Information
Journal Policies
ARC Journal of Urology
Volume-1 Issue-1, 2016
Abstract
Background: Benign prostatic hyperplasia (BPH) is the most common problem for men older than age 50, and up to 90% of men older than 80 suffer from this disorder. Benign tumor, by pressing the bladder and the urethra, causes lower urinary tract symptoms (LUTS) that interfere men’s quality of life. The aim of this study was to find out if Thermobalancing therapy is effective and safe to treat the symptoms of BPH.
Methods: During a 2-yr period, 124 men older than 55 with LUTS and the prostate volume (PV) up to 60 mL received Thermobalancing therapy enabled by therapeutic device. Before and after 6-months of treatment were investigated the International Prostate Symptom Score (IPSS), including quality of life (QoL) index, ultrasound measurement of PV and uroflowmetry maximum flow rate (Qmax). Also the dynamics of the same parameters were studied in men with BPH and the PV level over 60 mL. However they were observed during the longer period of time, up to one year.
Results: After treatment the PV level reduced (P <0.001), increased Qmax (P <0.001), improved QoL and diminished IPSS (P <0.001). Furthermore, the dynamics of clinical parameters in men with PV over 60 mL have shown positive results in PV, Q-max and IPSS as well. No side effects were observed. The dynamics of the same measurements in the control-group comprised 124 men who did not receive treatment have shown negative outcomes.
Conclusions: The observed positive effect of therapeutic device, termed Dr Allen’s Device, for BPH has allowed us to recommend Thermobalancing therapy as a new safe physiotherapeutic solution for men with enlarged prostate.
2.KEYWORDS
3.BACKGROUND
4.MATERIALS AND METHODS
5.RESULTS
6.DISCUSSION
7.CONCLUSION
8.REFERENCES
AUTHOR DETAILS
Simon Allen
Fine Treatment
29 Rewley Road, Oxford, OX1 2RA, United Kingdom
[email protected]
KEYWORDS
enlarged prostate, bph treatment, prostate enlargement, thermobalancing therapy, prostate natural treatment, lower urinary tract symptoms, bph cause, clinical trial
BACKGROUND
According to The National Institute of Health, benign prostatic hyperplasia (BPH) is the most common prostate problem for men older than age 50. In 2010, as many as 14 million men in the United States had lower urinary tract symptoms suggestive of BPH, about 50% of men between the ages of 51 and 60 and up to 90% of men older than 80.(1) Current estimates are that the number of individuals 80 years and older in the US will rise from 9.3 million in 2000 to 19.5 million in 2030, an increase of over 100%.(2) BPH and bladder outlet obstruction (BOO) have substantial adverse effects on the public health in all counties, including India. Despite widespread use of medical therapy, BPH remains, on a population level, associated with a substantial incidence of BOO-associated adverse events, including LUTS, urinary infections, bladder calculi, urinary retention and acute renal failure.(3)
Larger prostate volumes were positively associated with increased age. The total prostate volume (mL) in average at 40–49 years = 28; at 50–59 years = 30.8; at 60–70 years = 35.0. The mean length of prostate increased faster than the height and width, especially after the age of 60 years. These equations and models can facilitate further studies about prostate growth and may enable early diagnosis of BPH.(4) Some experts have believed that hormones, particularly testosterone, to play a permissive role in the development of BPH. This means that androgens have to be present for BPH to occur.(5) However castrated boys do not develop BPH when they age. In the following study of 26 eunuchs from the palace of the Qing dynastystill living in Beijing in 1960, the prostate was impalpable (could not be felt) in 81%.(6)
In the last decade, the pathogenesis of BPH began to consider from the perspective of vascular dysfunction,(7) chronic ischemic tissue,(8) and increasing the pressure in the prostate gland.(9)
Dr. Allen’s research on the Origin of Diseases has helped him to identify the causal root of prostate enlargement, namely capillary expansion. This conclusion is based on 2 functional physiological properties of capillaries which are activated by an irritating factor, i.e. a trigger; indeed this peculiarity of capillaries explains the cause of chronic internal diseases. Constriction of capillaries in response to an irritating trigger develops local micro-hypothermia. It is this focus of hypothermia, which in turn becomes a constant irritant maintaining illness, i.e. making a disease chronic. In response to irritation (i.e. a trigger-initiator and later focus of hypothermia) and in order to eliminate them, the blood flow increases through the spontaneous expansion of the capillary net locally. The formation of new capillaries is essentially the growth of the excess tissue that leads to an increased pressure inside the organ.
In other words, extra tissue becomes irritated as a response to different factors, such as cold, stagnation of its own secretion or infection, which leads to prostate growth. As a consequence, this essential organ ages prematurely. In order to terminate prostate growth and to reverse prostate enlargement, the improvement of blood circulation locally becomes the primary objective.(10)
Widely used BPH medications cannot reach prostate and provide symptomatically relief in its acute stage. Moreover BPH drugs and prostate surgeries(11) may be responsible for different side effects. For instance, the case studies published by the Harvard Medical School confirm complications arising from two BPH drugs: tamsulosin (Flomax) which may suddenly make men become lightheaded or develop retrograde ejaculation, and terazosin (Hytrin) which can be responsible for the acute urinary retention.(12) Dr. Irwig has confirmed persistence of erectile dysfunction after discontinuation of treatment with Propecia (finasteride). That is why a “watchful waiting” stage for BPH is recommended.(13)
The data above shows that in the etiology and pathogenesis of BPH vascular factor plays a decisive role, also BPH medications and surgeries are not safe that interfere men’s quality of life. In order to improve men’s wellbeing Thermobalancing therapy enabled by therapeutic device has been introduced. A 2-year controlled trial has shown the efficacy of thermobalancing therapy for men with BPH.(14) In this study we present some documents of the clinical trial and also the dynamics of the clinical symptoms in a man with the prostate volume over 60 mL.
MATERIALS AND METHODS
The observational clinical controlled study was used. Enrolment began on April 2013 in the Department of Urology at the Yerevan State Medical University and led by Professor Ivan Aghajanyan. The Ethics Committee of the Yerevan State Medical University has approved the clinical study on Thermobalancing therapy. Comparing men with BPH who received treatment with therapeutic device for 6 months and the control group on the watchful waiting stage, studied the effectiveness of Thermobalancing therapy. Dynamics of the symptoms and the indicators in each group were evaluated in comparison to their data in the beginning and end of the treatment.
The baseline evaluations included complete physical examination, medical history, DRE, serum biochemistry, and PSA measurements, electrolytes, urine and renal function tests. Evaluations were made at baseline and 6 months after the treatment. IPSS-QoL scored as follow: delighted = 0, pleased = 1, mostly satisfied = 2, about equally satisfied and dissatisfied = 3, mostly dissatisfied = 4, hopeless = 5 and poor = 6. PV was measured at baseline and at 6 months after the treatment by ultrasonography (US-9000E2 ultrasound scanner, Rising Medical Equipment Co. Ltd, Beijing, China) and uroflowmetry (maximum urinary flow rate - Qmax, mL/s) was used for the measurement of the rate of urine flow parameters (Sanuro2UL, Santron Meditronic, Maharashtra, India). The standard ellipsoid formula length×width×height×0.52 was used to determine prostate volume.
226 men were examined from April 2013 to December 2014 in total, and 124 patients selected for the clinical trial. 80 men were excluded, as their prostate volume was over 60 ml or they had severe comorbidities; 10 preferred operation; 4 were suspected prostate cancer; 8 did not attend to the following examinations. Men in treatment-group after the screening were given therapeutic device, termed Dr. Allen’s Device, see figure 1.
Inclusion criteria: Men were eligible for enrollment if they were over the age of 55, in the absence of acute prostatitis, at the level of prostate-specific antigen (PSA) that is not more than 4 m.mol/l. It did not matter if they were treated at the time of enrollment with medicines. However, after the use of therapeutic device other treatments were cancelled gradually. Exclusion criteria: PV greater than 60 ml, co-morbidities, such as diabetes, heart failure, cancer, etc.
In this study we also present an individual data of a man with prostate volume 154 ml who used Dr Allen’s Device for over 6-months.
The study’s quantitative variables are expressed as mean values, standard error, and minimum and maximum values, whereas the qualitative variables are expressed as numbers and percentages. For numerical data, independent sample t-tests were performed; for comparisons of before and after treatment, the non-parametric statistical hypothesis test by Wilcoxon was used. Statistical analysis was done by Statistical Package for the Social Science (SPSS Inc, Chicago, Illinois, USA) version 18.0.
RESULTS
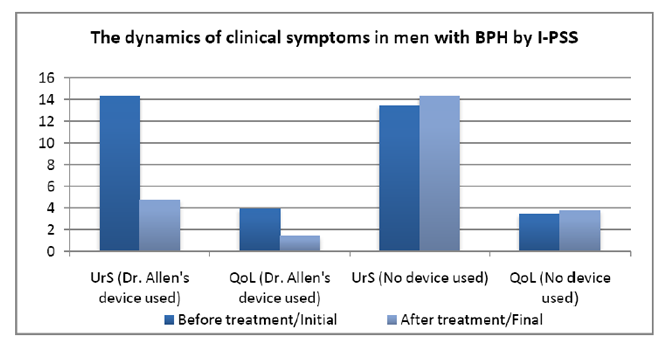
In the control group, the mean IPSS-UrS increased from 13.45 ± 3.254 to 14.35 ± 3.396, whereas in the treatment group the mean IPSS-UrS decreased from 14.33 ± 3.399 to 4.73 ± 2.754 at the end of the observation period. For the control group, the z value was 6.018 with a P value (P <0.001). For the treatment group, the z value was 9.674 with a significance level (P <0.001). This indicates that the
treatment with Therapeutic Device decreased the urinary symptoms significantly, while in absence of treatment the symptoms increased significantly.
In the control group, the mean IPSS-QoL increases from 3.43 ± 0.956 to 3.76 < 0.983, whereas in the treatment group the mean IPSS-QoL decreases from 3.91 < 0.755 to 1.39 < 1.110. For the control group, the z value was 5.286 with a P value (P <0.001). For the treatment group, the z value was 9.672 with a P value (P <0.001). These results indicated that the treatment with Therapeutic device improved the QoL while in the control group the QoL worsened.
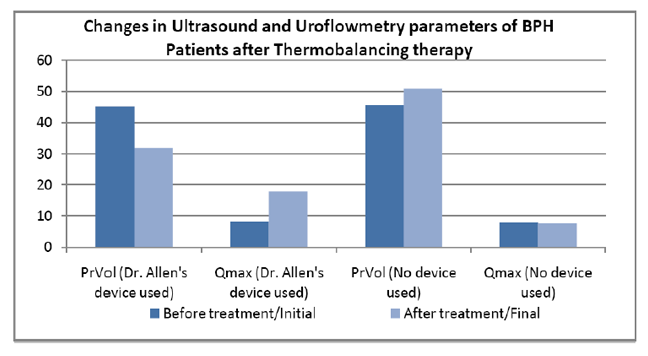
In the control group the mean prostate volume increased from 45.54 to 50.85 mL, whereas in the treatment group the mean prostate volume decreased from 45.19 to 31.86 mL. For the control group, the z value is – 8.727 at the significance level (P <0.001). So there was a statistically significant increase in the prostate volume in the control group. For the treatment group, the z value is – 9.669 at the significance level (P <0.001). So the treatment with therapeutic device reduced the PV level significantly, whereas in the no treatment group the PV level increased.
In the control group, the mean Qmax decreased from 7.95 ± 2.871 to 7.7 ± 2.695 mL/s, where as in the treatment group the mean Qmax increased from 8.10 ± 3.041 to 17.73 ± 4.392 mL/s. For the control group, the z value was 1.929 and the P value .054 (> .05), indicating no statistically significant difference. For the treatment group, the z value is 9.621 at the significance level (P <0.001), indicating a significant increase in the Qmax. Therefore, our results demonstrate that the therapeutic device increased the uroflowmetry Qmax significantly in BHP patients, whereas the control group had no significant difference in the uroflowmetry Qmax.
This case shows the use of the therapeutic device decreased the PV level and increased Q-max significantly in 7-months, consequently was observed improvement in IPSS.
Patients feel no side effects during the clinical trial. Besides all of this, the important factor is the cost of a new treatment compared to the cost of the standard treatment options..
DISCUSSION
This study results have demonstrated that Thermobalancing therapy decreased IPSS, reduced the PV level, increased the uroflowmetry Qmax and improved QoL significantly. These positive outcomes indicate that thermobalancing therapy is effective for BPH.
BPH is historically believed to be a consequence of the aging process and the elimination of the negative impact of an enlarged prostate in men should be done with the help of medical or surgical intervention. At the same time, medications used for the treatment of BPH do not provide sufficient performance. For example, a study showed that half (52.8%) of men with BPH were dissatisfied with the results of medical treatment conducted according to current international guidelines for BPH.(15) In addition, most commonly used BPH medications have side effects, especially, especially in the long-term use.(16) Surgical treatment of prostate may also be accompanied by new challenges. Thus, the results of a survey of sexually active men after three different laser surgeries from 2005 to 2010, concluded that these surgical techniques can have a negative impact on sexual function, and patients with normal preoperative sexuality are more at risk.(17)
In the last decade, the opinion of the necessity of medical/surgical treatment of BPH has been challenged. BPH/LUTS should not be viewed as an inevitable disease of older people but part of the aging process which can be prevented.(18) Thermobalancing therapy can play a crucial role in the prevention of BPH development, particularly when the problem is diagnosed. Thermobalancing therapy is entirely different than common heating treatments because it regulates the affected organ’s temperature locally, maintaining it within the normal body temperature range. All other treatments with imposed heat can be damaging, because the high temperatures destroy delicate cells of the already stressed organ. For example, any temperature above 104 Fahrenheit (or 40C) can result in the death of the living organism. On the other side, low temperatures decrease cellular metabolism and, as a result, interfere with natural replenishment and healing.
Thermobalancing therapy is enabled by therapeutic device which applies the thermoelement tightly to the skin in the projection of the affected organ, and overcomes the skin barrier spreading energy inside the body. One may suggest that similar treatments have been available on the market for a long time (e.g. wool or synthetic fabric clothes) and that many patients with chronic pain wear such devices for a long time. This is not the case, however, as no other treatment method and material have been able to overcome the skin barrier delicately and precisely. Thermobalancing therapy is the only external non-invasive treatment that targets pathological nidus continuously for a prolonged period of time, i.e. for days, months or even years, maintaining the accumulated temperature. We believe that the use of therapeutic device by keeping the temperature in the projection of the prostate gland acts on micro-focus of hypothermia and ischemia in it, removing the vicious cycle of spontaneous growth of capillaries in response to a trigger, micro-hypothermia, thereby relieving the BPH symptoms.
CONCLUSION
A study involving 124 men with BPH, to whom the therapeutic device was administered exclusively as a mono-therapy, has confirmed the effectiveness and safety of Thermobalancing therapy. Thoroughly examined before and after a 6-month treatment period, the patients reported a significant improvement to the disturbing lower urinary tract symptoms (LUTS). Their treatment results compared favourably to other patients, also 124 men, in the control group. This study and a case study support the concept that changes in the microcirculation of blood and hypothermia play a role in the development of BPH and that Thermobalancing therapy can be a new opportunity for secure effective physiotherapeutic intervention in BPH. The significant reduce of prostate volume under Thermobalancing therapy makes necessity to study the changes in the prostate gland precisely, possibly by using a magnetic resonance imaging (MRI).
REFERENCES
- Deters LA. Benign prostatic hypertrophy. Emedicine website. http://emedicine.medscape.com/ article/437359-overvie
- Centers for Disease Control and Prevention (CDC). Trends in aging-United States and worldwide. MMWR Morb Mortal Wkly Rep. 2003;52(6):101-4,106
- Patel ND, Parsons JK Epidemiology and etiology of benign prostatic hyperplasia and bladder outlet obstruction, Indian J Urol. 2014 Apr; 30(2):170-6
- Shi-Jun Zhang, Hai-Ning Qian, Yan Zhao et al, Relationship between age and prostate size, Asian J Androl. 2013 Jan; 15(1): 116–120
- BhasinS, Singh AB, Mac RP et al, Managing the Risks of Prostate Disease During Testosterone Replacement Therapy in Older Men: Recommendations for a Standardized Monitoring Plan, Journal of Andrology, 2003, 24, 3, 299–311
- Wu CP, Gu FL, The prostate in eunuchs, Prog Clin Biol Res. 1991;370:249-55.
- Shimizu S, Tsounapi P, Shimizu T, et al, Lower urinary tract symptoms, benign prostatic hyperplasia/benign prostatic enlargement and erectile dysfunction: Are these conditions related to vascular dysfunction? Int J Urol, 21(9):856-64, September 2014.
- Andersson K, Nomiya M, Yamaguchi O, Chronic Pelvic Ischemia: Contribution to the Pathogenesis of Lower Urinary Tract Symptoms (LUTS): A New Target for Pharmacological Treatment? LUTS: Lower Urinary Tract Symptoms, 2014, DOI: 10.1111/luts.12084
- Cohen PG, Abdominal obesity and intra-abdominal pressure: a new paradigm for the pathogenesis of the hypogonadal-obesity-BPH-LUTS connection, Hormone Molecular Biology and Clinical Investigation, 2012, 11-1, 317–320
- Allen S, Adjani A 2009 Therapeutic Device and Method, US 20110152986 A1, http://www. google.com/patents/US20110152986
- Ben-Zyi T, Hueber PA, Valdivieso R, et al, Urological resident exposure to transurethral surgical options for BPH management in 2012–2013: A pan-Canadian survey, Can Urol Assoc J. 2014 Jan-Feb; 8(1-2): 54–60
- Harvard Med School, Prostate Knowledge, 2007, Your benign prostatic hyperplasia medication: When to consider a change, http://www.harvardprostateknowledge.org/your-benign-prostatic-hyperplasia-medication-when-to-consider-a-change
- Irwig MS, Kolukula S., Persistent sexual side effects of finasteride for malepattern hair loss, J Sex Med. 2011 Jun;8(6):1747-53
- Allen S, Aghajanyan IG Benign Prostatic Hyperplasia Treatment with New Physiotherapeutic Device, Urol J. 2015 Nov 14;12(5):2371-6
- Fourcade RO, Lacoin F, Rouprêt М, et al. Outcomes and general health-related quality of life among patients medically treated in general daily practice for lower urinary tract symptoms due to benign prostatic hyperplasia. World J Urol. 2012;30:419-26
- Gacci M, Ficarra V, Sebastianelli A, et al. Impact of Medical Treatments for Male Lower Urinary Tract Symptoms Due to Benign Prostatic Hyperplasia on Ejaculatory Function: A Systematic Review and Meta- Analysis. J Sex Med. 2014;11:1554-66
- Elshal AM, Elmansy HM, Elkoushy MA, Elhilali MM. Male sexual function outcome after three laser prostate surgical techniques: a single center perspective. Urology. 2012;80:1098-104.
- Corona G, Vignozzi L, Rastrelli G, Lotti F, Cipriani S, Maggi M. Benign Prostatic Hyperplasia: A New Metabolic Disease of the Aging Male and Its Correlation with Sexual Dysfunctions. Int J Endocrinol. 2014;2014:329456