Information
Journal Policies
Terminal Ileal Necrosis with Mesentery Avulsion Secondary to Meckel Mesodiverticular Band. Case Report
Del Carmen Ortega Ignacio1, Sanchez Dauth Dulce Maria2, Gonzalez Villegas Hedler Olaf3, Gonzalez Valdez Luis Alberto4, Rodriguez Bautista Julio Orlando5, Serrano Ramos Javier Enrique6, Monroy Cedillo Jose Lius1, Marcos Irving Salazar Jimenez1*
2.Hospital Christus Muguerza del Parque
3.UMAE IMSS Leó Guanajuato
4.Hospital General Dr. Ruben Leñero
5.Hospital Regional de Petróleos Mexicanos Salamanca, Guanajuato
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background: The Meckel’s diverticulum is the most frequent congenital anomaly of the gastrointestinal tract. The mesodiverticular band is an embryological remnant of the vitelline circulation, when it cannot be obliterated, it can cause complications such as intestinal obstruction, among others.
Material And Methods: Male of 58 years-old, comes to the emergency room by a clinical picture of intestinal occlusion, with an internal hernia in the CT scan. For this diagnosis, an exploratory laparotomy is performed finding the presence of a Meckel's diverticulum conditioning terminal ileal necrosis.
Conclusion: The present case is a rare entity, especially in the adulthood, but the Meckel's diverticulum is manifested by complications that almost always require emergency surgical intervention.
Meckel's Diverticulum, Ileal necrosis, Intestinal obstruction, Mesodiverticular band,Surgery
The Meckel’s diverticulum is the most frequent congenital anomaly of the gastrointestinal tract. It appears secondary to the incomplete occlusion of the omphalomesenteric duct, that normally happens between the 7th and 8th week of gestation[1], it is a real diverticulum of the small bowel, containing mucosa, submucosa and muscularis propia[2].
In the worldwide literature this disease is associated with a rule called the “rule of the 2”, because it is presented in the 2% of population, with 2 inches of length, at 2 inches from the ileocecal valve, usually is presented before two years of age and contains 2 different ectopic tissues ( pancreatic and gastric are the most frequent, with the first in near 80% of the cases). It occurs at the same frequency in both sexes, but the complications are more frequent in males3. Secondary to the classic presentation in the pediatric age is unusual to consider this diagnosis in the adulthood, in which it is silent or with unspecific clinical courses mimicking other intraabdominal diseases, making this a diagnostic challenge[2,4].
The three clinical images associated with Meckel’s diverticulum are inflammation, low gut bleeding or intestinal obstruction. There are many mechanisms that can precipitate the intestinal obstruction, like the volvulus of small bowel around a fibrous band that is connecting the diverticulum to the umbilicus, the intestinal invagination, and the Littre hernia[5].
2. Case Report
Male of 58 years-old, without chronic diseases or surgical background, comes to emergency room for abdominal pain located in the hypogastrium with an intensity of 6/10 in the visual analog scale, accompanied with anorexia, and adynamia. He denied having nausea, vomiting or fever, with the last evacuation 2 days previous to consultation. Is evaluated and discharged with prokinetic management, but the abdominal pain increase and returns 6 hours later, is evaluated and hospitalized for study.
A physical exam with Glasgow of 15 points, with abdominal distention, at palpation with a soft abdomen, painful at media and deep palpation in lower hemiabdomen, with tympanic sound in upper hemiabdomen. In his lab test he presented leukocytosis 17.8x103/ml, neutrophils 15.6x103/ml (87.4%), hemoglobin 19.6 gr/dl, hematocrit 59.1%, platelets 300 x103/ml, creatinine 1.52 mg/dl and lactate 5.8mmol/l.
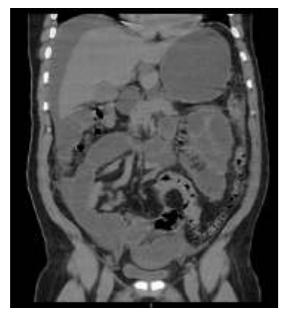
In the plain abdomen x-rays in two projections, we observed dilation of small bowel loops, the abdominal ultrasound with abundant liquid in small intestinal loops and diameter of 3.1 cm, interloop free liquid in the subdiaphragmatic right space and subhepatic space. In the CT scan, we observe a small bowel occlusion with a central transition zone in the mesogastrium, probably secondary to an internal hernia (Figure. 1), the free liquid in the peritoneal space (Figure. 2). After the location of the nasogastric tube, it drained 2000 ml of fecaloid aspect liquid. According to clinical and CT scan findings, an exploratory laparotomy is performed.
Surgical findings include small bowel loops dilated, with a Meckel’s diverticulum at 50cm of the ileocecal valve (Figure. 3) (Figure. 4). We observed a flange to the terminal ileum producing twisting and avulsion of the mesentery, with ileal necrosis of about 150cm (Figure. 5); an intestinal resection of the affected segment is completed at 40cm from the ileocecal valve and 140cm from the Treitz angle, with ileal-ileal anastomosis in a lateral-lateral fashion with stapler, and incidental appendectomy is completed too and an open drain placed to the pelvic hollow.
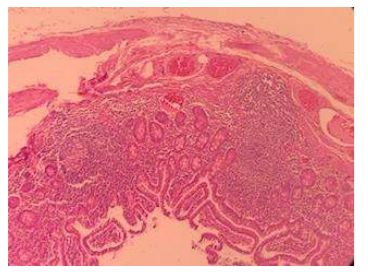
Post-surgical management includes fasting for three days, antibiotic and analgesic medication. The nasogastric tube was withdrawn on the third day, with an introduction with a liquid diet and the next day soft diet, with discharge at fourth day after surgery without complications, and posterior follow up in the external consult, where the pathologic report confirm the diagnosis (Figure.6).
Initially, the Meckel`s diverticulum was described by Fabricius Hildanus in 1598, posteriorly in 1809 by Johann Friedrich Meckel, who described extensively the anatomy and embryology, and for this reasons, this pathology receives their eponymous[6].
The mesodiverticular band is an embryologic remnant of the vitelline circulation that brings the arterial blood to the Meckel’s diverticulum. In the case of an absence of involution, an arterial band persists and it extends from the mesentery to the vertex of the antimesenteric border of the diverticulum, creating an opening across which the intestinal loops can herniate and produce an intestinal obstruction. This kind of internal hernia is a very rare cause of small bowel obstruction[6,7].
In adults, the most frequent location of the Mechel’s diverticulum is the antimesenteric border of the ileum, at E 60-100 cm from the ileocecal valve, different than the location in the child (30-60 cm)[6].
In the list of intestinal obstruction, the congenital anomalies like the presence of a mesodiverticular band represent less than 1% of the cases[8].
The integral diagnosis, with the abdominal CT scan as the gold standard for evaluation, with a sensibility of 90-95% and specificity of 96% for the diagnosis of small bowel obstruction, and that in 95% of cases it locates the exact site of obstruction and the etiology, in addition to indirect signs of intestinal hypoperfusion[9-11].
About the surgical treatment, the surgical resection with diverticulectomy or segmental resection of ileum with anastomosis is the best option of treatment. In our case, the segmentary resection was performed by the ischemic necrosis of the intestinal segment affected with ileal-ileal anastomosis. The laparoscopic surgical management depends on the surgeon habilities and the hospital resources but seems an excellent option in this cases[12].
4. Conclusion
The Meckel's diverticulum is a low-frequency gastrointestinal tract pathology, however, the clinical presentation is characterized by the associated complications. There is no need for a specialized test when the clinical suspicious is present and the surgical management must not be delayed. The incidental appendectomy is indicated in all the cases.
References
- Paras K. Pandove, Ashish Moudgil, Megha Pandove, Chandrashekhar, Divya Sharda, Vijay K. Sharda. Meckel’s diverticulum mesentery along with its band forming a hernial sac: A rare case of internal herniation. International Journal of Surgery Case Reports 10 (2015) 17–19. Mazin Al Janabi, Madan Samuel, Andrea Kahlenberg, Sujith Kumar and Mina Al-Janabi. Symptomatic pediatric Meckel’s diverticulum: stratified diagnostic indicators and accuracy of Meckel’sscan.NuclearMedicine Communications 2014, 35:1162–1166. Andrew A.H. Hadeed, Robert R.A. Azar, Nabiel N.A. Azar, Brion Benninger. Meckel’s diverticulum complicated by axial torsion and gangrene. Journal of Surgical Case Reports, 2015; 3, 1–3.
- Aziz Sumer, Ozgur Kemik, Aydemir Olmez, A. Cumhur Dulger, Ismail Hasirci, Umit Iliklerden, Et. Al. Small Bowel Obstruction due to Mesodiverticular Band of Meckel's Diverticulum: A Case Report. Case Reports in Medicine. 2010. Volume 2010, 1-3. Y. Narjis, H. Halfadl,A. Agourram, K. Rabbani, B. Finech. A Rare Internal Herniation in Adult: Meckel’s Diverticulum. Indian J Surg (2014) 76(1):5–7.
- C.R. López-Lizárraga, M.P. Sánchez-Muñoz, G.E. Juárez-López, L. Pelayo-Orozco, L.F. De la Cerda-Trujillo, C.F. Ploneda-Valenciaa A rare case of a strangulated Littre’s hernia with Meckel’s diverticulum. International Jornal of Surgery Case Reports 33 (2017) 58-61.
- Mirko Bertozzi, MD, PhD, Berardino Melissa, MD, Elisa Magrini, MD, Giuseppe Di Cara, MD, Ph.D., Susanna Esposito, MD, Antonino Apignani, MD, Ph.D. Obstructive internal hernia caused by mesodiverticular bands in children. Medicine (2017) 96:46.
- Gustavo Capelão, Miguel Santos, Sandra Hilário, Mónica Laureano, João Nobre, Inês Gonçalves. Intestinal Obstruction by Giant Meckel’s Diverticulum. GE Port J Gastroenterol 2017; 24: 183–187.
- Alexandra Platon, Pascal Gervaz, Christoph D. Becker, Philippe Morel, Pierre-Alexandre Poletti. Computed tomography of complicated Meckel’s diverticulum in adults: a pictorial review. Insights Imaging (2010) 1:53–61.
- Jae Min Lee, Chan Dong Jeen, Seung Han Kim, Jong Soo Lee, Seung Joo Nam, Hyuk Soon Choi, Et. al. Meckel’s diverticulum detected by computed tomographic enterography: Report of 3 cases and review of the literature. Turk J Gastroenterol 2014; 25: 212-5
- V K Kotha, MD, A Khandelwal, MD, S S Saboo, MD, Frcr, A K P Shanbhogue, MD, V Virmani, MD, Frcr, E C Marginean, MD, Et. al. Radiologist’s perspective for the Meckel's diverticulum and its complications. Br J Radiol 2014;87:1
- Chee S. Wong, Leanne Dupley, Haren N. Varia, Darek Golka, Thu Linn.Meckel’s diverticulitis: a rare entity of Meckel’s diverticulum. Journal of Surgical Case Reports, 2017;1, 1–3.