Information
Journal Policies
Mesh Related Infections in Hernia Surgery: A Case Report and Review of Literature
Agarwal Amit1*, Srivastava KN1
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction: Past few years have seen an increasing variety of non-infectious and infectious complications of mesh use in hernia surgery. This incidence is influenced by underlying co-morbidities, the type of mesh, the surgical technique and the strategy used to prevent infections. Important advances have led to the production of relatively inert and biocompatible surgical meshes. However, surgical meshes can trigger various responses when implanted in the human body.
Case Presentation: We present the case of a 62-year-old male who underwent B/L Laparoscopic inguinal hernia repair (TAPP) and presented 6 months after with high grade fever. He was found to have mesh related infection and was treated by drainage of pus with removal of infected mesh.
Discussion: Bearing the clinical significance of this condition it is best to prevent mesh infection at all costs. Various strategies have been described for the same. At present, adhering to strict asepsis and preoperative antibiotic is recommended in all cases while keeping other strategies as a reserve for high risk patients. Despite all measures such infections may occur in 1-8% of the cases. Treatment should be multimodality combining medical and surgical measures. If the infection is superficial with prosthesis not being involved, conservative measures with drainage of abscess and antibiotics maybe successful. However, most cases will require complete removal of mesh with drainage of abscess.
Conclusion: The possibility of a mesh-related infection occurring weeks or even years after hernia repair, should be considered in any patient with fever of unknown origin, or symptoms and/or signs of inflammation of the abdominal wall. Strategies should be devised to prevent it at source. If mesh infection develops it should be treated vigorously and mesh should be excised early if necessary.
Mesh infection, hernia, mesh removal, hernia infection,Surgery
1. Introduction
The use of a mesh in hernia surgery was first reported by Usher et al in 1958 [1]. Since then the use of mesh in hernia surgery has become a standard practice worldwide [2,3]. This has led to an increasing variety of non-infectious and infectious complications. These complications though rare, bear a significant clinical importance. They can be a cause of serious long term morbidity for the patient and cause significant stress to both the surgeon and the patient.
The mesh related complication include: Seroma, Adhesions, Chronic pain, Migration, Rejection, Infection Even though with the advent of technology, more and more biologically inert meshes are being devised every day, still, a foreign body in the human body can trigger any of the above reactions.
2. Case Report
We encountered a 62-year diabetic male who presented to us with high grade fever with chills and rigors. He had severe pain and swelling in the right inguinal region. the patient had undergone bilateral laparoscopic inguinal hernia repair (B/L TAPP) 6 months back. The adverse symptoms started 3 months after the surgery.
The initial ultrasound showed a purulent collection in relation to the right sided mesh. Aspiration of about 50ml of pus was done by the primary surgeon. Patient was also put on parenteral antibiotics including Amikacin and third generation Cephalosporins.
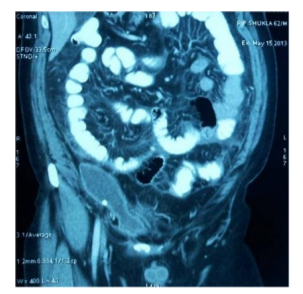
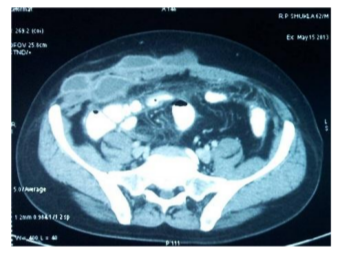
Despite this the fever and pain persisted. Patient also developed a progressive induration along the right inguinal region. On examination the patient was in sick general condition. He had a fever of 101.5 F. The abdomen was soft with no oraganomegaly. There was multiple tender indurated lumps in the right inguinal region reaching up to the right anterior superior iliac supine. A contrast enhanced CT scan was done (Figure. 1,2) which revealed loculated collections in the right side ant. abdominal wall in the inguinal region along the hernia mesh with associated adhesions. Fat stranding of omental and mesenteric fat planes was present. At least two other similar collections in the subcutaneous plane of the right lower anterior abdominal wall suggestive of abscess / pus collections were also seen. There was a thin rim of fluid in the pelvis.
The patient was optimized and exploration was done under spinal anesthesia. A large abscess cavity containing about 100ml pus in the sub cutaneous plane in the supra-pubic region was found (Figure. 3). Another abscess cavity in the right inguinal region beneath the external oblique aponeurosis, containing about 20ml pus and a third cavity containing about 50 ml pus in the retro pubic area along the mesh were also present. All he cavities were widely drained by a large inguinal incision. A free floating polypropylene mesh was found in the abscess cavity. Almost 90% of the right sided mesh was infected and free floating. This un-incorporated mesh was removed (Figure. 4). Only 10% of the mesh densely incorporated in the tissues on the medial most part was left behind. The wound was left open.
The patient was followed with daily dressings with I/V antibiotics followed by long term oral antibiotics. The overall healing was slow and it took 4 months for the wound to heal completely. At the end, there was no residual sinus. There was no recurrence till 1 year of the procedure.
3. Discussion
Important advances in medical technology have led to the production of relatively inert and biocompatible surgical meshes. However, surgical meshes can trigger various responses when implanted in the human body, including inflammation (foreign body reaction), fibrosis, calcification, thrombosis and infection.
Mesh-related infections following hernia surgery occur relatively infrequently. The reported incidence of mesh-related infection following hernia repair is variable in different studies ranging from 0.03 to 8% [4,5]. However, the actual incidence is unclear due to underreporting of such complications. These infections though rare bear significant clinical importance not only for the patients but also for the surgeons. They even become a cause of litigations due to the long morbidity involved.
Few factors have been implicated towards mesh related infections. These include: -
1. Underlying
2. co-morbidities
3. Diabetes
4. Immunosuppression
5. Obesity
6. Smoking
Meshes made of non-absorbable polymers have been used most frequently in clinical practice. Given the fact that absorbable polymers are associated less frequently with foreign body reactions and adhesion, the newer meshes are being made with a combination. Recent studies have indicated that weight of the mesh and pore size also have a bearing on the mesh related reactions in the body. Heavyweight meshes have a higher tensile strength and are stronger than lightweight meshes [6]. The use of heavyweight meshes is associated with increased complications and adverse events, such as fistula and adhesion formation and pain [7,8]. The pore size of the mesh also plays a role in the safety and tolerability of surgical meshes. The larger the pore the lesser will be the chances of seroma and infection, however the larger pore meshes will cause more adhesions and obstructive complications [7-9].
In most recent published trials, precise surgical approach did not influence the incidence of long-term complications significantly, including mesh infection. Several authors have suggested that the laparoscopic approach has fewer post- operative complications, especially in laparoscopic ventral hernia repair, however there are no clear, specific data [10].
The microbiology of mesh infection includes Staphylococcus spp., especially Staphylococcus aureus, Streptococcus spp. (including group B streptococci). Gram-negative bacteria (mainly Enterobacteriaceae), and anaerobic bacteria (including Peptostreptococcus spp.) may also be seen. Rarely, mesh infections are caused by Candida spp. or Mycobacterium spp [10].
The main characteristic of these infections is that they respond poorly to antimicrobial treatment regimens.
The interval between hernia repair and the manifestation of a mesh infection ranges from 2 weeks to 39 months in literature. The symptoms and signs of local acute inflammation are present including combination of pain, erythema, tenderness, swelling and increased temperature. Systemic signs like fever, malaise, chills or rigors may also be there. Late and rare manifestations include discharging sinus, intra-abdominal abscess and osteomylitis.
Considering the magnitude of this complication it is best to prevent it at source. One must adhere to strict asepsis. Foreign body reactions also depend a lot on the amount of the prosthesis mesh used[7].
In addition, four main approaches to the prevention of mesh infection have been described.
a. Intravenous perioperative administration of antimicrobial agents. Although hernia repair operations are classified as clean surgery, the administration of intravenous antibiotics perioperatively has shown to be beneficial
b. The wound can be rinsed with an antibiotic-containing solution, starting immediately after the dissection of the hernia sac, and then intermittently until the skin is sutured. It has been shown in an animal model that this approach inhibits the adhesion of bacteria to the surface of the mesh, as well as their growth.
c. Soaking of mesh in antimicrobial solutions like Vancomycin (reduced MRSA), Gentamycin or Rifampicin.
d. Use of material placed in front of the mesh to slowly deliver an antimicrobial agent locally or mesh containing embedded antimicrobial agents to prevent bacterial adhesion and colonization.
No definitive recommendation has yet been formulated. The perioperative administration of appropriate intravenous antibiotics has proven to be effective in reducing infections related to mesh in various trials [12,13]. This strategy should be used until new data regarding alternative preventive strategies becomes available. At the present time, additional strategies such as the use of gentamicin-laced collagen tampons with a mesh, are best reserved for patients at high risk of infection.
When a mesh-related infection occurs, a combined medical and surgical approach involving intravenous antimicrobial agents and surgical removal of the mesh is the preferred management strategy [14]. Monotherapy with intravenous antibiotics generally has a poor outcome. Conservative approach with drainage along with intravenous antibiotics and irrigation of the wound has been described. Superficial infections not directly involving the prosthesis can be expected to heal by this method. Incorporation of the meshes (polypropylene and polyester but not ePTFE) can usually be seen by 3-4 weeks. Excision is necessary only for the sequestered mesh. The integrated mesh can be left as such. Incomplete removal of the mesh should be suspected in any case with persistent or recurrent symptoms and/or signs of mesh infection.
The removal of the infected mesh generally does not result in recurrent herniation as sufficient fibrous scarring remains [15]. The same was seen in our case.
4. Conclusion
Though rare, mesh infections do occur and cause substantial morbidity. Clinicians should promptly consider the possibility of mesh infection in any patient who has undergone hernia repair surgery involving a mesh, and who has fever or symptoms and/or signs of infection of the abdominal wall. There is no adequate evidence in the literature concerning the specific risk factors for such infections. Whether the surgical technique used for the repair of a hernia or the precise type of implanted mesh influences the rate of development of a mesh-related infection also remains to be clarified. Strict asepsis with judicious use of antibiotics is recommended for prevention of mesh related infections. An approach that combines medical and surgical management is necessary for cases in which mesh infection occur. As of yet, there are no published reports of comparative trials of different antimicrobial regimens for the management of mesh-related infections. Consequently, no definitive recommendations can be made concerning the preferred medical management strategy. However, the therapy should at least include coverage for Staphylococcus. Complete removal of mesh with drainage of abscess remains the mainstay of treatment.
References
- Usher FC, Ochsner J, Tuttle LL., Jr Use of Marlex mesh in the repair of incisional hernias. Am Surg.1958;24:969–974.
- Vrijland WW, van den Tol MP, Luijendijk RW, Hop WC, Busschbach JJ, de Lange DC, et al. Randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br J Surg.2002;89:293–297.
- Lichtenstein IL, Shulman AG, Amid PK, Montllor MM. The tension-free hernioplasty. Am J Surg.1989;157:188–193.
- Gilbert AI, Felton LL. Infection in inguinal hernia repair considering biomaterials and antibiotics. Surg Gynecol Obstet. 1993; 177:126–130.
- Shulman AG, Amid PK, Lichtenstein IL. The safety of mesh repair for primary inguinal hernias: results of 3,019 operations from five diverse surgical sources. Am Surg. 1992; 58:255–257.
- Hollinsky C, Sandberg S, Koch T, Seidler S. Biomechanical properties of lightweight versus heavyweight meshes for laparoscopic inguinal hernia repair and their impact on recurrence rates. Surg Endosc.2008;22:2679–2685. doi: 10.1007/s00464-008-9936-6.
- Klosterhalfen B, Junge K, Klinge U. The lightweight and large porous mesh concept for hernia repair. Expert Rev Med Devices. 2005; 2:103–117.doi: 10.1586/17434 440.2.1.103.
- Miller K, Junger W. Ileocutaneous fistula formation following laparoscopic polypropylene mesh hernia repair. Surg Endosc. 1997; 11:772–773. doi: 10.1007/s0046 49900448.
- Horstmann R, Hellwig M, Classen C, et al. Impact of polypropylene amount on functional outcome and quality of life after inguinal hernia repair by the TAPP procedure using pure, mixed, and titanium-coated meshes. World J Surg. 2006;30:1742–1749. doi: 10.1007/s002 68-005-0242-3.
- Rodrigo Gonzalez, Edward Mason, Titus Duncan, Russell Wilson, Bruce J. Ramshaw. Laparoscopic Versus Open Umbilical Hernia Repair, JSLS. 2003 Oct-Dec; 7(4): 323–328.
- Taylor SG, O'Dwyer PJ. Chronic groin sepsis following tension-free inguinal hernioplasty. Br J Surg.1999;86:562–565.
- Kuzu MA, Hazinedaroglu S, Dolalan S, Ozkan N, Yalcin S, Erkek AB, et al. Prevention of surgical site infection after open prosthetic inguinal hernia repair: efficacy of parenteral versus oral prophylaxis with amoxicillin-clavulanic acid in a randomized clinical trial. World J Surg. 2005;29:794–799.
- Yerdel MA, Akin EB, Dolalan S, Turkcapar AG, Pehlivan M, Gecim IE, et al. Effect of single-dose prophylactic ampicillin and sulbactam on wound infection after tension-free inguinal hernia repair with polypropylene mesh: the randomized, double-blind, prospective trial. Ann Surg. 2001;233:26–33.
- Tolino MJ, Tripoloni DE, Ratto R, Garcia MI. Infections associated with prosthetic repairs of abdominal wall hernias: pathology, management and results. Hernia. 2009;13:631– 637
- Bellon JM, Bujan J, Contreras L, Hernando A, Jurado F. Macrophage response to experimental implantation of polypropylene prostheses. Eur Surg Res. 1994;26:46–53.