Information
Journal Policies
Comparison of Pre-Operative Clinical Condition and Values Ultrasound Findings with Postoperative Outcome of Surgical Treatment of Infants with Congenital Hypertrophic Pilorostenosis (CHP)
Karavdic K1*, Begic-Kapetanovic S1, Izmirlic M2
2.Medical Faculty,University of Sarajevo,Čekaluša 90. 71000 Sarajevo,Bosnia and Herzegovina.
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction : Congenital hypertrophic pyloric stenosis is an gastric outlet obstruction. It occurs in infants, most offten in the period of the 3rd to 6th week of life. Congenital hypertrophic pyloric stenosis occurs at 2 to 3,5 on 1000 live births. It is more common in first-born and male children (male to female ration is 4:1). Etiology of disease is not comletely cleare yet , but according to numerous of studies, both genetics and environmental facors have a contribution. The leading symptom is nonbilious projectile vomiting soon after feeding. There is also opstipation. If vomiting takes a few days, alkalosis, electrolyte disorder, dehydration and malnutrition may be present. The gold standard in diagnosis is ultrasound, which has high sensitivity (97%) and specificity (100%). The final treatment is surgical incision of the pyloric wall to the mucous membrane with leaving pylorus unstretched. The success of the surgical procedure is 100%.
Materials And Methods: The study included 58 infants surgically treated due to congenital hypertrophic pyloric stenosis at the Department of the pediatric surgery of the Clinical center University of Sarajevo in period from 01.01.2007. to 31.12.2017. Data were collected from medical records stored in the Archive of the Clinic for pediatric surgery.
Results: There is no statistically significant correlation of duration of vomiting, acid-base status, hydration status and ultrasonographic findings on admission with postoperative lenght of stay and time of nasogastric tube removal. There is no statistically significant correlation of age and weight on admission with postoperative lenght of stay. There is statistically significant negative correlation of age and weight on admission with time of nasogastric tube removal. There is no statistically significant dependence of duration of vomiting, age on admission, weight on admission, acido-base status on admission, hydration status on admission and ultrasonographic findings on presence of early postoperative complications.
Comparation, Kongenital Hypertrophic Pyloric Stenosis, Preoperative Clinical Condition, Ultrasonographic Finding, Postoperative Outcome,Surgery
1. Introduction
Congenital hypertrophic pilorostenosis is a relatively common illness with an incidence of 2-3.5 on 1000 live-born children [1,2]. Most commonly affects prematuruses, firstborn and male children (male to female ration is 4:1 ) in the period of the 3rd to 6th week of life[3,4]. Etiology is not clear yet, it is assumed to be generated by the interaction of genetic and environmental factors[5,6]. The diagnosis is based on heteroanamnesis, physical finding and ultrasonography. The leading symptom is nonbilious projectile vomiting soon after feeding. There is also opstipation. If vomiting takes a few days, alkalosis, electrolyte disorder, dehydration and malnutrition may be present. The gold standard in diagnosis is ultrasound, which has high sensitivity (97%) and specificity (100%)[7]. In certain unclear cases, the contrasting rtg of gastroduodenum is also applied [8-10]. The final treatment is surgical incision of the pyloric wall to the mucous membrane with leaving pylorus unstretched[11-14]. The success of the surgical procedure is 100%. Prior to surgical treatment, correction of metabolic disbalance is necessary[15].
Early diagnosis and treatment play an important role in preventing complications resulting from electrolyte and acid-base disorders, dehydration and malnutrition[16]. By preventing the occurrence of complications, the time spent in the hospital is reduced. Therefore, it is of great importance to examine possible association, which would allow for more adequate postoperative care and shortening the time of postoperative hospitalization.
Congenital hypertrophic pylorostenosis, although not sufficiently researched today, is a relatively frequent disease. For this reason, it is important to investigate the effect of preoperative clinical condition on postoperative outcome with the aim of providing more adequate and better postoperative patient care.
The aim was to compare preoperative clinical condition and value of ultrasound findings with postoperative outcome.
2. Materials And Methods
The study included 58 breastfeeding patients treated at the Clinic for Pediatric Surgery of the University Clinical Center of Sarajevo in the period from 01.01.2007. until 31.12.2017. year due to clinical and radiologically verified congenital hypertrophic pilorocytosis. The target group was formed based on data from the HIS (hospital information system) and operational protocols of the Clinic for Pediatric Surgery. The criteria for inclusion of the patients in the study were: the infant population aged 0-3 months, clinically and radiologically confirmed diagnosis of congenital hypertrophic pylorostenosis.
The criteria for exclusion of patients from the study were: infants older than 3 months, clinically and / or radiologically unrecognized diagnosis of congenital hypertrophic pylorostenosis and patients with confirmed diagnosis that were not surgically treated.
Parameters are divided into two groups: parameters of preoperative clinical condition and parameters of postoperative outcome. Preoperative clinical condition parameters are (6): duration of symptom duration, age of admission, body weight on admission, acid status at reception, status of hydration at the intake and ultrasound finding (thickness of muscle wall pilorus and pituitary thoracic channel) at reception. Parameters of postoperative outcomes (3): length of postoperative hospitalization, time taken for nasogastric tubee and early postoperative complications.
a. The relationship between duration of symptom duration, age of admission, bodyweight upon admission, acid status in admission, and hydration status at admission of ultrasound on arrival with length of postoperative hospitalization was investigated.
b. The relationship between symptom duration, age of admission, bodyweight on admission, acid-status reception status, receiving hydration status, and ultrasonic finding on nasogastric probe take-up were investigated.
c. Dependence of duration of symptom duration, age of admission, bodyweight on admission, acid status of admission, admission status of hydration and ultrasonography on admission with early postoperative complications were investigated.
3. Results
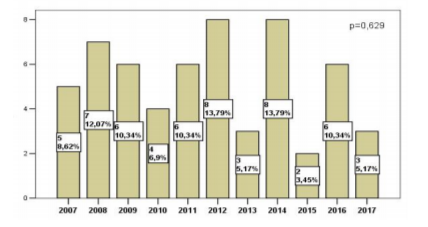
In the 11-year study period from 01.01.2007. until 31.12.1993. 58 patients with clinically and radiologically confirmed diagnosis of congenital hypertrophic pilorocytosis were operated. The largest number of operational interventions were conducted in 2012 and 2014, with 8 (13.79%), while the lowest number was in 2015 and was 2 (3.45%). The observed difference in the frequency of surgical procedures by year was not statistically significant (p = 0.629).
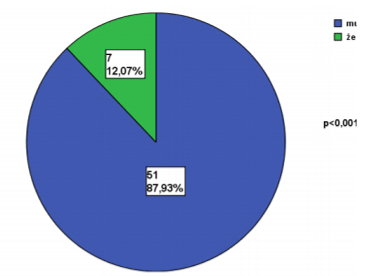
Of the 58 surveyed patients, 51 (87.93%) were male, while the other 7 (12.07%) were female. The established difference in sex distribution was statistically significant (p = < 0.001). (Graph 2)
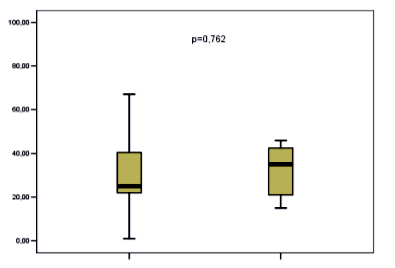
The mean age of the symptoms of all patients involved in the study was 26.0 days (21.75-41.75). The mean age of the symptoms in male patients was 25.0 days (22.0-41.0) and did not statistically differ significantly from the average age at the onset of symptoms in female patients, which was 35.0 days (20 , 0 to 46.0). (p = 0.762) (Graph 3)
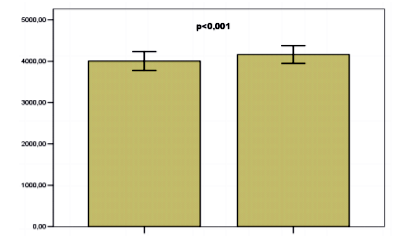
The average body weight at admission was 4004.63 ± 115.48 g and was statistically significantly lower than the average body weight at discharge 4161.53 ± 778.05 g (p < 0.001).
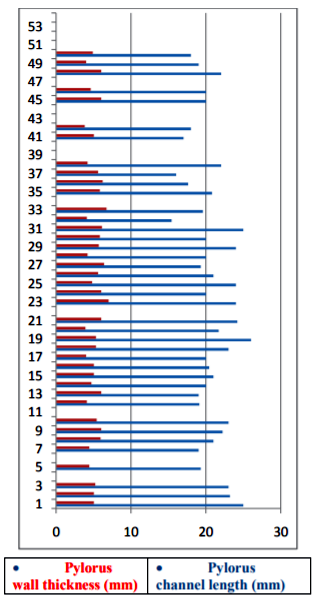
The average length of the pyloric canal in all treated patients was 20.76 ± 0.40. The thickness of the muscle thickness was 5.22 ± 0.13. (Figure 5) The average length of postoperative hospitalization was 7.74 days, and the time of the nasogastric probe was 43.67 h.
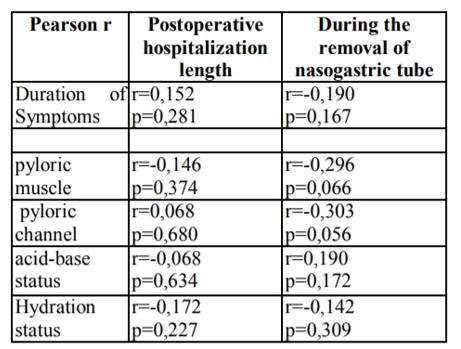
The correlations of parameters of preoperative clinical condition and UZ values with parameters of postoperative outcome were examined. (Table 1) No statistically significant correlation (p> 0.05) was found between the parameters given in the table. (Results not shown!)
No statistically significant correlation was found between the duration of symptoms and length of postoperative hospitalization (p = 0.281), nor between the duration of symptom and time of withdrawal of NG probe (p = 0.167).
Acid-status status at reception does not affect postoperative outcome in these patients (p = 0.634, p = 0.172).
The status of hydration at reception does not affect the postoperative outcome (p = 0.227; p = 0.309)
A statistically significant correlation was not established either between the value of the UZ finding and the length of postoperative hospitalization (mm p = 0.374; pk p = 0.680), nor between the value of the UZ finding and the NG probe timeout (mm p = 0.066, pk p = 0.056).
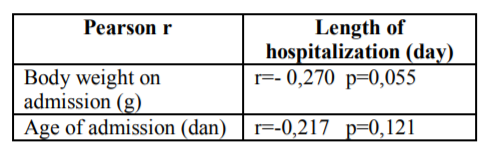
There was no statistically significant correlation between the age and body weight at the time of postoperative hospitalization. (Table 2).
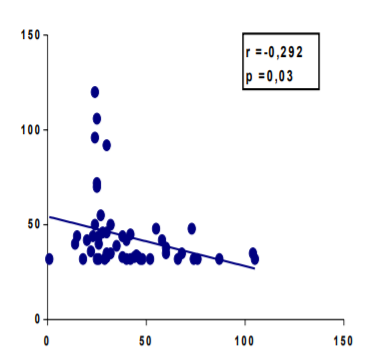
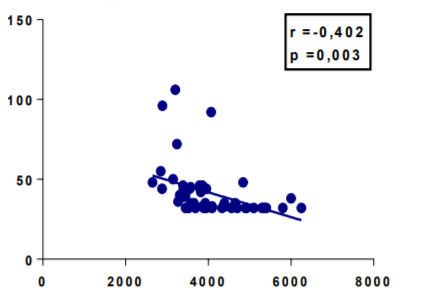
A statistically significant negative correlation between the age of the infant at reception and the time of NG probe was determined. (Figure 6)
A statistically significant negative correlation was found between the body weight of the infant at the intake and the time taken for the NG tube. (Figure 7)
Dependence of duration of symptom duration, age, body weight, acid status, hydration status, and ultrasound findings at the onset of early postoperative complications were investigated. No statistically significant correlation was found between these parameters (p> 0.05). (Results not shown!).
4. Discussion
The aim of this study was to examine the correlation between preoperative clinical condition and UZ findings with the postoperative outcome of breast cancer treatment with congenital hypertrophic pilorostenosis. The results show which parameters extend the postoperative hospitalization itself, and which is a possible way to shorten the length of postoperative hospitalization of these patients. Shortening the length of postoperative hospitalization of this group of patients leads to the following: it reduces the exposure of operated patients to hospital infections, reduces parent anxiety, allows for faster recovery of infants and gains weight, reduces the cost of staying at a hospital facility and reduces the occupancy of beds in children's hospice departments.
The average length of postoperative hospitalization in our study was 7.74 ± 0.75 days. Ayman et al. indicate the average duration of hospitalization after surgery for 5.1 ± 2.2 days. Only 1 (2.1%) patient of a total 47 patients developed early postoperative complications, and none required reoperation[17]. The results of our study show that 9 (16.07%) of patients had one of the early postoperative complications and 1 (1.72%) required reoperation. This is probably the reason for the higher average length of postoperative hospitalization in our study. Davoud et al. reported an average postoperative hospitalization of 55.22 ± 0.08 h [19], which is a shorter shorter hospital stay after surgery compared to our study and study conducted by Ayman et al. The average time of removal of the NG tube in the study conducted by Ayman et al. amounted to 31.0 h [17], while the mean time of withdrawal of the NG tube 43.67h showed our study. Garza et al. in their study,found that the average duration of hospitalization was 33.6 hours, while the mean time of withdrawal of NG tube was 18.5 h[20]. It is undoubtedly from the above data that the time of removeing the nasogastric tube directly affects the length of postoperative hospitalization. Possible explanation of the difference in the time taken to extract the nasogastric tube between Davoud and aut., our studies and studies on Ayman et al. is in carrying out dietary regimens to complete enteral entry. In patients in our study, the oral intake through the nasogastric tube starts 8 h after the operation. However, there are regimens that start earlier and last shorter, resulting in shorter time for NG tubes[21]. However, premature introduction of enteral intake, as per Van der Bilt and al. refers to the beginning of the first 4h post-operative feeding [22], leading to more frequent postoperative vomiting, which is a limiting factor in establishing full enteral intake and NG tubee retrieval. Scharli and al. suggest that 4-6h after the pyloromyotomy stomach peristalsis absent, and in the next 16-24h it remains slowed down. Therefore, entering liquid into the digestive tract during this period can lead to hyperperistals and vomiting [23]. In Davoud et al. 90 (72%) of a 120 patients, had at least one episodic episode of episodes after pyloromyotomy [19], while in our study a percentage of at least one episode of 47.27% was recorded. It is expected that longer duration of vomiting will require longer recovery time, hence longer postoperative hospitalization, but data does not show this[17]. Our study found that there was no statistically significant correlation between the duration of symptoms and the length of postoperative hospitalization. Ayman et al., In their study, also found that there was no statistically significant correlation between the duration of symptoms and the length of postoperative hospitalization[17]. However, our study shows that there is no statistically significant correlation between the duration of the symptoms and the time taken to remove the NG tube. Ayman et al. their study also found that there was no statistically significant correlation between the above parameters[17]. Garza et al. indicates that NG tube withdrawal time is shorter for 10 h in patients treated with laparoscopic technique [20]. All of our patients were treated with open laparotomy. However, Shawn et al. suggest that there is no difference in the time taken to extract the NG tube in patients operated laparoscopically than those treated with laparotomy[24].
The parameters that were monitored for the ultrasound findings were: length of the pyloric channel and thickness of the pyloric wall. The largest length of pyloric channels was 26 mm and the smallest 15.4 mm. The largest pylorus wall thickness in the subjects was 7 mm and the lowest 3.8 mm. The average pylorus channel length of our patients was 20.76 ± 0.40. The average pylorus wall thickness was 5.22 ± 0.13. The ultrasonic finding criteria for the diagnosis of pyloric stenosis are length of pyloric channels> 16 mm and pylorus wall thickness> 4 mm. Davoud et al. following values were quoted: the length of the pyloric channels of all patients ranged from 7.60 mm to 29.00 mm, an average value of 19.54 ± 0.324 mm, while the thickness of the pyloric wall from all patients ranged from 2.70 mm up to 9.00 mm, average values 4.86 ± 0.108 mm. [19] Hamdi Hameed et al.noted the average length of the pyloric channel 19.5 ± 3.2 mm and the average thickness of the pyloric wall 5.3 ± 1.1 mm[25].
No statistically significant correlation was found between the value of ultrasound finding and length of hospitalization, as well as between the value of the ultrasonic finding and the NG tube removal time. Davoud et al. in their study also state that there is no statistically significant correlation between these parameters[19].
The results of our study show that there is a statistically significant negative correlation between body weight on admission and NG tube withdrawal time, but not between body weight on admission and length of postoperative hospitalization. The reason is the same reason for the disaggregation of the age of the patient on the hospitalization and length of hospitalization. Iqbal et al. published that there is a statistically significant positive correlation between the body weight on the admission and the value of ultrasound findings. Patients with higher body weight at admission have higher values of observed parameters measured by ultrasound. Said et al. published that the ultrasound findings are correlated with age and body weight on admission, and that physicians should note that younger infants with clinical diagnosis of pyloric stenosis may indeed suffer from congenital hypertrophic pyloric stenosis, although the diagnostic criteria for ultrasound findings are not present[25-27]. Our study showed that 26 (49.06%) patients had alkalosis on admission, while 27 (50.94%) had acid status at the reference limits. The study shows that there is no statistically significant correlation between acid status at admission and length of postoperative hospitalization as well as between acid status at admission and time of NG tube retrieval. Kuo-Shu Tang et al. also show that the alkalosis at admission has no statistically significant correlation with the length of postoperative hospitalization[28].
The study showed that the status of hydration at admission did not have a statistically significant correlation with the length of postoperative hospitalization nor the time of NG tube retrieval. All patients were laid off after postoperative hospitalization in a good general condition. No mortality cases have been reported. Phillipo et al. reported 5 (4.9%) mortality cases and reported that the most common complication was an infection of the wound with a percentage of 27.3%[29]. Our study also shows that this is the most common complication, with a percentage of 7.14%. Of the preoperative parameters examined, only the body weight on admission and the age of admission affect the postoperative outcome. According to this, older infants with higher body weight at admission have the highest chance of staying in the hospital shortly after surgery. Of course, there are always exceptions. In practice, a major role in improving the treatment of these patients has early recognition and treatment. The reason is that early recognition shortens the duration of symptoms, and shorter duration of vomiting and constipation leads to a lower loss on the body weight of these patients. It has already been stated that the body weight is negatively correlated with the time taken to extract the NG tube.
The length of postoperative hospitalization of these patients is now being documented and there are many studies that point out the effect of the time out of removing out the NG tube. For this purpose, new diet schemes have been introduced after pyloromyotomy and attempt to shorten the start time of eneteral intake after pyloromiotomy[30]. In addition, some studies indicate that hospitalization is affected by surgical technique, so shorter recovery after laparoscopy compared to laparotomy[20,31]. Nigel et al. suggest a significantly higher incidence of operative and postoperative complications and lower efficacy in laparoscopic than open pyloriotomy[31]. This research investigated the correlation between preoperative clinical image and ultrasound findings with postoperative outcome and it was found that neither the preoperative clinical image nor the ultrasound finding score significantly influenced the postoperative outcome of the infant's treatment with congenital hypertrophic piloroscoposis and statistically significant effect on the postoperative outcome had only age and body weight at reception.
5. Conclusion
Preoperative clinical and ultrasound finding score significantly not influenced at the postoperative outcome of the infant's treatment with congenital hypertrophic pylorostenosis and statistically significant effect on the postoperative outcome had only patient's age and body weight at admission.
References
- Baskovic M, Zupancic B, Lesjak N, Vukasovic I. Acta Med Croatica, 70 (2016) 103-106.
- Sosa T, Sutlic Z, Stanec Z, Tonkovic I, i sur, Kirurgija. Zagreb: Naklada ljevak; 2007
- S Irish M, J´and Lucille R, M Bovet P, L Windle M, E Besner G, Clatworthy H W, et al. Pediatric hypertrophic pyloric stenosis surgery. Mart 25 (2016). Dostupno na: https://emedici ne.medscape.com/article/937263-overview
- Nazer H, Nazer D, Windle M L, Cuffari C, Du Bois J J, Beals D A, et al. Pediatric hipertrophic pyloric stenosis. Jul 26 (2017). Dostupno na: https://emedicine.medscape.com/article/929829 -overview
- Godbole P, Sprigg A, Dickson J A, Lin P C. Ultrasound comapred with clinical examination in infantile hypertrophic pyloric stenosis. Arch Dis Child. Oct (1996); 75(4): 335-337. Dost upno na: https://www.ncbi.nlm.nih.gov/pm c/ articles/PMC1511760/
- Jalsovec D. Sustavna i topografska anatomija covjeka, Zagreb:školska knjiga,str. 497-523.
- Junqueira L C, Carneiro J. Osnovi histologije. Jedanaesto izdanje. Ur. Lackovic V, Todorovic V. Beograd:data status.
- Sadler T. W. Langmanova medicinska embriologija. Zagreb: medicinska naklada.
- Olivé A P, Endom E E. Infantile hypertrophic pyloric stenosis. Updated: Sept 29 (2017). Dostupno na: https://www.uptodate.com/con tents/infantile-hypertrophic-pyloric-stenosis
- Vanderwinden J M, Vanderhaeghen J J, De Laet M H. Nitric oxide synthesis in infantile hypertrophic pyloric stenosis. N Engl J Med 1992; 327: 1690-1691. Dostupno na:https:// www.nejm.org/doi/full/10.1056/NEJM1992120 33272316
- Rogers I M, New insights on the pathogenesis of pyloric stenosis of infancy. A review with emphasis on the hyperacidity theory. Open Journal of Pediatrics. 2012, 2, 97-105.
- Ohshiro K, Puri P. Pathogenesis of infantile hypertrophic pyloric stenosis: recent progress . Pediatr Surg Int., 1998 April;13(4):243-52. Dotupno na: https://www.ncbi.nlm.nih.gov/ pubmed/9553181
- Dukic A, Durdevic P, Zivancevic-Simonovic S, Jurisic V, Mijatovic Lj. Opsta patoloska fiziologija. Drugo izdanje. Kragujevac: naša knjiga; 2006.
- Prpic I i sur. Kirugija za medicinare. Treće, nepromijenjeno izdanje. Zagreb: školska knjiga;2005.
- Subramaniam S. Pediatric pyloric stenosis clinical presentation. Updated: Oct 24 2017. Dostupno na: https://emedicine.medscape.com /article/803489-clinical
- Sharma R, Amini B, et al. Dostupno na: https://radiopaedia.org/articles/pyloric-stenosis
- Al-Jazaeri A, Al-Shehri A, Zamakhshary M, Al-Zahem A. Ann. Can the duration of vomiting predict postoperative outcomes in hypertrophic pyloric stenosis? Saudi Med. 2011 Nov-Dec; 31(6): 609-612. Dostupno na: https:// www.ncbi.nlm.nih.gov/pmc/articles/PMC3221 133/#ref2
- White J. S, Clements W. D. B, Heggarty P, Sindhu S, Mackle E, Stirling I. Treatment of infantile hypertrophic pyloric stenosis in a district general hospital: a review of 160 cases. Journal of pediatric medicine, pages 1333-1336. Dostupno na:https://www.jpedsurg.org/ article/S0022-3468(03)00391-9/fulltext
- Badebarin D, Aslanabadi S, Yazdanpanah , Zarrintan S. Afr J Pediatr Surg. 2016 Apr-Jun; 13(2): 73-75. Dostupno na: https://www.ncbi. nlm.nih.gov/pmc/articles/PMC4955443/#ref21
- Garza J. J, Morash D, Dzakovic A, Mondschein K. J, Jaksic T. Journal of Pediatric Surgery. Ad libitum feeding decreases hospital stay for neonates after pyloromyotomy. March (2002). Pages 493-495. Dostupno na: https://wwwjped surg.org/article/S0022-3468 (02) 92338-9/pdf
- van der Bilt J D, Kramer W L, van der Zee DC, Bax NM. Early feeding after laparoscopic pyloromyotomy: the pros. and cons. Surg Endosc. 2004 May; 18(5):746-8. Dostupbo na: https://www.ncbi.nlm.nih.gov/pubmed/150269 00
- Scharli A F, Leditschke J F. Gastric motility after pyloromyotomy in infants: A reappraisal of postoperative feeding. Surgery 64:1133-1137 (December) 1968. Dostupno na: https://www. jpedsurg.org/ article/ 0022-3468 (69)90418-7/abstract
- D. St. Peter S, W. Holcomb G, M. Calkins C, Murphy J Patrick, S. Andrews W, J. Sharp R, et al. Open versus laparoscopic pyloromyotomy for pyloric stenosis: A prospective, randomized trial. Annals of Surgery 2006; 244(3):363-370. Dostupno na: https://insights.ovid.com/ crossref ?an=00153307-200601240-00004
- D. Safford S, Pietrobon R, M. Safford K, Martins H, A. Skinner M, E. Rice H. A study of 11,003 patients with hypertrophic pyloric stenosis and the association between surgeon and hospital volume and outcomes. Journal of pediatric surgery, 2005. Dostupno na: https://www.jpedsurg.org/article/S0022-3468 (05)00205-8/abstract
- AlMaramhy H H. Is there a relation between pyloric muscle thickness and clinical and laboratory data in infants with hypertrophic pyloric stenosis. Indian J Surg. 2015 Dec; 77(Suppl 3): 827-830. Dostupno na: https://www.ncbi.nlm.nih.gov/pmc/articles/PM C4775562/
- Said M, Shaul D B, Fujimoto M, Radner G, Sydorak D M, Applebaum H. Ultrasound measurements in hypertrophic pyloric stenosis: Don´t let the numbers fool you. Perm J. 2012 Summer; 16(3): 25-27. Dostupno na: https://www.ncbi.nlm.nih.gov/pmc/articles/PM C3442757/
- Nasr A, H. Ein S, postoperative pyloric stenosis in the newborn: a forgotten problem. Journal of pediatric surgery, 2007. Dostupno na: https://www.jpedsurg.org/article/S0022-3468 (07)00184-4/abstract
- Tang KS, Huang IF, Shih HH, Huang YH, Wu CH, Lu CC et al. Factors contributing to prolonged hospitalization of patients with infantile hypertrophic pyloric stenosis. Pediatrics and neonatology, August 2011. Dostupno na: https://www.sciencedirect.com/ science/article/pii/S1875957211000659#tbl2
- L. Chalya P, Manyama M, M. Kayange N, B. Mabula J, Massenga A. Infantile hypertrophic pyloric stenosis at a tertiary care hospital in Tanzania: a surgical experience with 102 patients over a 5-year period. BMC Res Notes. 2015; 8:690 https://www.ncbi.nlm.nih.gov/ pmc/articles/PMC4652415/
- Sullivan KJ, Chan E, Vincent J, Iqbal M, Wayne C, Nasr A, et al. Feeding post-pyloromyotomy:A meta-analisis. Pediatrics 2016 Jan;137(1). Dostupno na: https://m.eur ekamag.com/research/057/871/05787 1504.php
- J. Hall N, Van Der Zee Y, L. Tan H, Pierro A. Meta-analysis of laparoscopis versus open pyloromyotomy. Ann Surg. 2004 Nov;240 (5):774-778. Dostupno na: https://www.ncbi. nlm.nih.gov/pmc/articles/PMC13 56481/