Information
Journal Policies
Biliary Pancreatitis: Current Practices and Guidelines
Ankush Sarwal MS,FNB,FIAGES1*, Pulkit Maru M.D2, Anant Pore DNB1, Piyush Shankar Tripathi DNB1, Amardeep kumar M.S3
2.Department of Radiodiagnosis.Tata Medical Centre, Kolkata, India.
3.Departmnet of Mininal Access, Max Healthcare Institute Ltd. Saket, New Delhi, India.
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Acute pancreatitis is a life threatening disease and is a common gastrointestinal emergency. Abdominal pain is its predominant presenting symptom. Gall stone are the commonest cause of acute pancreatitis. Severe biliary pancreatitis is associated with a significant morbidity and mortality. Pathophysiology of biliary pancreatitis is still not fully understood. Various recommendations are there in literature for managing a patient of biliary pancreatitis. In this article we review the possible mechanism and current recommendations in acute biliary pancreatitis and its management.
Biliary Pancreatitis, Acute Pancreatitis, Laparoscopic Cholecystectomy,Surgery
1. Introduction
Acute pancreatitis (AP) is a severe disease associated with significant morbidity and mortality. There is no specific treatment for AP other than supportive care. The most common etiology of acute pancreatitis is gallstones and alcohol consumption [1]. Gallstone disease is one of the major causes of abdominal morbidity and mortality throughout the world. Ranging from asymptomatic cholelithiasis to potentially lethal pancreatitis, biliary disorders are notorious for causing several abdominal diseases. Especially small gall bladder calculi and sludge can migrate from the gallbladder into the duodenum [2]. The mechanism of gall stone induced acute pancreatitis is still not fully understood. Long-term management of cholelithiasis aims at minimizing the risk of new biliary events. Recurrence rates of biliary pancreatitis up to 61% have been described when no definitive treatment was provided. Failure to provide definitive treatment exposes the patient to potentially fatal risks of biliary diseases [3]. This paper reviews the current literature and evidence on gall stone induce pancreatitis.
In 1901 Eugene Opie gave the common channel hypothesis which proposed that a gallstone transiently lodged in the distal common channel of the ampulla of Vater allowed bile to reflux into the pancreatic duct [4]. Another proposal suggested that passage of a stone through the sphincter causes transient incompetence of sphincter allowing duodenal fluid and bile reflux into the pancreatic duct. A third possibility is obstruction of the pancreatic duct due to gall stones, leading to ductal hypertension. This causes minor ductal disruption, extravasation of pancreatic juice into the less alkaline interstitium of the pancreas, and promotion of enzyme activation [5]. In cases where other etiological factors are not evident, there is still the possibility of finding microlithiasis, seen as birefringent crystals, on microscopy visualisation of bile[6]. This occult microlithiasis is probably responsible for up to half of those with idiopathic acute pancreatitis.
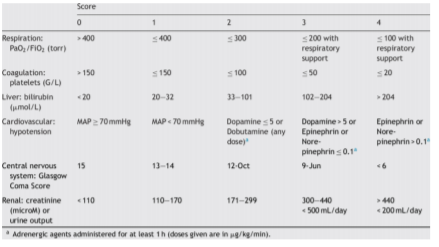
Patient having acute pancreatitis usually presents with sudden onset of a severe constant epigastric pain radiating to mid back, additionally can be associated with nausea and vomiting. Patient has tachycardia and can develop fever. Till date, none of the available tests can be used as the gold standard for the assessment of the severity of AP. Patient suffering from gallstone-induced AP will have blood ALT levels over 150 IU/L with a 48–93% sensitivity and 34–96% specificity. Serum amylase not specific for AP but a normal amylase level rules out an event of pancreatitis [7]. A serum lipase test should be performed in all patients with a suspected diagnosis. A 3-fold elevation of serum lipase from the upper limit of normal is required to make the diagnosis of AP [8]. Study done by Anderson et al showed blood trypsin-2-α1 antitrypsin complex/ trypsinogen-1 ratio as a useful marker for diagnosis of gallstone-induced AP[9].Some role of measuring nesfatin-1 and leptin levels at admission has been reported in literature but it is not part of current guidelines to follow[10]. To assess the severity of AP and systemic response, there are various scoring system like Ranson`s score and Sequential organ failure assessment (SOFA) score. [Figure 1]
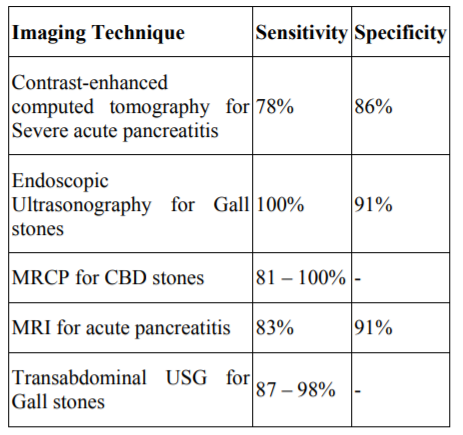
A combination of findings of gall bladder stone, dilated biliary tree and changes of pancreatitis on cross-sectional imaging is highly supportive in diagnosis of gall stone pancreatitis. A further finding of a gall stone in distal biliary duct is diagnostic in a patient of acute onset pain [11,12].
CECT with oral and intravenous contrast is the preferred modality for initial evaluation and follow up of pancreatitis with moderate sensitivity and excellent specificity for changes of pancreatitis and its complications. In acute pancreatitis, CECT is usually acquired in the pancreatic phase of CECT, the affected pancreas appears enlarged and heterogeneous or hypo attenuating with irregular margins, peripancreatic fat stranding, thickening of fascia, intraperitoneal or retroperitoneal fluid collections [12,13]. Fluid collections are initially seen at peripancreatic and anterior pararenal spaces and may extend from the mediastinum to pelvis. Sections of thorax can show pleural effusion which is often left sided. Complications such as pseudocyst, pancreatic abscess and haemorrhage, necrosis, venous thrombosis and pseudoaneurysms, can all be recognized with CECT [13].
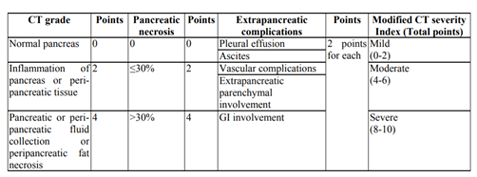
Revised Atlanta classification provides a CT severity index and grades acute pancreatitis into mild, moderate and severe [14]. Major drawback of CECT is that it is poorly sensitive in identifying the radiolucent gall stones.
MR imaging can reliably depict features of pancreatitis equally sensitive to CT. Moreover, MRCP can image the biliary tree and pancreatic ductal system non-invasively and detect calculi in gall bladder as well as bile duct [11,13]. Unlike ERCP, it can be used to image proximal to the site of obstruction, depict any anatomical variations, congenital disorders or more commonly depict obstructive dilatation of biliary and pancreatic ducts in case of calculus at ampulla. Being non-invasive modality, it carries none of the risks associated with ERCP.
Transabdominal USG is an excellent imaging modality for detection of gall bladder calculi and biliary duct dilatation and in the hands of well experienced sonologists, these findings are almost never missed. A calculus is seen as echogenic reflection with posterior acoustic shadow. Additionally, acute cholecystitis can be diagnosed by observing the GB wall and pericholecysticfluid [11,15]. Distal CBD can sometimes be difficult to image transabdominally due to bowel gas but endoscopic ultrasound can overcome this problem and show the cause of proximal dilatation of bile duct such as a distal calculus [16]. Endoscopic ultrasound (EUS) can be immediately followed up with ERCP for stone retrieval.
Transabdominal USG can also detect, though with decreased sensitivity as compared with CECT, changes of acute pancreatitis such as enlargement of pancreatic gland and fluid in peripancreatic, anterior pararenal and peritoneal spaces. The problem lies with the sentinel loop of transverse colon, which in cases of acute pancreatitis is a peristaltic and filled with gas and thus hiding the pancreas from view on a transabdominal USG. EUS can circumvent this and additionally image the pancreas directly from wall of stomach and duodenum and look for changes of pancreatitis. EUS is superior to ultrasonography in terms of ability to visualize common bile duct stones [16].
There has been an ongoing debate for years on role of ERCP with sphincterotomy as early intervention in patients having biliary pancreatitis. However, pancreaticography should be avoided as when ERCP is performed for gallstone-induced pancreatitis [17].
Supportive care, including resuscitation with isotonic intravenous fluids (e.g., Ringer’s Lactate solution), pain control and mobilization should be the mainstay of treatment of patients with biliary pancreatitis. Prophylactic antibiotics are not recommended in patients with mild or severe acute pancreatitis. Antibiotics should be prescribed only in patients with infected necrosis confirmed by FNAC or if there is gas within a collection visualized on CT scan. Repeat CECT can be performed in case infection is suspected. Enteral nutrition should be started as soon as possible following admission preferably within 48 hrs of admission. A nasojejunal tube is not superior to a nasogastric feeding tube; thus commencement of feeds should not be delayed for the purpose of placing a nasojejunal feeding tube. Enteral feeding is recommended over parentralnutrition [18].
2. Treatment Of Biliary Stones In Gallstone-Induced Pancreatitis
International Association of Pancreatology (IAP) Guidelines suggest that early ERCP is beneficial in patients with on-going cholestasis due to biliary obstruction. Early ERCP should be performed in gallstone induced acute pancreatitis when complications of cholangitisor prolonged passage disorder of the biliary tract is suspected [19]. Similarly various RCTs conducted by Zhou et al and Orisa et al have shown usefulness of ERCP in cases with severe gallstone-induced acute pancreatitis accompanied by a prolonged passage disorder of the bile duct[20,21].
After an episode of biliary pancreatitis, patients may have a recurrent episode of gall stone induced pancreatitis predicted to be as high as 32–31% or other biliary events, such as or biliary colics, acutecholecystitis, Obstructive jaundice due to CBD stones or cholangitis. In order to prevent these recurrentbiliary events, IAP guidelines advise performing cholecystectomy after biliary pancreatitis [22]. In case definitive treatment is not provided to the patient, there is a high possibility of fatal risks of recurrent biliary diseases. The timing of cholecystectomy in patients with clinically severe pancreatitis, with local complications such aspancreatic necrosis and organ failure, is deliberately delayed until local complications have resolved, typically after some 6 weeks. In patients with mild pancreatitis, International guidelines advise cholecystectomy directly after recovery or in the first 2 to 4 weeks after discharge for mild biliary pancreatitis [22,23].
Laparoscopic cholecystectomy (LC) has been introduced actively ingallstone-induced acute pancreatitis. Analysing the data of various retrospective studies, it was found that LC had a success rate of 94.5%, with the incidence of complications was 5.5% and the mortality rate was low of around 0.4% (0–2.5%), suggesting that LC is as successful as open surgery [24,25]. Most of the times while operating a patient with history of biliary pancreatitis the laparoscopic cholecystectomy is not as difficult as predicted by the surgeons. At present, the type of adequateprocedures is decided as per the skills of the operating surgeon. Instead of ERCP, LC can be performed along with Intra Operative Cholangiography and in case the operating surgeon does not have the expertise of Laparoscopic CBD exploration then the procedure could be converted to open cholecystectomy otherwise laparoscopic CBD exploration is an equally efficient procedure [26]. There is a high possibility that LC will make remarkable progress and become a standardized procedure for managing gall stones in patients of biliary pancreatitis. Still, more studies and data isrequired concerning the safety, invasiveness, rate of successfulexecution and adequate selection of cases involved.
3. Conclusion
Gall stone induced pancreatitis is associated with significant morbidity and mortality. Supportive care is the initial mainstay in managing a patient with biliary pancreatitis. Several haematological, biochemical and radiological investigations are helpful in assessing the severity of pancreatitis and response to the treatment given to the patient. There is high possibility of recurrent episode of gall stone induced pancreatitis or other biliary problems which can be fatal at times. To avoid these complications, definitive treatment in form of cholecystectomy should be done in every patient. Timing of cholecystectomy depends on the severity of pancreatitis. With the advances in medicine laparoscopic cholecystectomy is to become the procedure of choice for biliary pancreatitis.
References
- Banks PA. Epidemiology, natural history, and predictors of disease outcome in acute and chronic pancreatitis. GastrointestEndosc2002; 56(Suppl):S226-30.
- Peery AF, Dellon ES, Lund J, Crockett SD, McGowan CE, Bulsiewicz WJ, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 2012;143. 1179-87 e1e3.
- Alimoglu O, Ozkan OV, Sahin M, Akcakaya A, Eryilmaz R, Bas G. Timing of cholecystectomy for acute biliary pancreatitis: outcomes of cholecystectomy on first admission and after recurrent biliary pancreatitis. World J Surg 2003;27:256e9.
- Opie E. The etiology of acute hemorrhagic pancreatitis. John Hopkins Hosp Bull 12: 182-188,1901.
- Acosta JM, Ledesma CL. Gallstone migration as a cause of acute pancreatitis. N. Engl J Med 1974;290:484e7.
- Lee SP, Nicholls JF, Park HZ. Biliary sludge as a cause ofacute pancreatitis. N Engl J Med. 1992; 326(9): 589-593.
- Liu CL, Fan ST, Lo CM, et al. Clinico-biochemical prediction ofbiliary cause of acute pancreatitis in the era of endoscopic ultrasonography. Aliment PharmacolTher. 2005;22:423–31.
- Greenberg JA, Hsu J, Bawazeer M, Marshall J, Friedrich JO, Nathens A, Coburn N, May GR, Pearsall E, McLeod RS. Clinical practice guideline: management of acute pancreatitis. Can J Surg. 2016 Apr;59(2):128-40.
- Andersen JM, Hedstrom J, Kemppainen E, et al. The ratio of trypsin-2- a 1-antitrypsin to trypsinogen-1 discriminates biliary and alcohol-induced acute pancreatitis. Clin Chem. 2001;47:231– 6.
- Ülger BV, Gül M, Uslukaya Ö, Oğuz A, Bozdağ Z, Yüksel H, Böyük A. New hormones to predict the severity of gallstone-induced acute pancreatitis. Turk J Gastroenterol. 2014 Dec;25(6):714-7. doi: 10.5152/tjg.2014.6201.
- Hazem ZM. Acute biliary pancreatitis: diagnosis and treatment. Saudi J Gastroenterol 2009;15:147–55.doi:10.4103/1319-3767.54740.
- Carroll JK, Herrick B, Gipson T, Lee SP. Acute pancreatitis: diagnosis, prognosis, and treatment. Am Fam Physician 2007;75:1513– 20.
- Arvanitakis M, Delhaye M, Maertelaere VDE, Bali M, Winant C, Coppens E, et al. Computed Tomography and Magnetic Resonance Imaging in 2004:715–23.doi:10.1053/ j.gastro. 2003.12. 006.
- Foster BR, Jensen KK, Bakis G, Shaaban AM, Coakley F V. Revised Atlanta Classification for Acute Pancreatitis: A Pictorial Essay. RadioGraphics 2016;36:675–87.doi:10.1148/ rg. 2016150097.
- Bortoff GA, Chen MYM, Ott DJ, Wolfman NT, Routh WD. Gallbladder Stones:Imaging and Intervention.RadioGraphics 2000;20:751–66 .
- Stabuc B, Drobne D, Ferkolj I, Gruden A, Jereb J, Kolar G, et al. Acute biliary pancreatitis: detection of common bile duct stones with endoscopic ultrasound. Eur J Gastroenterol Hepatol 2008;20:1171–5. doi:10.1097/MEG.0b013e32830a9a31.
- Moon JH, Cho YD, Cha SW, et al. The detection of bile duct stones in suspected biliary pancreatitis: comparison of MRCP, ERCP, and intraductal US. Am J Gastroenterol. 2005;100: 1051– 7.
- Lankisch PG, Weber-Dany B, Lerch MM. Clinical perspectives in pancreatology: compliance with acute pancreatitis guidelines in Germany. Pancreatology 2005;5:591-3.
- Working Group IAPAPAAPG. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology Off J Int Assoc Pancreatol 2013;13:e1e15.
- Zhou MQ, Li NP, Lu RD. Duodenoscopy in treatment of acute gallstone pancreatitis. Hepatobiliary Pancreat Dis Int. 2002;1: 608–10.
- Orıa A, Cimmino D, Ocampo C, et al. Early endoscopicinterventionversusearly conservative management in patients with acute gallstone pancreatitis and biliopancreatic obstruction: a randomized clinical trial. Ann Surg. 2007;245:10–7.
- Uhl W, Warshaw A, Imrie C, Bassi C, McKay CJ, Lankisch PG, Carter R, Di Magno E, Banks PA, Whitcomb DC, Dervenis C, Ulrich CD, Satake K, Ghaneh P, Hartwig W, Werner J, McEntee G, Neoptolemos JP, Büchler MW, International Association of Pancreatology: IAP Guidelines for the Surgical Management of Acute Pancreatitis. Pancreatology 2002, 2:565– 573.
- Toouli J, Brooke-Smith M, Bassi C, Carr-Locke D, Telford J, Freeny P, Imrie C, Tandon R: Guidelines for the management of acute pancreatitis. J GastroenterolHepatol 2002, 17(Suppl 1):15–39.
- Chang L, Lo S, Stabile BE, et al. Preoperative versus postoperative endoscopic retrograde cholangiopancreatography in mild to moderate gallstone pancreatitis: a prospective randomized trial. Ann Surg. 2000;231:82–7.
- Ballestra-Lopez C, Bastida-Vila X, Bettonica-Larranaga C, et al. Laparoscopic management of acute biliary pancreatitis. Surg Endosc. 1997;11:718–21.
- Campbell-Lloyd AJ, Martin DJ, Martin IJ. Long-term outcomes after laparoscopic bile duct exploration: a 5-year follows up of 150 consecutive patients. ANZ J Surg. 2008; 78:492-4.