Information
Journal Policies
The Influence of Instrument Length Calibration on Laparoscopic Depth Perception: A Randomised Controlled Trial
Mohammad K Riaz1*, Manhon Tang1, Benjie Tang1, Afshin Alijani1
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Aim: Laparoscopic task performance relies on the interpretation of 2-D visual image with deteriorating depth perception. This study aims to investigate the impact of laparoscopic instrument length calibration on the depth perception through a randomised controlled trial.
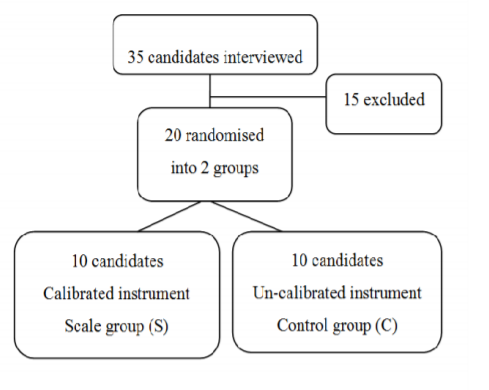
Methods: Twenty medical students were randomised into two groups (scale and control). Studied instrument was calibrated with scale markings, 10 mm apart from instrument tip. Predesigned sheet (10 cm diameter) inside an endotrainer box was marked at 8 peripheral clockwise points. Total distance from the centre of sheet to any of these clockwise points was 10 cm. This distance was concealed from candidates. Instructions were provided to mark the sheet eight times at target distance (TD) from the centre of the sheet at 8 different clockwise directions. Instructions for TD and directions were randomised. There are four potentially optical-axis to view angles (OATV) with a laparoscope and were set at standard for this trial. The task was repeated four times in 150, 450, 600, 900 OATV angles. Difference from TD to marked area was studied and recorded as + (mm) if mark overran and – (mm) if short of target. Data was analysed and statistical differences between both groups was calculated.
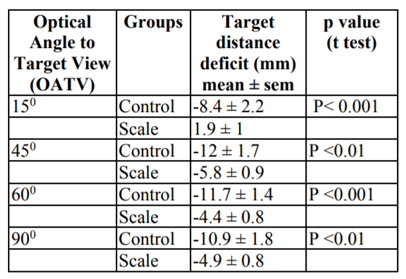
Results: Scale group was nearest to the target in all directions and OATV angles. At 150 OATV angle mean target distance was -8.4 ± 2.2 vs 1.9 ± 1 (mm ± sem) for control and scale group respectively (p < 0.001). Similar variation was noted at 450: -12 ± 1.7 vs -5.8 ± 0.9 (p< 0.01), 600: -11.7 ± 1.4 vs -4.4 ± 0.8 (p< 0.001) and 900: 10.9 ± 1.8 vs -4.9 ± 0.8 (p< 0.01).
Conclusion: Instrument calibration significantly improves laparoscopic task performance by enhancing depth perception in vitro settings.
Depth perception, Instrument calibration, optical-axis-to-view angle,Surgery
1. Introduction
Acquiring motor skills to enhance laparoscopic task performance is fundamental to current surgical training environment. Cognitive ability to master these skills can potentially get compromised due to shortened training period and rapid modernisation of laparoscopic instruments. Bimanual dexterity, depth perception, efficiency and tissue handling are the common impediment for a laparoscopic trainee.
Human brain is accustomed to interpreting objects in three-dimensional settings; however, a laparoscopic camera produces two-dimensional views creating this dilemma of depth perception while working with a laparoscopic instrument. Although majority of trainees overcome this problem with experience; nevertheless, it compromises a valuable time of training, which could be utilised, for excelling surgical skills.
This randomised controlled study aims to investigate a new method of reducing issue of depth perception. We introduced a novice technique of calibrating laparoscopic instruments to create a comparison tool for vision to appreciate the distance in two-dimensional views.
2. Methods
Influence of instrument calibration on depth perception was tested using a mixed-method design. Comparison was made between subjects who used calibrated laparoscopic instrument and those who used normal laparoscopic instrument. Impact of optical-axis-to-view angles on the experiment was also studied.
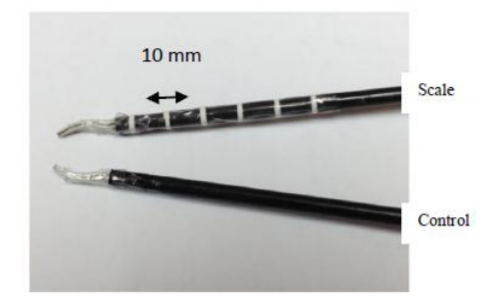
Twenty medical students with no prior laparoscopic experience were invited to participate in this study. All candidates were right-handed and were corrected for eyesight (only right hand working port was utilised). Each received a standard thirty-minute introduction to laparoscopic instrument handling and the set up before experiment. Participants were randomised into two groups; scale and control. Control group used non- calibrated (normal) instrument and scale group used calibrated laparoscopic instrument [Figure 1].
A home-made box was used for this experiment with dimensions of 20 X 30 X 40 cm. Two 5mm ports (Endopath Excel ®, Ethicon Endosurgery, New Jersey, USA) were inserted as working ports from the top with a manipulation angle of 60° with the laparoscope [Figure 2].
Two laparoscopic scissors were used (Endopath Excel ®, Ethicon Endosurgery, New Jersey, USA) for the purpose of making holes as markers on a predesigned sheet of paper as a working area (Figure. 3). Plane scissors were used for the control group. For the study group, scissors were calibrated with six thin white strip, taped 10mm apart [Figure 3].
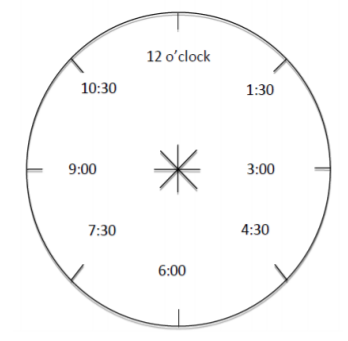
Task was to mark at 8 different o’clock positions by guessing distance from the centre (Target distance) [Figure 4].
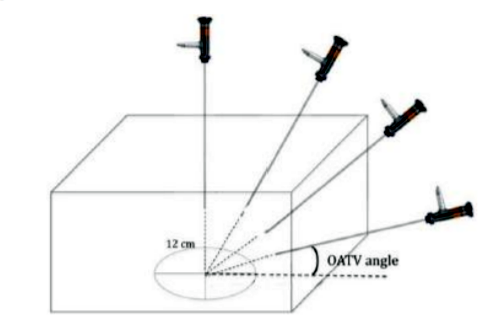
Four 11mm ports (Endopath Excel ® ports, Ethicon Endo Surgery, New Jersey, USA) were inserted along the midline to create optical-axis-to-view-angles (OATV) of 15°, 45°, 60° and 90° [Figure 5].
Hopkins 2 ® laparoscope (0°) (Karl Stortz Gmbh & Co. Tuttlingan, Germany) was positioned through the 11 mm ports and was positioned securely with flexible camera holder. The magnification of the endoscope was fixed for all participants and the distance from the tip of the endoscope to the centre of the working area was kept constant at 12cm for all OATV angles. Images were projected using Tele Pack ® (Karl Stortz © Gmbh & Co. Tuttlingan, Germany) which is an integrated and portable camera and light source system. The centre of the monitor screen was fixed at a distance of 100cm in front of the subjects. All experiments were conducted under the same illumination and environment.
The standard task involved using the sharp point of a laparoscopic scissor to make holes on a piece of white circular sheet (10 cm diameter) inside the laparoscopic box. Candidates were instructed to make holes on the target paper at specified distances away from the centre (Target distance). This ranged from 2cm to 8cm inclusive (2, 3, 4, 5, 6, 7, 8 cm). The task was performed in a clockwise fashion along eight different clock positions on the target paper (12:00, 1:30, 3:00, 4:30, 6:00, 7:30, 9:00, and 10:30) [Figure 4]. This was repeated for 4 OATV angles at 15°, 45°, 60° and 90°. The instructions for target distance, o’clock positions and OATV angles for candidates were randomised beforehand. Information about the size of paper was kept anonymous and its boundaries were kept out of view to minimise estimation.
Candidates used their best guess to mark the target (sheet of paper) based as per instructions, e.g. 4cm from the centre at 3 o’clock position. The primary endpoint was the target distance deficit (TDD), which was defined, as the difference (mm) between the instructed target distance (2, 3, 4, 5, 6, 7, or 8 cm) and the actual distance from the centre of the area marked by the candidates. This was measured using a standard ruler corrected to the nearest millimetre (mm). Results were recorded on a predesigned form with randomised number of each candidate. These forms were individually coded prior to the trial.
Based on previous similar studies 2,6 and literature review, power calculation suggested that 20 candidates should enable the detection of 20% difference in error numbers between the two groups with 80% power at p< 0.05. Both groups performed the task and target sheets were analysed by a different trainer. Target distance deficit was calculated for each group. The statistical package for the Social Sciences Software (version 17.0.0, SPSS Chicago, IL, USA) and Excel (Microsoft Excel®, Microsoft Corporation, Redmond, Washington, USA) were used for data collection and interpretation. Student t-test determined mean +/- standard error of mean (S.E.M) with 95% confidence interval to highlight statistical difference between groups (Scale vs Control). On graphic plots the target distance deficit (TD) is marked as + (mm) mean +/- sem, if the candidate overran the instructed distance and – (mm) mean +/- sem, if short of the instructed distance.
3. Results
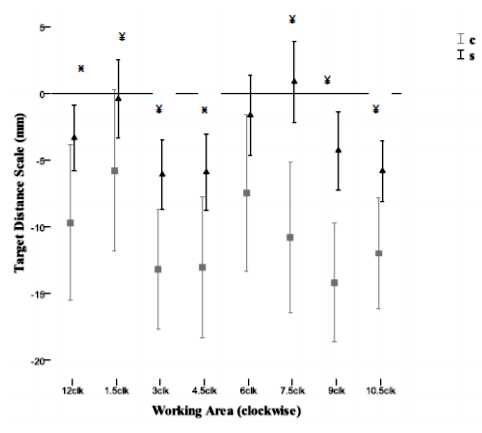
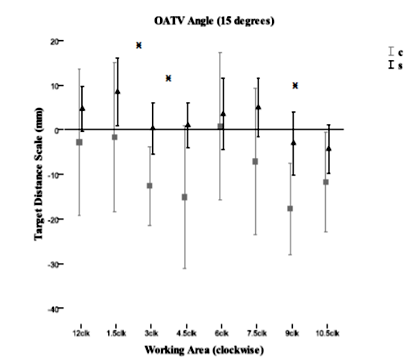
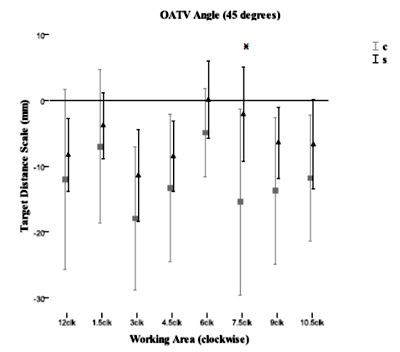
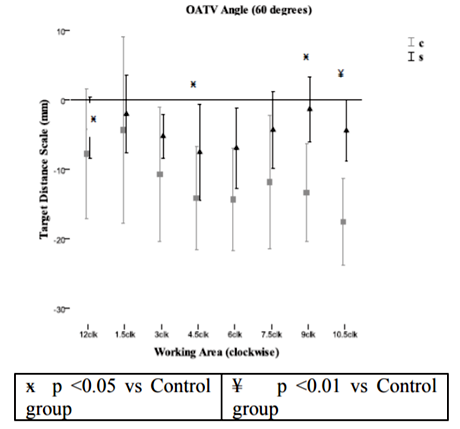
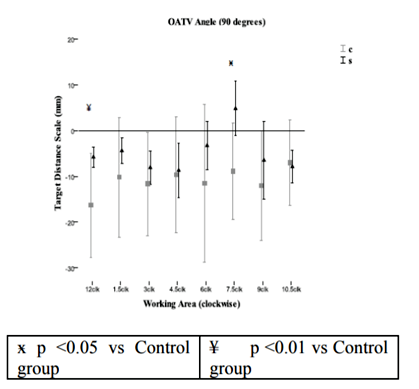
Results were analysed after plotting target distance deficit at individual OATV laparoscope positions i.e., 15, 45, 60 and 90 degrees [Figures 7,8,9,10] and at combined OATV angle [Figure 6] to study total difference between both groups (Scale vs Control).
4. Discussion
Conversion of 2-D visual display to 3-D image in the brain to create depth perception is a complex neural function which depends on many factors i.e., light, shadow, reflection etc. To move any instrument within the box and then make a mark, having calibrations on the instrument, is naturally going to facilitate that move by creating reference points for the eyes. But, to move the instrument to an object within that box that is at an undetermined distance is another issue and that is the difficulty with operating in a 2-D environment. The study design questioned this issue of understanding the learning of brain from unfixed visual references and its impact on laparoscopic performance.
Visual display plays a fundamental role in the outcome to any laparoscopic operation. Although, efforts to improve technical issues with laparoscopic visual metaphors are inspiring[13]; nevertheless, technology failed to provide any concrete solution to this issue of reduced depth perception. Role of 3-D visual display in literature proved controversial[4,5]. To master laparoscopic skills, a surgical trainee still relies on many years of hard work to overcome these physiological barriers. Impact of shortened surgical training time further introduces longevity in the proficiency achievement for specific laparoscopic procedures.
Results from this study also highlighted important factors influencing depth perception. One such factor is the optical axis to view angle and second, the working direction. Certain areas of abdominal cavity (directions) are difficult to view and anomalous depth perception complicates simple surgical skill like suturing even difficult. Calibration is best viewed when endoscope is positioned at 15 degrees OATV angle. Both groups achieved best outcome in terms of depth perception at 15 degrees OATV angle; still there was significant difference between both groups in three different directions [Table 1] [Figure 7]. 90 degrees OATV angle confirmed the worst performance from both groups. During laparoscopic surgery the normal OATV angle is 60 degrees with 0-degree scope. At this angle scale group performance at 12 o’clock, 1.5 o’clock is comparable to performance at 7.5 o’clock and 9 o’clock [Figure 9] which shows consistency in the method of improving depth perception through calibration.
The environment for conducting this experiment is far removed from a factual situation and cannot be justly equated in true surgical environment with the significance in the results obtained. There are several aids for perceiving depth in a real time situation. Therefore it remains to be seen if the experiment carries the same weight in a more natural environment.
5. Conclusion
Based on the results from this trial, it would be safe to support the argument in favour of instrument calibration in order to provide a reference point in operating field of vision. Although the results of this study are promising; nevertheless, they are far from proving the point in the complex anatomical environment of laparoscopic surgery. We would strongly urge to repeat the test in the vivo environment by comparing a simple laparoscopic task among junior surgical trainees.
References
- Blavier A, Gaudissart Q, Cadiere GB (2006) Impact of 2D and 3D visionon performance of novice subjects using da vinci robotic system. Acta chir belg 106: 662-664.
- Baudurdeen S, Abdul-Samad O, Story G, Wilson C, Down S, Harris A (2010) Nintendo Wii video-gaming ability predicts laparoscopic skill. Surgical Endoscopy 24: 1824-1828. DOI 10.1007/s00464-009-0862-z.
- Dion YM, Gaillard F (1997) Visual integration data and basic motor skills under laparoscopy: Influence of 2-D and 3-D video-camera system. Surgical Endoscopy. 11: 995-1000.
- Hanna GB, Cuschieri A (2000) Influence of two-dimensional and three dimensional imaging on endoscopic bowel suturing. World J. Surg. 24, 444-449. DOI: 10.1007/s002689910070.
- McDougall EM, Soble J, Wolf SJ (1996) Comparison of Three-Dimensional and Two-Dimensional Laparoscopic Video Systems. Journal of Endourology. 4: 371-374. Doi:10.1089/end.1996.10.371.
- Patel H, Ribal M.J, Arya M, Nauth-Misir R, Joseph J.V (2007) is it worth revisiting laparoscopic three-dimensional visualization? A validated assessment. 70: 47-49.http://dx.doi. org/10.1016/j.urology.2007 .03.014.