Information
Journal Policies
Epidural Hematoma in Handball - The importance of Surveillance
Joao L. Pascoa Pinheiro1, Marcos Barbosa1,3, Joao Pascoa Pinheiro2,3*, Armando Rocha1, Maria Joao Frade1
2.Centro Hospitalar Universitário de Coimbra, Physical Medicine and Rehabilitation Department, Coimbra, Portugal
3.Faculty of Medicine, University of Coimbra, Coimbra, Portugal
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Traumatic brain injury is a silent epidemic entity with a great impact in nowadays economy and society. Currently, it is the leading cause of mortality and disability among young people in developed countries. In sports, epidural hematomas are rare. Early surgical treatment is usually associated with good outcomes. So, early diagnosis of these silent entities is important to prevent irreversible neurological deficits. This case report highlights the importance of surveillance of the athlete who suffers a TBI during sports practice.
Epidural Hematoma, Traumatic Brain Injury, Sports Injuries, Intracranial Hypertension ,Research in Sports Medicine
1. Introduction
According to various centres it is estimated that between 1.6 and 3.8 million cases of sports-related traumatic brain injury (TBI) occur annually. The most common head injury is concussion, a diffuse lesion caused by acceleration-deceleration mechanisms[1].In sports, epidural hematomas (EDH) are a rare entity. In the literature, ED Hare usually associated with motor sports, horse riding and contact sports such as rugby, American football, ice hockey, lacrosse or boxing. Severe TBI and focal head injuries have a low incidence in handball practice[2]. Early surgical evacuation of EDH is usually related to good functional outcomes. If no other underlying brain injury is present, 50% of patients have a Glasgow Outcome Scale (GOS) of 5, 15 days after surgical drainage. However, the athlete must be strongly advised to give up the practice of all contact sports[3].
We report a case of a handball player who developed an EDH after a head injury during a handball match. The lack of surveillance after the traumatic event and the time to surgery may explain the poor outcome.
2. Case Report
A 23-year-old handball player received a blow from an elbow to the right temporo-parietal region during a match. He fell to the ground complaining of dizziness and a light headache.
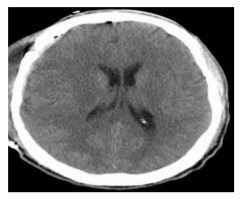
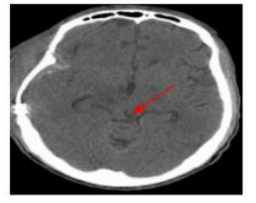
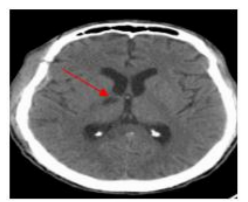
No loss of consciousness or focal neurological deficits was reported. The athlete remained on the field until the final whistle. In the dressing room he referred to a low-intensity non-localized headache. Three hours after the TBI, he began to experience confusion and nausea. Two hours later, he was found lying on the ground unconscious, without reactivity to auditory or painful stimuli. He was transported by ambulance to the emergency room of the nearest hospital, where a Glasgow Coma Scale (GCS) of 6 (E1M4V1), anisocoric pupils and bilateral withdrawal from pain were reported. A Cranial Computed Tomography (CT) scan performed in the emergency showed a fracture of the temporal bone and a large right fronto-temporo-parietal EDH, with great mass effect, midline shift, uncal herniation and signs of active bleeding (Figure1). The athlete was immediately transferred to the neurosurgery department of our institution for urgent surgical intervention, which was carried outwithout complications. He stayed in the Intensive Care Unit (ICU) with Intracranial Pressure (ICP) monitoring and was transferred to the neurosurgical ward on the tenth day after surgery. No residual bleeding or hematoma was described on the control cranial CT scan (Figure2). On the tenth postoperative day, multiple ischemic lesions in the mesencephalon and thalamus were recorded in imaging controls (Figure3) (Figure4) and the GOS after discharge from the ICU was 2. He was transferred to a rehabilitation department, 2 months after surgery. Recently, at the 12-month follow-up, no improvement in neurological status was observed.
3. Discussion
Ankle and knee sprains are the most common acute injuries in handball practice. Hamstrings and gastrocnemius strains, nose and fingers fractures and shoulder anterior dislocation are also frequent lesions. In fact, thoracic and cranial trauma have a low incidence and prevalence[4].The Advanced Trauma Life Support (ATLS) guidelines suggest a CT scan after TBI in a patient with a GCS of 15, if there is loss of consciousness, headache or dizziness associated[5].
EDHs are focal haemorrhagic lesions located between the inner table of the skull and the dura mater. More than 85% of EDH are associated with a fracture of the temporal bone and rupture of the middle meningeal artery. The anterior branch is the most affected, since its path includes the pterion, a region in the temporal fossa, where the frontal bone, parietal bone, squamous part of the temporal bone and great wing of the sphenoid articulate[6].
Clinical features of HED were first described by Jacobson in 1886. There is initially a period of lucidity which corresponds to the accumulation of blood in the epidural space. No symptoms or neurological deficit are observed. In minutes or hours, a progressive deterioration of mental status, hemi paresis and oculomotor nerve palsy could occur. The blood between the bone and the dura starts to compress the brainstem and its structures such as the reticular formation, cerebral peduncles and the oculomotor nerve. In later stages, transtentorial followed by tonsillar herniation promote dysfunction of respiratory and cardiac centres with possible death[7].
According to the Monroe-Kelly doctrine, intracranial volume is the sum of cerebrospinal (CSF), blood and parenchymal volumes. An additional component inside the cranial vault leads to an increase in the ICP. The first physiological compensation is a reduction in CSF volume, followed by a decrease in the cerebral blood flow (CBF). CBF reduction is also related to aberrant cerebral pressure auto regulation, a consequence of the traumatic event[8].
In this case the poor outcome may be explained by several factors. The period of time between the onset of the compressive phenomenon and cerebral decompression was too long. Thus, high ICP values promote a CBF decrement over a long period of time. Cerebral anoxia may also account for the ischemic lesions observed, since the athlete was found unconscious with a GCS of less than 8 and without protection of the airway.
4. Conclusion
This case report emphasizes the importance of promoting a thorough neurological examination following TBI in any sport. After a correct primary survey based on ATLS guidelines, side-line neuropsychological exams such as the Sports Concussion Assessment Tool version 5 (SCAT5) or the Standardized Assessment of Concussion (SAC) should be performed.9The athlete should under no circumstances return to the match.
Sports Medicine physicians need to be more aware of these silent entities capable of triggering serious consequences. We believe that a rigorous plan of surveillance lasting at least 24 hours should be implemented for athletes who are victims of TBI during a competition.
This should include regular observation by their relatives and one medical doctor. Any symptom suggesting the presence of an intracranial haemorrhagic lesion in the brain, is reason enough to immediately take the athlete to the nearest hospital for a CT Scan. Early identification of an EDH could saves the athlete’s life or avoid severe neurological disability.
References
- Hobbs JG, Young JS, Bailes JE. Sports-related concussions: diagnosis, complications, and current management strategies. Neurosurg Focus. 2016;40(4):E5.
- Zemper ED. Catastrophic injuries among young athletes. Br J Sports Med. 2010; 44(1):13-20.
- Bullock MR, Chesnut RM, Ghajar JB. Surgical Management of TBI. Neurosurgery. 2006; 5(2):342-349.
- Dirx M, Bouter LM. Aetiologyofhandball in juries : a case-controlstudy. Br J Sports Med. 1992;26(3):3-6.
- ATLS Subcommittee, American College of Surgeons’ Committeeon Trauma, International ATLS workinggroup. Advanced trauma lifesupport (ATLS®): then in the edition. J Trauma Acute Care Surg. 2013;74(5):1363-1366.
- Morris SA, Jones WH, Proctor MR, Day AL. Emergent treatment of athletes with brain injury. Neurosurgery. 2014; 75:S96-S102.
- Miele VJ, Norwig JA, Bailes JE. Sideline and ringside evaluation for brain and spinal injuries. Neurosurg Focus. 2006;21(4):E8.
- Stein DM, Hu PF, Brenner M, et al. Brief episodes of intracranial hypertension and cerebral hypoperfusion are associated with poor functional outcome after severe traumatic brain injury. J Trauma. 2011; 71(2):364-374.
- McCrory P, Meeuwisse W, Dvořák J, et al. Consensus statement on concussion in sport— the 5thinternational conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017; 51(11):838-847.