Information
Journal Policies
Functional Outcomes and Rates of Complications of Open Reduction and Internal Fixation of Mason Type III Radial Head Fractures
Bougiouklis Dimitrios1*, Psychogyios N. Vasileios2
2.Fifth Department of Orthopeadics–Unit of Hand Surgery and Microsurgery, General Hospital “Asklepieion” Voulas, Athens, Greece.
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Objective: To evaluate the treatment of patients with these comminuted fractures by open reduction and internal fixation and early mobilization. An additional purpose was to investigate whether, the concomitant elbow dislocation, may influence the final function results.
Methods: From 2007 to 2017, 23 patients (mean age of 32 years) who underwent open reduction and internal fixation for Mason type-III radial head fractures were retrospectively reviewed. In the cases were necessary it was used an autogenous bone graft from the lateral humeral epicondyle. Eleven radial head fractures were isolated injuries, while five fractures were associated with dislocation of the elbow. Two patients had trans-olecranon fracture-dislocation, two had posterior Monteggia fracture, one had a c fracture of lateral condyle fracture, one had a rupture of medial collateral ligament and one had an Essex-Lopresti injury.
Results: The average follow-up was 5 years. All fractures were united, except for one, at an average of 12.7 weeks. In not patient avascular necrosis was noted. The average Broberg and Morrey score was 86.4 (range, 76-92). In two patients, removal of the plates was required because of the fact that the first one developed heterotopic ossification and the second one presented painful crepitation. An ulnar neuropathy developed in one patient, but it was resolved after 4 months postoperatively. The average elbow flexion was 139° (range, 120° to 150°), and the average flexion contracture was 7° (range, 0o to 20°). The average supination was 74° (range, 70° to 87°), and the average pronation was 68° (range, 600o to 80o).
Conclusion: The surgical treatment of comminuted fractures of the radial head has been controversial because there is conflicting evidence supporting resection, prosthetic replacement, and open reduction with internal fixation. The radial head is important to elbow stability and therefore, we consider that even when two or more fracture fragments are present, the primary goal is to fix and preserve the radial head.
Elbow, Radial Head, Comminuted Fracture, Mason III, Internal Fixation,Surgery
1. Introduction
The radial head plays an important role in maintaining elbow stability. The three primary static stabilizers of the elbow are the ulnohumeral articulation, the medial collateral ligament as well as the lateral collateral ligament. Secondary constraints include the radial head, the joint capsule and the common flexor and extensor origins. If the coronoid process or medial collateral ligamentare injured, the radial head becomes a critical stabilizer. The muscles around the elbow, especially the anconeus, biceps and triceps, function as dynamic stabilizers[1].
Radial head fractures have an incidence of 2.5-2.9 per 10.000 per year and account for up to one third of all elbow fractures [2]. Radial head fractures are most often the result from a fall on the outstretched hand with elbow partially flexed and pronated [3]. Amis and Miller correlated elbow fractures to the angle of flexion of the elbow during a fall, the so-called “arc of injury”. They observed that the radial head fractures at a flexion angle between Oo and 80o. Radial head fractures are commonly classified under the Mason classification system: type I, fissure fractures or marginal sector fractures without displacement; type II, partial articular fractures with displacement; and type III, comminuted fractures involving the whole head of the radius. Mason type III fractures are difficult to treat. Proper treatment of these fractures is essential in order to regain the stability and functional activities of the elbow and minimize the consequences. The treatment of Mason type III fractures generally requiring plating if possible, or replacement of radial head, or its excision. During recent years, the resection of the radial head is seldom adopted due to complications of instability of the elbow joint, muscle force regression, proximal radius dislocation and long-term arthrosis. Improvements in operation techniques and implants, such as low-profile mini-plates, have increased the appeal of open reduction and internal fixation treatment (ORIF) [4]. The goals of ORIF are to obtain an anatomic reduction and stable fixation, but bone nonunion and fixation failure are the most common complications which can lead to chronic pain and dysfunction of the elbow joint [5].
Our algorithm for the management of Mason type III radial head fractures includes an initial assessment in an effort to preserve it, especially in young and active patients. The purpose of this retrospective study was to evaluate the treatment of patients with these comminuted fractures by open reduction and internal fixation, collateral ligament repair and early mobilization. An additional purpose was to investigate whether, the concomitant elbow dislocation, may influence the final function results.
2. Materials And Methods
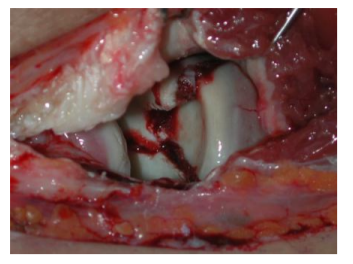
Between 2007 and 2017, we evaluated 23 patients suffering from Mason type III radial head fractures and treated with open reduction and internal fixation using low-profile mini-plates and screws and, if necessary, using autogenous bone graft from the lateral epicondyle of the humerus. There were 18 men and 5 women, with a mean age of 32 years (range 21-63). Seventeen cases regarding the dominant extremity. The mechanism of injury was a fall from a height in six patients, a traffic accident in nine patients, and a sport injury in eight patients. Eleven radial head fractures were isolated injuries, while five fractures were associated with simple dislocation of the elbow [Figure.1]. Two patients had trans-olecranon fracture-dislocation, two had posterior Monteggia fracture, one had a concomitant fracture of lateral condyle fracture, one had a rupture of medial collateral ligament and one had an Essex-Lopresti injury.
During the period of the study, we also performed prosthetic replacement of the radial head in 11 patients and radial head resection in 3 patients for the management of comminuted fractures that could not be reliably treated with ORIF. Of the 23 patients treated by ORIF, in 12 of these we used an autogenous bone graft.
After reviewing the patients’ medical records and radiographs in our medical databases, we invited the patients to the hospital for clinical and radiographic evaluations. Whitten informed consent was required for participation in this study. No patient was lost to follow-up.
The mean time interval between injury and operation was 4 days (range, 1-10). Repair of lateral collateral ligament was carried out in five cases, while the medial collateral complex was repaired in one patient. Internal fixation of seven patients was combined with autogenous bone graft from the lateral epicondyle of the humerus.
A brachial plexus block was used in all patients. With the patient in the supine position and under pneumatic tourniquet control, the fracture was approached through a long Kocher lateral approach which was beginning at the lateral epicondyle ending distal to the radial neck. In the cases with trans-olecranon fracture-dislocation and in those with Monteggia fractures, we realized a midline longitudinal dorsal incision.
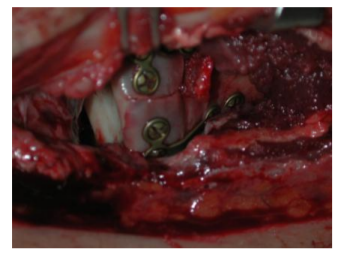
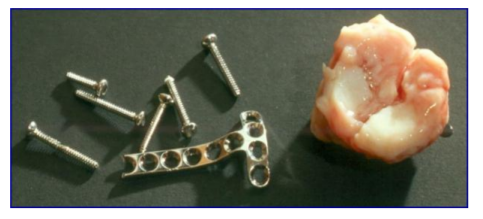
The radial head and lateral collateral ligament were exposed and checked. A longitudinal incision was made through the annular ligament and capsule, along the anterior part of the lateral collateral ligament. Thus, the longitudinal continuity of the lateral ligament was not disturbed. The fracture was identified and all pieces of the radial head were found, after irrigation of intra-articular hematoma [Figure.2]. Care was taken to protect the sinovium and periosteum overlying the fragments to preserve the vascular supply and facilitate reduction [6]. Once reduced, the fracture fragments were temporarily fixed with 1mm K-wires. Two K-wires were placed from one fragment into the shaft obliquely. The other fragments (usually two) were then similarly reduced and held with two more K-wires. Bones grafts from the lateral epicondyle were implanted in the bone defect between the radial head and neck if necessary. The donor site was located in the lateral metaphysis of the humerus and far away from the origins of the lateral collateral ligament and common extensor tendon. Both cancellous and corticocancellous bone were taken, which size was commensurated with the injury. The reconstructed radial head was definitively fixed with suitably moulded plates [Figure.3]. A 2 mm mini-screw was inserted into each hole after predrilling to 1.5 mm. Finally, the K-wires were removed. The plates were placed on the no-articular portion of the radial head (“safe zone”). The non-articular portion of the radial head exhibited a thinner band of yellowish cartilage relative to the wider, white, glistening cartilage of the articular portion of the radial head [7]. Sometimes a fragment was too small to be fixed with a plate and could only be fixed with 24 mm or 35 mm mini-screws.
Associated fractures were concomitantly fixed and the radial head and proximal radioulnar joint were examined by fluoroscopy to ensure extra-articular screw placement. The capsule and annular ligament were closed with absorbable sutures. In cases where the lateral collateral ligament was avulsed from the lateral condyle, it was reattached with an anchor. If there was associated injury to the medial collateral ligament, it was repaired with non-absorbable sutures or an anchor through a medial approach. We checked the stability of the medial collateral ligament by flexing the elbow at 30° and applying valgus stress after internal fixation. Thorough irrigation was done and wound was closed in layers [Figure.4].
Postoperative immobilization in a splint was performed for 3 weeks with the elbow at 90o. Active and active-assisted range of motion exercise was initiated at 4 weeks after surgery. We did not use indomethacin or irradiation as prophylaxis against heterotopic ossification.
The clinical examination and radiographic evaluations were performed by one of the authors. Flexion and extension of the elbow and wrist, with the forearm in a neutral rotation, and the range of pronation and supination were measured. A standard long-limb goniometer was used to measure the angles of motion. The outcome was graded using the elbow functional rating index described by Broberg and Morrey (8). Functional rating index scores were converted to a qualitative score as follows: 95 to 100 points, excellent; 80 to 94 points, good; 60 to 79 points, fair; and 0 to 59 points, poor; a fair or poor result was considered unsatisfactory. Follow-up radiographs including anteroposterior and lateral projections of the elbow, were used to assess fracture union, congruity, post- traumatic osteoarthritis and hardware-related problems. Failure of fixation and nonunion requiring a second operation to excise the radial head was considered an unsatisfactory result. Recovery of less than 100o of forearm rotation with an otherwise satisfactory functional result was also considered a poor result. Radiographic signs of arthrosis were assessed according to the criteria of Broberg and Morrey [8].
The data were analyzed using Microsoft excel. Descriptive statistics (mean, standard deviation and proportions) were used to summarize the study variables. The 95% confidence intervals (CI) for difference of mean were used. Chi-square test was used to observe an association between the qualitative study outcome variables. Unpaired t-test was used for analysis of quantitative data. A two-sited p-value of less than 0.05 was considered statistically significant.
3. Results
The average follow-up was 5 years. No complications occurred in the donor site area. All fractures were united, except for one, at an average of 12.7 weeks. In this case where the fracture was not healed, revision was realized 7 months later, with the use of bone graft. At the most recent evaluation, the fracture was healed. In not patient avascular necrosis was noted. In the series, the average Broberg and Morrey score was 86.4 (range, 76-92). In two patients, removal of the plates was required because of the fact that the first one developed heterotopic ossification and the second one presented painful crepitation [Figure.5]. An ulnar neuropathy developed in one patient, but it was resolved after 4 months postoperatively. Three another patients descripted pain a rest that required the occasional use of analgesic. Nineteen patients had no evidence of degenerative change (grade 0), 3 patients had grade 1 changes, and 1 patient had grade 2 changes. All four patients (grades 1 and 2) had Mason type-III fractures according to the scale of Broberg and Morrey for the radiographic assessment of posttraumatic arthritis.
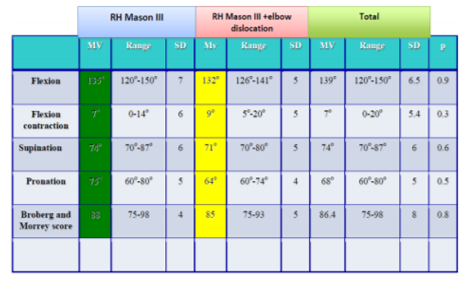
In the patients who suffered by isolated Mason type-III fracture, the average elbow flexion was 135° (range, 120° to 150°), and the average flexion contracture was 7° (range, 0o to 14°). The average supination was 74° (range, 70° to 87°), and the average pronation was 75° (range, 60° to 80°) [table 1]. All patients recovered more than 100° of forearm rotation. According to the system of Broberg and Morrey, the average score was 88 points (range, 75-96) [Figure.6].
In the patients who suffered by Mason type-III fracture-dislocation, the average elbow flexion was 132o (range, 126° to 141°), and the average flexion contracture was 9° (range, 5o to 20°). The average supination was 71° (range, 70° to 80°), and the average pronation was 64° (range, 60° to 74°) [table 1]. The mean Broberg and Morrey score was 85 points (range, 75-93).
4. Discussion
Fractures of the radial head are among the most common elbow fractures in adults and accounts for 15% to 45% of injuries around elbow joint. Since the radial head is an important lateral column stabilizer, for the treatment of its fractures we should attempt to be preserved. The treatment of Mason type III fractures and those with associated ligamentous damage or dislocation is challenging. The management options for these fractures include simple excision, prosthetic implant replacement and open reduction and internal fixation. The preferred surgical treatment is still a matter of debate. Excision of the radial head had been an accepted form of treatment for Mason type III fractures. However, excision of the radial head may be associated with proximal radial migration and consequent disorders in the wrist [9]. Some patients have reported weakness after excision of the radial head on long-term follow-up [10]. Radial head fractures combined with injury of medial collateral ligament should not be treated by radial excision [11]. Therefore, it is important to restore radiocapitellar contact through repair or replacement of the radial head when treating unstable fracture-dislocations of the forearm or elbow, such as those associated with injury of the interosseous ligament of the forearm (an Essex-Lopresti lesion) or posterior dislocation of the elbow with fractures of the radial head and coronoid process (the terrible triad of the elbow) [12]. Prosthetic replacement of the radial head is another alternative and is commonly performed when the head is fractured into more than three displaced fragments. Prosthetic replacement provides immediate stability without the risk of early collapse [13]. However, there have been difficulties with prosthetic size and design, and the long-term effects of contact between a metal prosthesis and the capitellar articular cartilage are not known [14]. Flinkkilä et al.[15] reported that loosening of press-fit radial head prostheses was found in 12 of 37 patients (32.4%). van Riet et al.[16] reported that 47 elbows underwent removal of a failed metallic radial head replacement.
With current advances and better understanding of elbow biomechanics and with the advent of new implants, osteosynthesis of radial head is emerging as the technique of choice, even for comminuted fractures. ORIF is the preferred treatment method, particularly in young and active patients. Both biomechanical and clinical studies have proven that preservation of the radial head haw a positive impact on elbow stability [17]. On the other hand, risk of early collapse, nonunion, and avascular necrosis can be seen after open reduction and internal fixation [18]. Heim et al.[19] encountered problems with healing or avascular necrosis in 5 of 11 comminuted fractures. Autogenous bone graft is beneficial for both maintenance of reduction and healing of fractures. In the present series, no nonunion or avascular necrosis occurred after ORIF with a bone graft from the lateral epicondyle. However, bone grafting has not been widely used in combination with ORIF for the treatment of radial head fractures, and different donor site have been reported in the literature [20]. We prefer autografting from the lateral epicondyle of the humerus. The reasons for this choice are as follows: a) taking bone chips from the same incision is convenient and induces less iatrogenic damage; b) preparation of another sterile area for donation is not needed; and c) the procedure is safe and has no adverse effects on elbow function.
Reconstruction of the radial head is usually performed using a mini-screws or mini-plate system and has more recently been conducted with absorbable pins for Mason type-II fractures [21]. Koslowsky et al. [22]reported a reconstruction rate of 100% and good clinical results using fragment fixation system wires with a diameter of 1.6 mm in 14 Mason type-III and 11 type-III fracture-dislocations. However, during mini-plate fixation, displacement of the radial head from the neck could lead to poor reduction. Furthermore, the presence of a minimal misalignment of the plate after removal of the temporary K-wires, used for the initial reduction, may put the construct under tension. Finally, incorrect contouring of the plate could bring as a result a poorer reduction, with the largest incongruity between the radial head and neck. Actually, successful reconstruction of the head alone would not restore full function, and correct alignment of the reconstructed redial head to the neck is the key pre-requisite for normal rotation in the proximal radioulnar joint. In our series T-shaped mini-plate and screws were used when the fracture fragments were large enough to accept the screw heads. It was not always possible to join the comminuted radial head to the shaft when the fracture extended into the neck and fragments were small. Radial head plates were used under these circumstances. When placing the plates and screws on the surface of the radial head and neck, they were placed in the “safe zone,” where they did not impinge on the proximal radioulnar joint during rotation of the forearm.
In 3 of our patients there was chondral leaf from capitellum interposed into radial head fracture fragments. In one more, the presence of the fracture of lateral condyle of the humerus, blocked the reduction. This phenomenon was well defined by Caputo et al.[23]. The complex fractures like Mason type III fractures and Mason type III fractures with dislocation of the elbow may include impacted articular fragments or small fragments with subchondral bone not amenable to any form of internal fixation. Not only do these factors increase the difficulty of surgical fixation, but they also increase the risk of posttraumatic arthritis and joint stiffness. In this study, we excised the small fragments with subchondral bone that were not amenable to any form of internal fixation. If those fragments originated from the important part of the joint, we buttressed it with the plate.
In the present study, we are unable to find statistical differences between Mason type-III fractures and Mason types-III fractures with dislocation of the elbow for the studied parameters (p>0.05). Nineteen patients had no evidence of degenerative change (grade 0), 3 patients had grade 1 changes, and 1 patient had grade 2 changes. All four patients (grades 1 and 2) had Mason type-III fractures according to the scale of Broberg and Morrey for the radiographic assessment of posttraumatic arthritis. We were unable to see any degenerative changes in Mason type-III fractures with dislocation of the elbow. The reason is that the dislocation may prevent cartilage degeneration by transferring trauma energy directly to the bone and ligaments. In the absence of dislocation, energy could be directly transmitted to the cartilage.
In all cases our principal aim was to provide stability of the fracture and elbow and then allow early active mobilization. For this reason, we used bone grafting when there was any doubt about stability. In each case, stability of both collateral ligaments was checked. In the case of any tear, acute repair of collateral ligaments was performed because these ligaments are important for elbow stability. By performing an acute repair of the medial collateral ligament, the surgeon can be confident that earlier mobilization can be instituted.
5. Conclusion
Comminuted fractures of the radial head were more likely to be part of a complex elbow dislocation pattern. The surgical treatment of these fractures has been controversial because there is conflicting evidence supporting resection, prosthetic replacement, and open reduction with internal fixation. Currently, the possibility of using low-profile materials, has made internal fixation sufficient, even small bone fragments. The use of CT scan with three-D reconstruction, we help to plan the treatment. In every operation, we make the preparation for both open reduction with internal fixation and prosthesis. Osteoporosis is the other important factor in making a decision to fix the radial head. However, we consider that even when two or more fracture fragments are present, the primary goal is to fix and preserve the radial head.
References
- O’Driscoll SW, Jupiter JB, King GJ, Hotchkiss RN, Morrey BF. The unstable elbow. Instr Course Lect 2001; 50:89–102.
- Kaas L, van Riet RP, Vroemen J, Eygendaal D. The epidemiology of radial head fractures. J Shoulder ElbowSurg 2010; 19:520–3.
- Amis A, Miller J. Mechanisms of elbow fractures: an investigation using impact tests in vitro. Injury 1995; 26:163–8.
- Ikeda M, Yamashina Y, Kamimoto M, Oka Y. Open reduction and internal fixation of comminuted fractures of the radial head using low-profile miniplates. J Bone Joint Surg Br. 2003;85:1040–4.
- Ring D (2004) Open reduction and internal fixation of fractures of the radial head. Hand Clin 20(4):415–427. doi:10.1016/j.hcl.2004.06.001.
- Businger A, Ruedi TP, Sommer C. On-table reconstruction of comminuted fractures of the radial head. Injury.2010;41:583–8.
- Caputo AE, Mazzocca AD, Santoro VM. The nonarticulating portion of the radial head: anatomic and clinical correlations for internal fixation. J Hand Surg Am. 1998;23:1082–90.
- Broberg MA, Morrey BF. Results of treatment of fracturedislocations of the elbow. Clin Orthop Relat Res 1987;216:109–119.
- Hotchkiss RN. Displaced fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg 1997;5:1–10.
- Janssen RP, Vegter J. Resection of the radial head after Mason type-III fractures of the elbow: follow-up at 16 to 30 years. J Bone Joint Surg 1998B;80:231–233.
- Charalambous CP, Stanley JK, Siddique I, Powell E, Ramamurthy C, Gagey O. Radial head fracture in the medial collateral ligament deficient elbow; biomechanical comparison of fixation, replacement and excision in human cadavers. Injury. 2006;37:849–53.
- Essex-Lopresti P. Fractures of the radial head with distal radio-ulnar dislocation; report of two cases. J Bone Joint Surg 1951;33B:244 – 247.
- Bain GI, Ashwood N, Baird R, Unni R. Management of Mason type-III radial head fractures with a titanium prosthesis, ligament repair, and early mobilization. Surgical technique. J Bone Joint Surg 2005;87A:136– 147.
- Moro JK, Werier J, MacDermid JC, Patterson SD, King GJ. Arthroplasty with a metal radial head for unreconstructible fractures of the radial head. J Bone Joint Surg 2001;83A: 1201–1211.
- Flinkkilä T, Kaisto T, Sirniö K, Hyvönen P, Leppilahti J. Short- to mid-term results of metallic press-fit radial head arthroplasty in unstable injuries of the elbow. J Bone Joint Surg Br. 2012;94(6):805–10.
- van Riet RP, Sanchez-Sotelo J, Morrey BF. Failure of metal radial head replacement. J Bone Joint Surg Br. 2010;92:661–7.
- Geel CW, Palmer AK. Radial head fractures and their effect on the distal radioulnar joint. A rationale for treatment. Clin Orthop Relat Res. 1992;275:79–84.
- Ring D, Quintero J, Jupiter J. Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg 2002;84A:1811–1815.
- Heim U. Kombinierte Verletzungen von Radius und Ulna im proximalen Unterarmsegment. Hefte Unfallchir. 1994;241:61–79.
- Luenam S, Kosiyatrakul A, Jangsombatsiri W, Pimpabootr N, Vathana T. Midterm outcome of partial radial head replacement with a contoured iliac crest bone graft in complex elbow dislocation. J Orthop Surg (Hong Kong). 2018;2 https://doi.org/10.1177/2309499017754105.
- Helling HJ, Prokop A, Schmidt HU, et al. Biodegradable implants versus standard metal fixation for displaced radial head fractures: a prospective randomized, multicenter study. J Shoulder Elbow Surg 2006; 15:479-85.
- Koslowsky TC, Mader K, Gausepohl T, Pennig D. Reconstruction of Mason type-III and type-IV radial head fractures with a new fixation device: 23 patients followed 1-4 years. Acta Orthop 2007;78:151-6.
- Caputo AE, Burton KJ, Cohen MS, King GJ. Articular cartilage injuries of the capitellum interposed in radial head fractures: a report of ten cases. J Shoulder Elbow Surg 2006;15:716 –720.