile implant procedures were performed between 1984 and 2016. Patients were operated on and followed up by the same surgeon (DP) (26), who also treated all cases of postoperative complication.
The costs of these procedures were not covered by the Italian National Health Service but were payable by the patients or, in some cases, by private health insurance. Economic considerations were therefore a significant factor in some operating strategy decisions.
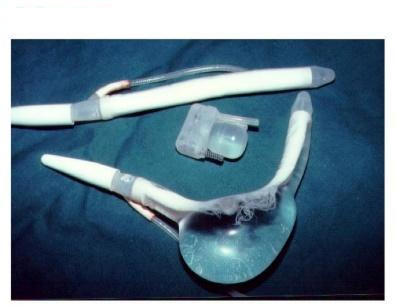
This factor partly conditioned the use of semi-rigid silicone (190 patients) or malleable (188 patients) implants (Eurogest, Implantal, Small Carrion, Jonas, Omniphase, Duraphase, AMS600, MentorAcuform, ColoplastGenesis, Subrini, SSDA-GIS), which are less costly in Italy. The use, in the remaining 152 cases, of IPP(Mentor Mark II, Alpha I, Titan OTR, AMS Hydroflex, Dynaflex, Ambicor, 700 Ultrex ,700CX, 700LGX), whose costs are standardised, was mainly decided by the patients, accordingly to their economical conditions.
The meticulous preoperative protocol in use from 1984 to 2006 (the first 318 cases) involved hair removal immediately before surgery,uncontaminated operating theatre, flushing of the operating field for 5 minutes with Betadine and alcohol and double gloving.
For organisational reasons, from 2006 to 2010, patients (cases 319-432) were prepared in the same way as for other patients undergoing genital surgery, involving hair removal up to several hours earlier, quick skin lavage with Betadine, less control over the operating theatre and single gloving.
Following some infections of hydraulic prostheses, a procedure similar to the original protocol was used from 2011 (cases 433-530), with hair removal as close as possible to surgery, first procedure in operating theatre (uncontaminated theatre), flushing of the operating field for more than 3 minutes and double gloving.
There was no difference in the incidence of infections among the three skin preparation protocols, although a more thorough preparation has been used in recent years, partly for insurance reasons.
Patient, 58 years, received an AMS700 UltrexIPP under spinal anaesthesia in 1992.He was administered preoperative antibiotic therapy with ceftriaxoneICf and ciprofloxacin (Cp). 15 days after the procedure and before the implant had been used, the patient complained of high septic fever and pain at the base of the shaft. A yellowish boil was found at the base of the penis on the right, from which issued a creamy yellowish purulent fluid (Figure. 1).
The volume of pus increased if the implant cylinders were inflated. Suspecting an infection, it was suggested to the patient that the implant should be removed. However, the patient refused categorically. A solution of iodopovidone in saline was injected into the pericavernous space (Figure. 2) and the cylinders were inflated to flush the solution out 2-3 times. Gentamycin (Gm) was then instilled and kept in loco with the cylinders partly inflated.
This procedure was performed every 8 hours for 7 days, and a progressive reduction in the volume and purulence of the secretion was observed. After 3 days Gm alone was injected, followed by the complete deflation of the implant cylinders. After 5 days no more pus was secreted and the Gm inoculation was stopped. The opening remained closed after 20 days (Figure. 3).
The cylinders were kept at maximum inflation. After another 4 days with no secretion, fever or pain, the cylinders were deflated. Since then the patient has had no further infections and has used the implant regularly from 1992 to date.
Patient, 52 years, with major Corporal- Veno-Occlusive-Dysfunction, (CVOD) received an SSDA GIS silicone implant in 2005. Unsatisfied with its rigidity, in December 2005 he requested a Mentor MARKII IPP. The patient had very intense, frequent sexual activity up to June 2013, when the cylinders suddenly stopped inflating. A new surgical procedure was performed, with antibiotic therapy with Cf, Cp and Gm. The scrotal pump was found to have malfunctioned, so the implant and reservoir were removed. A Coloplast Titan IPP was implanted. Aspiration and drainage were not used. The patient was discharged the next day with modest swelling, left scrotal haematoma and home antibiotic therapy. Onset of septic fever 8 days later. The patient did not present any significant general or local (penile or abdominal) symptoms, apart from slight pain on palpation of the left testis near the pump, which was functioning normally. X ray and US investigations were negative. The patient was hospitalised and given continuous intravenous antibiotic therapy with a mix of kanamycin, bacitracin, vancomycin, Gm, teicoplanin, piperacil lin/tazobactam, tobramycin, Cp, daptomycin and clarithromycin. However, the evening fever did not resolve. Blood cultures proved negative. The antibiotic therapy was modified for another 15 days without any effect on the fever or markers of inflammation (PCR, ESR, leucocytosis).
After 20 days of unsuccessful therapy (June 2013) it was decided to remove all components of the implant, which was apparently infected. No signs of infection were found in any of the removed components. The day after the removal the fever came down and over the next few days the blood chemical markers normalised and the patient's general condition improved.
The patient, who was strongly against having to give uphis sex life, requested another implant. It was considered dangerous to use another hydraulic system so, to avoid predictable scar tissue in his corpora cavernosa, a AMS Spectra malleable implant was implanted 15 days later, with a view to possible insertion of another IPP at a later date. The patient was unsatisfied with this implant and consulted another university hospital. After preoperative broad-spectrum antibiotic therapy for about 20 days, in December 2013 he underwent the removal of the Spectra implant and the implantation of an AMS700 CX IPP.A year later, the patient was well and satisfied with his erectile function.
The incidence of post-operative bleeding is not insignificant, especially in patients under treatment with aspirin and anticoagulants, even though they are normally instructed to stop taking these from 7 days before to 7 days after implantation. Bleeding may be caused by scrotal vascular lesions occurring during access to the corpora cavernosa, whether during positioning of the prosthetic pump or reservoir or from the corpora cavernosa themselves through incompletely closed corporotomy after semirigid or malleable penile prosthetic implant or through the necessarily incompletely closed corporotomy after IPP implantation. To avoid the risk of blood collections or postoperative haematoma, which could give rise to dangerous infections, the short term (24-36 hour) use of closed suction drainage has been proposed [12].
Patient, 52 years, who underwent reimplantation of an AMS 700CX after the breakdown of a similar IPP at the age of 45 years due to vascular problems. The patient had stopped taking aspirin 7 days previously. Following peno-scrotal incision, the cylinder and pump were removed and replaced (maintaining the reservoir) without any particular problems. Suction drainage was used, as with all the author's cases since 2006. The following morning (18 hours later) the drain had aspirated 30 mL; there was no scrotal swelling. The cylinders were deflated and it was decided to remove the drain in the afternoon, before discharge. Four hours later further examination revealed a large (10 x 10 cm) scrotal haematoma and blockage of the drain. Some suction manoeuvres were tried, but were unsuccessful. The patient was transferred to the operating theatre, where the bleeding was found to originate from the suture of the left corpus cavernosum. We inflate the cylinder fully and observed that the bleeding completely stopped. The blood collection was drained and the area flushed with antibiotics; a new suction drain was positioned and the penoscrotal incision re-stitched. The next day there were no signs of hematoma or drainage. The patient was discharged and instructed to keep the cylinders inflated for 10 days (which manoeuvre was facilitated by maintaining the previous reservoir) and to suspend aspirin for a further 15 days. Four years later the implant was still working well.
Patient, 31 years, with normal baseline coagulation parameters, underwent implantation of a Coloplast Genesis 11x22 cm implant via peno-scrotal access, without any particular difficulties. The following morning he presented a large ecchymosis involving the pelvic and genital area, without any hematoma (Figure.4).
The ecchymosis was successfully resolved through medical treatment and observation. A year later the same patient requested a Coloplast OTR IPP, as he was dissatisfied with the rigidity of the Genesis implant. Peno-scrotal access was used, and there were no particular problems with the removal of the Genesis cylinders and insertion of the reservoir, in the retropubic space, and the inter-testicular pump. Closed suction drainage was used. During the night, a large hematoma appeared, involving the scrotal sac and shaft (Figure. 5);
The drain was empty. An immediate exploratory procedure failed to identify the source of the bleeding. The area was flushed with antibiotic solution and a new suction drain positioned. The cylinders were kept fully inflated for two days. The drain, which was empty, was removed after 2 days and the cylinders were kept inflated for 5 days, until the first outpatient follow-up visit. The patient did not have any negative consequences. We referred the patient to a haematologist. Two years later he reported good penetrative activity.
In this case series, two (0.50%) scrotal haematomas were observed in 396 semi-rigid, malleable or single-component IPP, both resolved without surgery. Eight (5.9%) peno-scrotal haematoma were observed after 134 IPP. In a 52-year-old patient, a small, non-surgically-treated scrotal haematoma was thought to be the cause of subsequent IPP infection and removal.
Patient, 68 years, who hadacute myocardial infarction (AMI) at age 60; coronary angiogram at 65 years showed signs of coronary artery disease. He had an adequate erectile response with 5PDEis.At age 66, he underwent Video- Laparoscopic-Radical Prostatectomy for Gleason 6 (3+3) prostate cancer. Since then he experienced good urinary continence, no response to 5PDEis and very weak response to PGE1.He decided to have a ColoplastTitan OTR IPP. Anticoagulant therapy was suspended 7 days before the procedure and Cp begun. The implant was positioned through the peno-scrotal route after spinal anaesthesia. There was some difficulty in dilating the retropubic space, even with a Foley catheter inflated to100 c.c., but it was possible to position a 75 c.c. reservoir without reflux. The pump was positioned in the inter-testicular area and the aspirating drainage was removed after 24 hours. There was no shaft or scrotal problems at 5-day follow-up. The pump could easily be felt, although it was painful. No fever, urination normal. After 7 days the patient recommenced anticoagulant therapy. He began to notice a painless scrotal swelling; no fever. The patient found it difficult to locate the scrotal pump with his fingers. At 28 day follow-up: no fever but a taut, elastic swelling of the scrotum (15 x 15 cm), moderately painful. It was possible to locate the pump and get it to work, with inflation and deflation of the cylinders.US scan revealed that the pump was surrounded by an effusion with a corpuscular appearance. As the situation aroused concern, it was decided to operate. This involved local anaesthesia and deep sedation, antibiotic therapy with Cp; re-incision of the peno- scrotal wound revealed a bloody effusion, partly organised, surrounded by a thick capsule adhering to the surrounding tissue. A large part of the capsule was cautiously resected and the area was flushed with hydrogen peroxide and Gm solution. The pump was positioned in a subdartoic right scrotal pocket (treatment with Cf, amoxicillin-clavulanic acid).There was no secretion from the wound and after 7 days the patient was able to palpate the scrotum and easily identify the testicles and pump. After a month he was able to have satisfactory sexual intercourse.
Patient, 63 years, heavy smoker, who had Peyronie's disease with shaft deviation. An AMS700 Ultrex was implanted in 2008 (peno-scrotalincision, inter-testicular pump, reservoir in retropubic space, Wilson's manoeuvre to correct the curvature, no aspiration and drainage).The patient was discharged the day after surgery. No complications were found at 3-day follow-up. After the first follow-up the patient did not leave himself time to recuperate and took numerous long car trips. After 5 days he complained that he could not find the scrotal pump due to progressively increased scrotal volume (Figure.6);
No fever or pain. At 21-day follow-up a collection of scrotal fluid was found which impeded location and activation of the pump.US examination revealed a homogeneous, non-corpuscular fluid. It was decided to operate (treatment with Cf and Cp; re-incision of the peno-scrotal wound).The prosthetic pump was found to be surrounded by a clear, transparent fluid with the capsule under tension. The fluid was drained and the capsule was removed; bleeding was controlled. After verifying pump function, aspiration and drainage was performed and the scrotum was sutured. The next day the drain was removed and the patient was discharged.15 days later the cylinder inflation-deflation process began, with easy identification and activation of the prosthetic pump. The patient then enjoyed intense sexual activity until 2017, when a new problem developed.
The same patient now aged 73 and under treatment for hypertension, hyperuricaemia and obstructive pulmonary disease, complained of an acute pelvic pain with an episode of gross haematuria. An abdominal US examination performed in another hospital excluded kidney stones but found that the prosthetic reservoir was adjacent to the bladder and there were hyperechoic images in the bladder. From the following morning the patient presented urinary retention and pain in the distal part of the urethra. He returned to the author's surgery, where it was found that the penile implant was functioning correctly and there were no problems with the reservoir. A bladder US examination did not reveal any obvious stones. Solid, roundish formations obstructing the urethral canal could be seen in the distal part of the urethra. A small meatotomy was performed under local anaesthetic with lidocaine cream and two stones, of 5-7 mm diameter, were extracted (Figure.7).
A Foley CH16 catheter was inserted, which reached the bladder easily without encountering any obstructions. After 7 days of antibiotic therapy with Cp the patient underwent a flexible cystoscopy which revealed benign prostatic hyperplasia, detrusor hypertrophy and no bladder stones.
Patient, 68 years, with AMS700 LGX implanted through the infra-pubic route. There were no problems during surgery. The drain was removed after one day, on discharge. On postoperative day 7 the patient developed a significant oedema of the foreskin, with difficulty in retracting it from the glans and considerable local discomfort; no fever. Treatment with oral cortisone for 10 days led to a moderate reduction in the swelling, enabling the glans to be uncovered. After another 10 days the oedema had resolved fully.
Patient, 53 years, with Peyronie's disease, who had received an AMS700 LGX implant by the infra-pubic route. On postoperative day 7 the patient complained of the development of a significant oedema of the foreskin, impeding its retraction from the glans and causing considerable discomfort. After treatment with oral cortisone for 15 days the oedema normalized.
Patient, 52 years, arterial disease, with Coloplast Titan OTR implanted through the infra-pubic route. There were no problems during surgery. The patient developed a significant oedema of the foreskin 7-10 days after surgery. After 5 days the lymphoedema was still present and antibiotic and cortisone therapy were instigated. After 25 days the patient began using the implant. Five days later the foreskin oedema reappeared, creating problems with shaft rigidity. Cortisone therapy was recommenced, and the patient's condition normalised after 7 days. However, the foreskin lymphoedema returned (Figure.8) after his first sexual relations, tending to normalise after cortisone therapy. At this point a circumcision was performed, thus resolving the problem.
The infra-pubic incision could determine a blockage of local lymphatic drainage.
Patient, 51 years, with vascular dysfunction, poor response to PDEi5s and refusal to use PGE1. An AMS700 LGX IPP was inserted through the peno-scrotal route and the reservoir positioned as normal in the peri- vesical area; inter-testicular pump, no drainage. After 8 days the patient reported feeling an egg-shaped swelling in the right groin. This was found to be the reservoir, which had migrated there spontaneously. The implant worked perfectly although with the cylinders deflated it was possible to see the swelling in the right groin, which reduced in volume on inflation of the cylinders. It was suspected that the transverse fascia had not been fully perforated and that the reservoir had been inserted in a sub muscular position. It was decided to re-operate. The reservoir was emptied by inflating the cylinders and removed through a small infrapubic incision. It was then re-implanted in the retropubic space after opening the transverse fascia. To avoid migration of the reservoir tube it was fixed to the transverse fascia. The incision was closed. After 2 months the situation had regularised. The prosthetic system was performing perfectly after 3 years. The patient is satisfied.
Patient, 56 years, with longstanding Peyronie's disease and erectile dysfunc -tion. An AMS700 CXIPP, 18 cm long with+2.0 cm Rear Tip Extender (RTE) was inserted. After 6 months the patient complained of pain in the glans, which was deformed, due to suspected apical extrusion of the right cylinder (figure.9).
It was decided to perform exploratory surgery following antibiotic prophylaxis with Cf and Cp; this involved sub coronal incision,separation of the glans and liberation of the tip of the right corpus cavernosum, which seemed to have been perforated by the cylinder. The cylinder had not reached the outside and therefore there was no reason to suspect bacterial contamination (Figure.10).
Following a small re-incision at the base on the right of the penis and incision of the tunica albuginea, the right cylinder was extracted and the 2.0 cm RTE was replaced with a 1.0 cm extender. The margins of the apical laceration were removed and the wound was sutured with Vicryl 2/0. A small Marlex patch for hernia repair was affixed as a "hood". The right cavernous cylinder was reinserted. After verifying that there was no apical tension, the glans was fixed above the tip of the corpus cavernosum. The cylinders were kept inflated for 5 days and then alternately inflated and deflated for several hours. After 25 days the patient was authorised to recommence penetrative sex. Seven years later, the patient is satisfied and performs regular penetrative sex.
Patient, 36 years, with diabetes and CVOD. An Implantal PP120 silicone implant inserted in 2003. In 2009 the patient complained of pain in the glans and of being able to feel the tip of the left cylinder (Figure.11).
Surgery was performed to free the tip of the corpus cavernosum perforated by the cylinder, which was extracted, and the area was flushed with antibiotics. It was decided not to implant a new cylinder immediately due to the risk of infection. Aspiration and drainage was inserted and removed after 2 days. After discharge, the patient reported that he had acceptable sexual relations with just one cylinder, and preferred not to undergo further surgery.
Patient, 28 years, with CVOD. The procedure involved preparation with Cf and Cp and peno-scrotalaccess. During Hegar dilation of the right corpus cavernosum the crus of the penis was perforated. There was no perineal haematoma. A RTE was inserted in the crus and, with a small perineal incision, affixed to the tunica albuginea with 2 Vicryl 3/0 stitches. Eurogest 11 mm cylinders were inserted into the corpora cavernosa; 21 cm on the left and 19 cm on the right. No postoperative complications. The patient recommenced sexual activity after one month, and remained satisfied at 5 year follow-up.
Patient, 72 years, with diabetes and hypertension. An AMS 700 Ultrex IPP was inserted in 1999, permitting good sexual function. In 2004, the patient reported pain in the left groin at the base of the penis. A small skin swelling had formed which secreted serous fluid on opening. There was no fever, and the implant was working correctly. It was agreed with the patient to perform surgery to remove a small skin lozenge around the tube. The area was flushed with antibiotics (Cp and Gm).The tube was buried and the skin resutured. There were no local or general complications and the patient recommenced sexual activity after 20 days, with which he was still satisfied in 2011 (27).
Two patients, 58 and 64 years, with diabetes and AMS700 Ultrex IPP, presented scrotal inflammation, purulent reaction, skin erosion and emergence of the prosthetic pump 30 and 36 days after the implant procedure (Figure.12).
The patients' general and local condition led to the full removal of the implants. Neither patient wanted to undergo anew implantation procedure, due in part to financial motives [28, 29].
Patient, 53 years, a surgeon by profession, had been in a relationship with a hospital colleague for 10 years but had never had penetrative sex with her due to inadequate penile rigidity, even with 5PDEis.He specifically requested an IPP, and as quickly as possible. He had not informed his partner of his decision. A ColoplastTitan I, was implanted under standard antibiotic preparation through peno-scrotal incision. Aspiration and drainage were not used. The patient was discharged the next day, and there were no postoperative complications. At the first follow-up at 4 weeks the implant was working well and the patient was ready to use it. After 60 days, the patient stated that his partner's reaction was completely negative, that she had been fully satisfied with their non-penetrative sexual relations and that she was so offended by his actions that she had threatened to leave him. The patient therefore requested the implant's removal. It was suggested that he see a psychologist, but his decision was final. His reasoning was determined: "I'd rather have a woman without an implant than an implant and the risk of not finding another partner."The IPP was removed.
There are various "classic" complications which caused removal of the implant in this author's practice. Two distal extrusions were recorded with semi-rigid and malleable implants, but no case of significant infection. Mechanical breakdowns occurred in 14 of 18 single-component IPP(77.7%) and in 25 of 134 (Figure. 13,14).
3. Results and Discussion
Bacterial infection is still the main problem with penile prosthetic surgery. Despite the meticulous attention to antisepsis of the operating environment and patient, the use of thorough antibiotic prophylaxis, the creation of penile implants with antibiotic coatings, and attempts to minimise operation times, the risk of infection has still not been eliminated, even with procedures performed by highly experienced surgeons (30).No surgeons can consider themselves immune from the risk of infection in penile implants they have performed.
Another limitation of prosthetic surgery is the risk of malfunction, breakage or breakdown of the implant itself. As a general rule, after 15 years an IPP is likely to develop a problem. The lifetime guarantee offered by the manufacturers somewhat attenuates the annoyance of having to replace the implant but does not address the inconvenience and cost of the new procedure itself.
A number of other complications in penile prosthetic surgery can be attributed to the surgeon's inexperience. While almost all surgeons will abide by the suggestions of their more expert colleagues when performing their first few procedures, their inexperience, indecision and need to repeat non-essential manoeuvres can lead to longer operation times and possibly excessive and negative surgical manoeuvres, movements and actions. This author also experienced some complications such as apical and crural extrusion, dislocation of the corpora cavernosa and perforations of the septum during his early surgical career. After gaining more experience, patients with complex clinical situations who would in the past have been sent to more comprehensive facilities, were also accepted.
From the author's limited but not negligible experience, it can be affirmed that not all infections must be considered an automatic cause for removal of the implant, as is often argued in the scientific literature; in some cases, antibiotic therapies can be instigated to eliminate the responsible microorganisms, avoiding the risk of generalised sepsis and enabling the "sterilisation" of the implant.
Many problems related to tissue reactions involving the implant's components (extrusion of the cylinders (Figure. 15) or tubes, pump malfunction, involvement of scrotal pumps in reactive and coagulation processes) can be resolved with a new, possibly limited surgical procedure, while bearing in mind the risk of causing further damage.
In all cases, a good surgeon-patient relationship is necessary; a patient who shares with his surgeon any preoperative, perioperative and postoperative concerns about this important procedure enables them both to make the best decisions which take account of the patient's situation, the hospital facilities and the financial costs of the procedure.
References
- Scott FB, Bradley WE, Timm GW. Management of erectile impotence: use of inflatableprostheses. Urology. 1973; 2:80-22.Small MP, Carrion HM, Gordon JA. Small-Carrion penile prosthesis. New implant for management of impotence. Urology. 1975;5:479-86.
- Darouiche RO, Bella AJ, Boone TB, Brook G, Broderick GA, Burnett AL, Carrion , Carson C 3rd, Christine B, Dhabuwala CB, Hakim LS, Henry G, Jones LA, KheraM, Montague DK, Nehra A. North American consensus document on infection of penile prostheses. Urology. 2013;82:937-42.
- Selph JP, Carson CC 3rd. Penile prosthesis infection: approaches to prevention and treatment. UrolClin North Am. 2011;38:227-357
- Schoepen Y, Staerman F. penile prostheses and infection. Progr Urol. 2002;12:377-83
- Silverstein AD, Henry GD, Evans B, Psmore M, Simmons CJ, Donatucci CE. Biofilm formation on clinically noninfected penile prostheses. J Urol. 2006;176:1008-11
- Wilson SK, Costerton JW. Biofilm and penile prosthesis infections in the era of coated implants: a review. J Sex Med. 2012;9:44-53
- Henry GD, Donatucci CF, Conners W, Greenfield JM, Carson CC, Wilson SK, Delk J, lentz AC, Cleves MA, Jennermann CJ, Kramer AC. An outcomes analysis of over 200 revision surgeries for penile prosthesis implantation; a multicenter study. J Sex Med.2012; 9:309-15
- Minervini A, Ralph DJ, Pryor JP. Outcome of penile prosthesis implantation for treating erectile dysfunction:experience with 504 procedures. Br J Urol.2006;97:129-33
- Al-Reshaid RA, Madbouly K, Al-Jasser A. penile abscess and necrotizing fasciitis secondary to neglected false penile fracture. Urol Ann. 2010;2:66-8
- Sadeghi-Nejad H,IlbeigiP,WilsonSK,Delk JR, Siegel A, Seftel AD, Shannon L, Jung H. Multi-istitutional outcome study on the efficacy of closed-suction drainage of the scrotum in three-piece inflatable penile prosthesis surgery. Int J Impot Res. 2005; 17: 535-8.
- Garber BB, Bickell M. Delayed postoperative hematoma formation after inflatable penile prosthesis implantation. J sex Med. 2015;12:265
- Morey AF. Outcomes of abdominal wall reservoir placement in inflatable penile prosthesis implantation: a safe and efficacious alternative to the space of Retzius. J Urol. 2015;193:251
- Simon R, Hakky TS, Henry G, Perito P, Martinez D, Parker J, Carrion RE. Tips and tricks of inflatable penile prosthesis reservoir placement: a case presentation and discussion. J Sex Med. 2014;11:1325-33
- Hakky T, Lentz A, Sadeghi-Nejad H, KheraM.Levine LA, Hoeh MP. Review of penile prosthetic reservoir: complications and presentation of a modified reservoir placement technique. J Sex Med. 2012;9:2759-69
- Chung PH, Morey AF, Tausch TJ, Simhan J, Scott JF. High submuscular placement of urologic prosthetic balloons and reservoirs: 2-year experience and patient-reported outcomes. Urology. 2014;84:1535-8
- Ball TP Jr. Surgical repair of penile "SST"deformity. Urology. 1980;15:603-4
- Tran CN, Boncher N, Montague DK, Angermeier KW. Erosion of inflatable penile prosthesis reservoir into neobladder. J Sex Med. 2013 sept; 10:2343-615.
- Wilson SK, Delk JR 2nd. Prevention and treatment of complications of inflatable prosthesis surgery: a review article. Arch Esp Urol.1996;49:306
- Mulcahy JJ. Current approach to the treatment of penile implant infections. TherAdvUrol, 2010;2:69-75
- Mulcahy JJ. Penile prosthesis infection: progress in prevention and treatment. CurrUrol Rep. 2010;11:400-4
- Carson CC 3rd. Efficacy of antibiotic impregnation of inflatable Penile Prosth -eses in decreasing infection in original implants. J Urol. 2004;171:1611-4
- McKim SE, Carson CC 3rd. AMS700 inflatable penile prosthesis with Inhibizone. Expert Rev Med devices, 2010;7:311-7
- Dhabuwala C. In vitro assessment of antimicrobial proprerties of rifampicin- coated Titan Coloplast penile implants and comparison with Inhibizone.J Sex Med. 2010;7:3516-9
- Wilson SK, Salem EA, Costerton W. Anti-infection dip suggestions for the Coloplast Titan Inflatable penile prosthesis in the era of the infection retardant coated implant. J Sex Med. 2011;8:2647-54
- Pozza D, Pozza M, Musy M, Pozza C. 500 penile prostheses implanted by a surgeon in Italy in the last 30 years. Arch Ital UrolAndrol. 2015;87:216-21
- Morales A. Tubing erosion of an inflatable penile prosthesis long after implantation. Sex Med. 2014;2: 103-23.
- Christodoulidou M, Pearce I. Infection of penile Prostheses in patients with diab etes mellitus. Surgical Infections.2016;1:2-4
- Bodin T, Bruyere F. Prothesepenienne: revue de la literature des complications infectieuses post operatoires. Progresen Urologie. 2015;7:381-6
- Henry GD, Kansai NS, Callaway M, Grisby T, Henderson J, Noble J, Palmer T, Cleves MA, Ludlow JK, Simmons CJ, Mook TM. Centers of excellence concept and penile prostheses: an outcome analysis. J Urol. 2009;181:1264-8