Information
Journal Policies
Comparison of Monopolar and Segmental Radiofrequency Ablation in the Treatment of Lower Limb Chronic Venous Insufficiency
Jun-Yi Ryan TAN, Zhiwen Joseph LO, Pravin LINGAM, Qiantai HONG, Enming YONG, Sadhana CHANDRASEKAR, Glenn Wei Leong TAN
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction: There are 4 commercially available RFA systems for endovenous ablation of lower limb varicose veins. We aim to compare outcomes in patients with chronic venous insufficiency treated by monopolar (EVRF®, F Care Systems, Belgium) and segmental (ClosureFast™, Medtronic, USA) radiofrequency ablation (RFA)
Methods: Retrospective review of 288 limbs (189 patients) treated from 2014-2015, evaluating demographics, comorbidities, venous disease grading, pre-operative venous duplex, surgical procedure and post-operative outcomes.
Results: 146 limbs were treated by monopolar RFA, 142 limbs by segmental RFA. Both groups were similar in patient characteristics. In addition to long saphenous vein ablation, anterior accessory great saphenous vein (AAGSV) (monopolar: 20%, segmental: 10%, p=0.01) and short saphenous vein RFA (monopolar: 14%, segmental: 8%, p=0.14) were performed. Post-operative outcomes were similar in both groups. Transient superficial neuropathy was 8% in both groups (p=0.83), phlebitis occurred in 4% of monopolar group and 1% of segmental group (p=0.28). No deep vein thrombosis nor recurrences occurred.
Conclusion: Both monopolar and segmental RFA are safe and efficacious. The shorter ablation tip of monopolar RFA enables the ease for ablation of shorter veins, such as the AAGSV.
Endovenous Radiofrequency Ablation, Varicose Veins, Chronic Venous Insufficiency, Anterior Accessory Great Saphenous Vein.
Chronic venous insufficiency (CVI) is a prevalent issue, affecting an average of 10-15% of men and 20-25% of women worldwide1. Surgical treatment of lower limb CVI has progressed greatly since the days of open ligation and stripping to more minimally invasive procedures such as foam sclerotherapy and most recently endothermal ablation technologies such as endovenous laser therapy (EVLT) and endovenous radiofrequency ablation (RFA) [2]. EVLT and RFA have recently been recommended as first-line interventions for CVI by 2013 NICE guidelines [3] and have been shown to be superior to open surgery and foam sclerotherapy [4]. 4 main RFA systems are available commercially - Covidien ClosureFast™.
(Medtronic, USA), EVRF® (F Care Systems, Belgium), RFiTT® (Celon AG, Germany) and VeinClear™ (RF Medical, South Korea). Covidien ClosureFast™, a segmental RFA system, and EVRF®, a monopolar RFA system, have both been shown to be safe and efficacious [5,6]. However, a recent 2015 meta-analysis on the 4 commercially available RFA systems revealed far fewer publications [7] on EVRF® data as compared to Covidien ClosureFast™, with no previous direct comparisons of the monopolar and segmental systems. As such, in our study we aim to bridge this gap in existing knowledge by comparing the outcomes in patients with lower limb CVI treated with monopolar (EVRF ®, F Care Systems, Belgium) versus segmental (Covidien® ClosureFast™, Medtronic, USA) radiofrequency ablation (RFA) therapy.
2. METHODS
This study was a retrospective analysis of a total of 288 limbs treated with endovenous RFA from January 2014 to May 2015 at a 1,500-bed tertiary referral university hospital. Factors investigated included patient demographics, co-morbidities, venous disease clinical manifestation (CEAP Classification), pre-operative venous duplex mapping, surgical procedure and post-operative outcomes. Patient co-morbidities were determined by American Society of Anaesthesiologists (ASA) Classification, smoking history, type 2 diabetes mellitus and control, peripheral arterial disease and previous venous surgery.
All patients were encouraged to undergo a trial of lifestyle modification and graduated compression stockings before surgical intervention. Patients with C6 venous disease were treated with 4-layer compression bandaging to promote ulcer healing prior to any surgical intervention. The decision for treatment with segmental or monopolar RFA was based on surgeon’s preference. All procedures were carried out by trained consultant vascular surgeons who were experienced and proficient in both systems.
Pre-operatively, patients routinely underwent venous duplex mapping at our local vascular diagnostic laboratory by trained vascular scientists according to Society of Vascular Ultrasound guidelines, using Philips iU22 ultrasound machines (Philips, USA). Sapheno- femoral junction (SFJ) incompetence, great saphenous vein (GSV) reflux, sapheno-popliteal junction (SPJ) incompetence, short saphenous vein (SSV) reflux and deep venous reflux were assessed in the venous duplex mapping. Anterior accessory great saphenous vein (AAGSV) incompetence is also evaluated as part of the diagnostic protocol.
All cases were carried out under general or regional anaesthesia, with no routine intravenous pre-operative antibiotics or pharmacological deep vein thrombosis prophylaxis given. Ultrasound-guided venous punctures were performed with Philips iU22 ultrasound machines (Philips, USA). Access was achieved at below knee GSV under ultrasound guidance with a 21G needle, after which a 7F sheath was inserted using the Seldinger technique and flushed with heparinised saline. Tumescent anaesthesia (480ml of saline mixed with 20ml 1% lignocaine, 16ml 8.4% sodium bicarbonate and 60 units 1:1000 adrenaline) was administered prior to endovenous ablation. Intra-operatively, ablation of the AAGSV would be attempted if reflux were found, while SSV reflux was treated only with the concomitant presence of SPJ incompetence.
In the monopolar group, the EVRF® RFA system (F Care Systems, Belgium) with the CR45i catheter were used for ablation. The CR45i catheter delivers power of up to 25W and has an active catheter tip of 0.5cm. The CR45i catheter was inserted and positioned 2cm from the SFJ. Ablation of the GSV was carried out at 25W within the fascia envelope and at 22W when not enveloped by fascia. A pull-back technique was employed for ablation and the pull-back rate was 0.5cm (1 marking) every 3 beeps (5- 6seconds) as per manufacturer instructions for use.
In the segmental group, the ClosureFast™ system (Medtronic, USA) was used with a ClosureFast™ Endovenous RFA catheter and ClosureRFG™ radiofrequency generator. The ClosureFast™ catheter has a 3cm or 7cm active catheter tip and in view of financial considerations, only 1 is utilized for each patient. The ClosureFast™ catheter was inserted and positioned 2cm distally from the SFJ. Ablation was carried out in 20-second cycles from 40W (120°C) to 10W. Two cycles were applied for the initial 7cm segment and one cycle per segment subsequently. The catheter was pulled back at 2.5cm or 6.5cm intervals after each ablation cycle to allow for a 0.5cm segment of overlap, as per manufacturer guidelines.
All patients had an on-table ultrasound post- procedure to ensure complete ablation of GSV and to ensure the absence of deep vein thrombosis within the femoral vein. All procedures were completed with stab avulsion phlebectomies. Incision sites were closed with Steri-Strips™ (3M, USA) and dressed with 3M Coban™ 2 Layer Compression bandage (3M, USA). This bandage would be removed on post- operative day 1, exchanged for a light-weight stocking TubigripTM (Molnlycke Health Care, Sweden) and continued until review in clinic. Oral paracetamol or non-steroidal anti- inflammatory drugs were prescribed for post- operative analgesia. Patients were reviewed in clinic 6 weeks post-operatively and assessed clinically for symptoms of complications such as transient neuropathy, phlebitis, deep venous thrombosis and clinical recurrences. Repeat ultrasound venous duplex mapping will be performed should there be any suspicion for clinical recurrences.
Factors investigated were evaluated using descriptive statistics. Percentages were used for categorical data and means for continuous data. Comparisons between groups for categorical data were made using Chi-square tests, while comparisons made between continuous data were made with the Student’s t-test. All p values were 2 tailed and p values ≤0.05 were considered statistically significant. SPSS 13.0 (Illinois, USA) was used for statistical analysis.
3. RESULTS
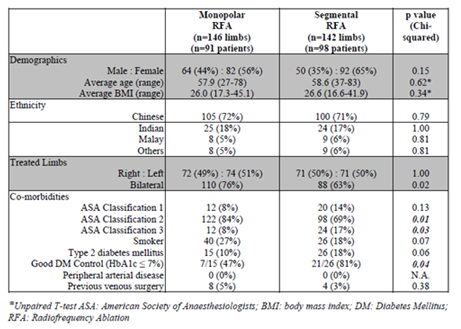
From January 2014 to May 2015, 189 patients (288 limbs) were treated with endovenous radiofrequency ablation at our institution (Table 1). There was an equal distribution between both treatment modalities, with 146 limbs treated with monopolar RFA and 142 limbs treated with segmental RFA. Of these, 55 patients (110 limbs) of the monoplar group and 44 patients (88 limbs) of the segmental group had bilateral chronic venous insufficiency that was treated.
Both groups were largely similar in terms of patient demographics and comorbidity profile (Table 1). The mean age of our patients was 58 (27 - 83) years while the mean Body Mass Index was 26.3 (16.6 - 45.1) kg/m2. Of the 288 limbs treated, 174 were female while 114 were male. Majority of patients were of American Society of Anesthesiologists (ASA) Class I and II (92% in monopolar and 83% in segmental) while we had few smokers (27% in monopoolar and 18% in segmental) and Type 2 diabetics (10% in monopolar and 18% in segmental). Significantly, no patients had concomitant arterio-venous disease. Minority had undergone previous venous surgery (5% in monopolar and 3% in segmental).
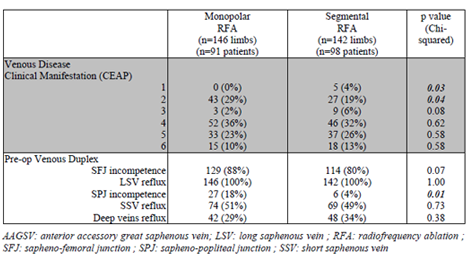
In terms of pre-operative CEAP venous disease manifestation (Table 2), within the monopolar group patients with C2-C5 disease were 29%, 2%, 36%, 23%, 10% respectively. Similarly in the segmental group, patients with C1-C6 disease were 4%, 19%, 6%, 32%, 26% and 13% respectively. On pre-operative venous duplex scanning, all limbs treated had GSV reflux, majority had SFJ incompetence (88% in monopolar, 80% in segmental, p=0.07) while half had SSV reflux (51% in monopolar and 49% in segmental, p=0.73) and a third had concomitant deep venous reflux (29% in monopolar and 34% in segmental, p=0.38).
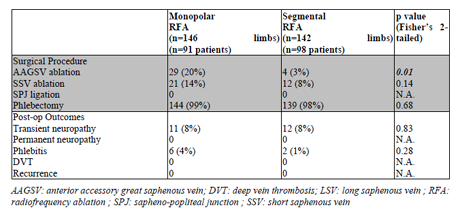
There was a significant difference between the veins ablated in both groups. All patients underwent LSV radiofrequency ablation. However, in addition to LSV RFA, there were significantly far more in the monopolar group that had undergone AAGSV ablation as compared to the segmental group (Table 3). 29 (20%) limbs in the monopolar group underwent AAGSV ablation as compared to only 4 (3%) in the segmental group and this was found to be statistically significant by chi squared analysis (p=0.01). A similar trend is seen in SSV ablations, with 21 (14%) ablated in the monopolar group compared to 12 (8%) in the segmental group. Almost all patients underwent phlebectomies, 144 (99%) in the monopolar group and 139 (98%) in the segmental group. Post-operative complications were few and there were no statistical differences between both groups. There were 11 (8%) limbs with transient neuropathy in the monopolar group and 12 (8%) in the segmental group. None of the patients developed permanent neuropathy. There were 6 (4%) with phlebitis in the monopolar group compared to 2 (1%) in the segmental group. There were significantly no incidences of deep venous thrombosis or clinical recurrences within both groups (Table 3).
4.DISCUSSION
Within the literature, this is the first study which directly compared monopolar and segmental radiofrequency ablation for lower limb CVI. Our study is also the largest series of monopolar radiofrequency ablation for lower limb CVI within Asia. The most significant finding of our study was that more short vein ablations, such as AAGSV ablations, were carried out with the monopolar system. The AAGSV was ablated in 20% of ablations carried out in the monopolar group as compared to only 3% in the segmental group. This is likely a result of the shorter, 0.5cm active catheter tip of the of the monopolar EVRF® system, which has a 0.5cm active catheter tip as compared to the 3cm or 7cm active catheter tip of the ClosureFast™ catheter. In current literature, there is a low reported rate of AAGSV ablations in most studies [5,8], ranging from 2.7% - 10% in various studies on endothermal ablation. Ablation of the AAGSV is not well studied although incidence of isolated AAGSV reflux has been reported at 10% [9] and its clinical significance has been suggested in its role in causing recurrence after GSV ablation or stripping [10-12] although currently, there is no consensus on its treatment, even in the absence of reflux.
Similarly, in our study we saw a similar trend in more SSV ablations carried out in the monopolar group (14%) as compared to the segmental group (8%), and this is consistent with that described in existing literature - in a 2015 study on the monopolar system by Spiliopoulos et al [5] 14.8% of procedures involved ablation of the SSV, while only 5% were ablated in a 2015 segmental study [13].
Our study’s findings also further reiterate the safety and efficacy of radiofrequency ablation as a treatment modality for lower limb CVI, demonstrating favourable surgical outcomes with low rates of post-operative complications in both the segmental and monopolar groups with no significant differences between both groups. Our study had no incidences of deep venous thrombosis and clinical recurrences, which is in keeping with existing literature that shows a < 1% risk of deep venous thrombosis [14]. In our series there was a 2.7% incidence of post-operative phlebitis, in keeping with current reported literature of 0.8 - 5.5%6, [15]. However, although our study reported a low rate of 8% incidence of transient neuropathy in both groups, existing literature has reported slightly lower rates of post-operative transient neuropathy, with 3-5% and 2% reported in segmental [6,15,16] and monopolar [5] studies respectively. Notably none of the incidences of transient neuropathy were permanent in our study and in reported literature. A possible explanation for the slightly higher incidence in transient neuropathy in our series, although still low, compared to that of existing literature could be in the ethnic differences in our patients, with 71.5% of Chinese descent, which has anecdotally been associated with a higher incidence of incomplete fascial covering over the GSV.
Limitations of our study include the retrospective nature of our study design, with its associated selection and information biases. In terms of chronic venous insufficiency grading, we adopted the CEAP classification and did not use the venous severity score. Post-operative recurrences were evaluated clinically, with no formal surveillance ultrasound venous duplex. We also were not able to compare the efficacy of the other 2 endovenous radiofrequency ablation devices on the market.
5. CONCLUSION
Both monopolar and segmental RFA are safe endovenous modalities in the treatment of lower limb CVI, with similar clinical outcomes and low complication rates. The significant advantage of monopolar over segmental RFA would be its shorter active catheter tip of 0.5cm, which enables the ease for ablation of shorter veins, such as the AAGSV.
6.REFERENCES
- Callam MJ. Epidemiology of varicose veins. Br J Surg. 1994;81(2):167-73.
- Van den Bremer J, Moll FL. Historical overview of varicose vein surgery. Ann Vasc Surg. 2010;24(3):426-32.
- National Institute for Health and Care Excellence (NICE). Varicose veins: diagnosis and management. 2013 [Clinical Guideline 168]: Available from: http://guidance.nice.org.uk/CG168.
- Van den Bos R, Arends L, Kockaert M, et al. Endovenous therapies of lower extremity varicosities: a meta-analysis. J Vasc Surg. 2009;49(1):230-9.
- Spiliopoulos S, Theodosiadou V, Sotiriadi A, et al. Endovenous ablation of incompetent truncal veins and their perforators with a new radiofrequency system. Mid-term outcomes. Vascular. 2015;23(6):592-8.
- Proebstle TM, Vago B, Alm J, et al. Treatment of the incompetent great saphenous vein by endovenous radiofrequency powered segmental thermal ablation: first clinical experience. J Vasc Surg. 2008;47(1):151-6.
- Goodyear SJ, Nyamekye IK. Radiofrequency ablation of varicose veins: Best practice techniques and evidence. Phlebology. 2015;30(2 Suppl):9-17.
- Krnic A, Sucic Z. Bipolar radiofrequency induced thermotherapy and 1064 nm Nd:Yag laser in endovenous occlusion of insufficient veins: short term follow up results. Vasa. 2011;40(3):235-40.
- Theivacumar NS, Darwood RJ, Gough MJ. Endovenous laser ablation (EVLA) of the anterior accessory great saphenous vein (AAGSV): abolition of sapheno-femoral reflux with preservation of the great saphenous vein. Eur J Vasc Endovasc Surg. 2009;37(4):477-81.
- Garner JP, Heppell PS, Leopold PW. The lateral accessory saphenous vein - a common cause of recurrent varicose veins. Ann R Coll Surg Engl. 2003;85(6):389-92.
- Proebstle TM, Mohler T. A longitudinal single- center cohort study on the prevalence and risk of accessory saphenous vein reflux after radiofrequency segmental thermal ablation of great saphenous veins. J Vasc Surg Venous Lymphat Disord. 2015;3(3):265-9.
- Bush RG, Bush P, Flanagan J, et al. Factors associated with recurrence of varicose veins after thermal ablation: results of the recurrent veins after thermal ablation study. ScientificWorldJournal. 2014;2014:505843.
- Broe M, Shaikh FM, Leahy A. Endovenous radiofrequency ablation: no value in short-term duplex ultrasound follow-up. Ir J Med Sci. 2015;184(3):641-5.
- Marsh P, Price BA, Holdstock J, et al. Deep vein thrombosis (DVT) after venous thermoablation techniques: rates of endovenous heat-induced thrombosis (EHIT) and classical DVT after radiofrequency and endovenous laser ablation in a single centre. Eur J Vasc Endovasc Surg. 2010;40(4):521-7.
- Dermody M, O'Donnell TF, Balk EM. Complications of endovenous ablation in randomized controlled trials. J Vasc Surg Venous Lymphat Disord. 2013;1(4):427-36 e1.
- Creton D, Pichot O, Sessa C, et al. ClosureFast Europe G. Radiofrequency-powered segmental thermal obliteration carried out with the ClosureFast procedure: results at 1 year. Ann Vasc Surg. 2010;24(3):360-6.