Information
Journal Policies
Giant Pancreatic Pseudocyst with Laparoscopic Management, Case Report
Medina Andrade Luis Angel1,Guillermo Antonio Garcia Barajas2,Vallejo Ramirez Jose Eduardo3,Haizel Valencia Romero4,Cesilia Vez Felix5,Hisela Viridian Flores Galicia6,Pamela Valencia Uribe7,Astrid Alvarez Alvarado8,Yazmin Samaniego Martinez9,Carlos Eduardo Rodriguez Rodriguez10,Eduardo Vidrio Duarte11
2.México National Autonomous University UNAM, General Zone Hospital 1A Rodolfo de Mucha Macias, México City, México.
3.México Valley University, UVM, General Zone Hospital 1A Rodolfo de Mucha Macias, México City, México.
4.La Salle University, Angeles Metropolitano Hospital, México City, México.
Copyright :© 2017 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Pancreatic pseudocyst is a frequent complication after acute or chronic pancreatitis, and in 15% it needs some endoscopic or surgical intervention to resolve.
We present the case of a female of 27 years-old consulting after having mild acute biliary pancreatitis three months ago, and a laparoscopic cholecystectomy after this. She complains of persistent abdominal pain of low intensity, with early postprandial fulfill and a decrease in weight for about 4 kilograms the last month. At physical exam a solid mass of about 10 centimeters could be perceived at deep palpation in epigastrium, with mild pain, it can’t be mobilized and was not compressible, with regular borders. CT scan was requested, reporting a collection in the front wall of the pancreas, with a thick wall (5mm) and heterogeneous content, predominantly hypo-echogenic, of 119x65x60 mm and a volume of 241 cc. A laparoscopic cysto gastroanastomosis was scheduled. The cystogastro anastomosis was completed by a transgastric approach without complications. Total surgical time was 160 minutes, with bleeding of 30cc. After surgery patient underwent fasting for 3 days and at fourth day liquid diet was introduced. Patient was discharged at day 5 uneventfully and at 1 month follow up she stills asymptomatic.
The cystogastric anastomosis as treatment of pancreatic pseudocyst is feasible and safe in hands with proper training.
Acute pancreatitis complications,Pancreatic pseuodocyst, laparoscopic gastro-cyst anastomosis,Surgery
Pancreatic pseudocyst is a complication frequently observed after acute or chronic pancreatitis in 2-10% and 10-30% respectively[1]. The 2012 Revised Atlanta Classification of Acute Pancreatitis defined pancreatic pseudocysts as well-circumscribed, completely encapsulated fluid collections of more than 4 weeks old; surrounded by a non-epithelial wall of fibrous or granulation tissue; homogeneous and without a non-liquid component; and arising as a consequence of acute pancreatitis, chronic pancreatitis, or pancreatic trauma with pancreatic ductal disruption[2,3]. Up to 85% of this lesions have an spontaneous resolution within 4 to 6 weeks4. Symptoms include abdominal pain, postprandial fullness, weight loss, and intestinal occlusion. As for the laboratories we can observe hyperamylasemia as the only alteration. Acute complications of this pathology include hemorrhage, spontaneous rupture with peritonitis and cyst infection, and chronic complications include gastric or biliary outlet obstruction, portal venous or splenic thrombosis[3].
Indications for intervention include a persistent cyst for more than 6 weeks, larger than 6cm, significant symptoms, and the available options include endoscopic, open surgery or laparoscopic drenaige[4].
We present the case of a giant pseudocyst resolved by laparoscopic approach.
2. Case Report
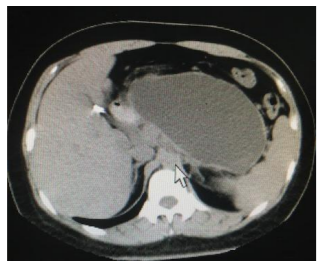
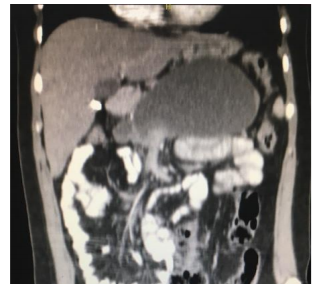
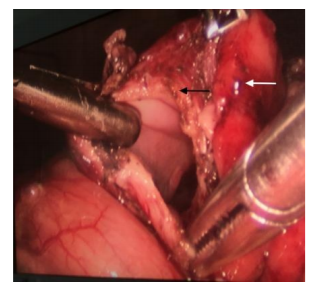
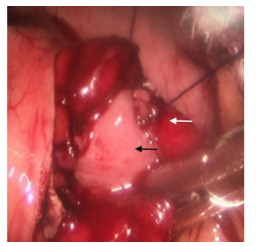
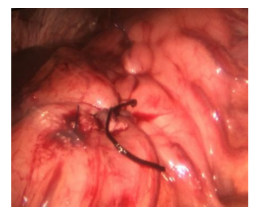
A female of 27 years-old came to general surgery consultation after having mild acute biliary pancreatitis three months ago and having a laparoscopic cholecystectomy after this. He complains of persistent abdominal pain of low intensity, with early postprandial fulfill and a decrease in weight for about 4 kilograms the last month. At physical exam with a BMI of 19kg/m2, all vital signs in normal parameters, without cardiothoracic alterations, plain abdomen with normal bowel sounds, in epigastrium a solid mass of about 10 centimeters could be perceived at deep palpation, with mild pain, it can’t be mobilized and was not compressible, with regular borders. The rest of physical exam was normal. By the background a pancreatic pseudocyst was suspected and a CT scan requested, which reported a collection in the front wall of the pancreas, with a thick wall (5mm) and heterogeneous content, predominantly hypo-echogenic, of 119x65x60 mm and a volume of 241 cc (Figure. 1-2). The open and laparoscopic approaches were offered to the patient and she decided to had a laparoscopic cystogastro anastomosis that were delayed two months to be completed by a surgeon with the appropriate training in advanced laparoscopic procedures. The cystogastro anastomosis was completed by a transgastric approach by a 6cm incision in the anterior gastric wall, with punction of posterior wall to confirm position of the cyst by draining a clear liquid, with opening of about 5 cm of the posterior gastric and anterior cyst wall and completing the anastomosis with prolene 00 running suture and closing anterior gastric wall with prolene 00 running suture. Total surgical time was 160 minutes, with bleeding of 30cc and without complications (Figure 3-5). After surgery patient underwent fasting for 3 days and at fourth day liquid diet was introduced, without any complications after this and diet progression. Patient was discharged at day 5 uneventfully and at 1 month follow up she stills asymptomatic.
3. Discussion
Pancreatic pseudocyst are complications of acute or chronic pancreatitis as mentioned before, being detected between 4-6 weeks after the acute onset in the first case.After diagnosis in 85% of cases it resolves in a period of 6 weeks. In cases without spontaneous resolution or persistent symptoms the drainage of the cyst is indicated because almost 33% could present complications like rupture, hemorrhage, infection or gastric outlet obstruction[5]. For this purpose, multiple endoscopic and surgical techniques have been developed along history. In the beginning the open approach to create a cystgastrostomy, cystduodenostomy and Roux-en-Y cystjejunostomy were the only options to treat this pathology. With the development of minimally invasive techniques, the drain of this collections by a catheter or stent during endoscopic procedures was widely applied but with a recurrence of 14.4% compared with 10% in open techniques and 2.5% in the laparoscopic group6. The advantage of endoscopic approach includes the low cost, feasibility in multiple medical centers, the short length of hospital stays and low rate of complications (12%) 4. Depending on location the drain by punction have being tried but with high rates of recurrence, for this reason there are no longer considered as an effective option. Laparoscopic techniques have been widely applied in some pathologies since their introduction, with a fast integration in the daily practice and being one of the preferred techniques actually, by the reduction in surgical time in many procedures, less bleeding, short length of hospital stay, less complications in some procedures, high rate of success, less pain, less fasting and faster recovery after surgery.
In the case of pancreatic pseudocyst, depending on the location, the laparoscopic approach would have excellent results with all the known benefits of laparoscopy including lower morbidity, rapid recovery and recurrence index comparable to open surgery. The surgical technique is basically the same as in the open approach, with the need of advanced laparoscopy skills by the surgeon. In the study of M. Aljabah et. al. comparing the effectiveness of laparoscopic vs endoscopic resolution the laparoscopic approach had better results with a success rate ranging from 95-98%, in comparison with endoscopic with a success rate of 80%, and the consequent needing for another option of drainage in the 15% of patients. The morbidity associated to laparoscopic approach is 4.2% and for the endoscopic approach 12%, with mortality of 0% and 4% respectively, recurrence of 2.5% for laparoscopy and 14.4% for endoscopy and re-intervention rates of 0.9% and 11.8% respectively[6]. In another study by Phillip S. et. al. the success rate for resolution in laparoscopic approach was 93.8% and 84.6% for endoscopic management, and 90.9% for open cystogastrostomy2. The reported results are similar than other actual studies with superiority of laparoscopic approach over open and endoscopic in success, morbidity, mortality and re-intervention rate[7].
By the previous mentioned reasons, the laparoscopic approach seems to be the election treatment option in case of pancreatic pseudocyst requiring drainage, and could be achieved by surgeons with advanced laparoscopy skills without the need of special instruments. In México the laparoscopy had been introduced many years ago and more procedures are being reproduced each day. In the Crisanto Campos et. al. report of laparoscopic cystogastrostomy for pancreatic pseudocyst treatment, developed from 2012 to 2014 and including 17 patients, they have similar success rate and complications associated with this approach[7]. In the Mexican Institute of Social Security, we have not found a previous report of this approach as the preferred, only a retrospective study of open technique results including 139 patients from 2000 to 2013, and only 1 was resolved by laparoscopy in the XXI Century National Medical Center, a low rate considering that it is one of the biggest hospitals in México[8].
4. Conclusion
In conclusion the laparoscopic cystogastrostomy have been confirmed to be a safe and effective method to resolve pancreatic pseudocyst, with superior results over other techniques, and could be developed by surgeons with advanced laparoscopic skills.
References
- Asri Che Jusoh , Jasni Hassan , Ruzaimie Mohd Nor, Kong Chee Fong, et. al. Combined Laparoscopic Cholecystectomy And Drainage Of Pancreatic Pseudocyst: A Case Report And Review Of Current Management. . Med J Malaysia 2013; 68 (3): 273-274.
- Phillip S. Ge, Mikhayla Weizmann, Rabindra R. Watson. Pancreatic Pseudocysts Advances in Endoscopic Management. Gastroenterol Clin N Am 45 (2016) 9–27
- Alaa A. Redwan, Mostafa A. Hamad,and Mohammed A. Omar. Pancreatic Pseudocyst Dilemma: Cumulative Multicenter Experience in Management Using Endoscopy, Laparoscopy, and Open Surgery. JOURNAL OF LAPAROENDOSCOPIC & ADVANCED SURGICAL TECHNIQUES Volume 00, Number 00, 2017. DOI:10.1089/lap.2017.0006.
- Yazan S. Khaled, Deep J. Malde, Jessica Packer, Thomas Fox, et. al. Laparoscopic versus open cystgastrostomy for pancreatic pseudocysts: a case-matched comparative study. J Hepatobiliary Pancreat Sci (2014) 21:818–823.
- Daniel F. Saad, Kenneth W. Gow, Samer Cabbabe, Kurt F. Heiss, Mark L. Wulkan. Laparoscopic cystogastrostomy for the treatment of pancreatic pseudocysts in children. Journal of Pediatric Surgery (2005) 40, E13– E17.
- M. Aljarabah, B. J. Ammori. Laparoscopic and endoscopic approaches for drainage of pancreatic pseudocysts: a systematic review of published series. Surg Endosc (2007) 21:1936– 1944 DOI 10.1007/s00464-007-9515-2.
- Guardado-Bermúdez F, Azuara-Turrubiates AJ, Ardisson-Zamora FJ, Guerrero-Silva LA. Pancreatic pseudocyst. Case report and literature review. Cir Cir. 2014 Jul-Aug;82(4):425-31.
- José Luis Martínez-Ordaz∗, Carlos Toledo-Toral, Norma Franco-Guerrero,et. al. Surgical treatment of pancreatic pseudocysts. Cirugía y Cirujanos. 2016;84(4):288-292