Information
Journal Policies
Talus fractures in children
N. K. Sferopoulos
Copyright :© 2017 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Pediatric talus fractures are very rare in childhood. The talar neck is the most common fracture site, followed by the talar body. The mechanism of injury is usually an axial load on a dorsiflexed foot. They are classified in two age groups. In group I, involving children younger than 6 years, fractures are usually undisplaced and the diagnosis may be easily missed. In group II, involving children older than 6 years, fractures are usually due to high-energy injuries, the incidence of complications is higher and osteochondral fractures may also be encountered. The Hawkins classification may be used to describe the different types of fractures of the talar neck and to predict the risk of avascular necrosis. Undisplaced injuries may be managed non-operatively with cast immobilization. Displaced injuries may be treated with either closed or open reduction. Internal fixation is recommended for any instability following reduction. The most significant complications of talus fractures are avascular necrosis and post-traumatic malalignment, which may be followed by early osteoarthritic changes.
Talus fractures,children,Research in Sports Medicine
Editorial
The rare incidence of pediatric talus fractures in the literature has precluded large epidemiologic studies referring to outcomes and rates of complications. The most common fracture location in children is the talar neck. The skeletally immature bone, in younger children, is less brittle and provides higher elastic resistance to torsional forces than in older children and adults. The most common mechanism of injury in talus fractures is forceful dorsiflexion resulting in talar neck fracture as it impinges against the anterior tibia. Inversion injuries may result in osteochondral fractures of the superior talar dome, due to impingement of the talus against the medial malleolus, while plantar flexion forces may displace os trigonum segments or fracture the posterior talar dome.
Talus fractures encompass fractures of the neck, of the body, such as transchondral dome fractures, lateral process or posterior tubercle fractures, shear or crush fractures, and bone bruises.
History and clinical examination in children may be challenging. The clinical symptoms and signs usually include pain and swelling to the anterior aspect of the ankle associated with inability to bear weight on the affected extremity. In undisplaced injuries, the presentation may be subtle and the injury may be easily missed. With high-energy trauma, such as falls from height and traffic road accidents, a large degree of soft tissue damage and clinical deformity is often evident, while concomitant fractures elsewhere in the foot or about the ankle may also be encountered.
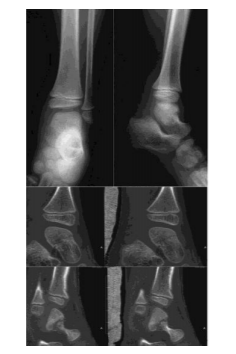
Plain radiographs may not necessarily demonstrate a fracture or an osteochondral defect. Advanced imaging is often necessary to better characterize the fracture pattern or extent of injury. When no fracture is visualized on plain films and suspicion is high, based on the clinical examination, computed tomography (CT) or magnetic resonance imaging (MRI) is useful to identify an undisplaced or minimally displaced fracture (Figure.1).
In the case of a comminuted fracture, CT may better delineate the fracture fragments, the degree of displacement and assist in determining the need for operative intervention. The edema pattern seen on MRI may also be helpful to delineate an occult fracture. The Hawkins sign, appearing 6-8 weeks post-injury, as radiolucency in the subchondral area of the talar body indicates a good blood supply and that the talus is likely to remain viable.
Talar fractures in children may be classified in type I-IV fracture patterns correlating with the severity of injury and the risk of avascular necrosis using the Hawkins classification, modified by Canale and Kelly that is used in adults.
A classification, including two groups of patients, depending on the age of the injured child has also been proposed. In children younger than 6 years the diagnosis is easily missed because the fracture may not be clearly delineated on radiographs. In children older than 6 years osteochondral fractures, complete fractures and avascular necrosis are more commonly encountered.
It is important to note that talus fractures may also be associated with other concomitant fractures. Even in the setting of an obvious talus fracture, radiographs must be scrutinized to rule out additional injuries. Talar neck fractures have been described in association with compression injuries of the calcaneocuboid joint, as well as with fractures of the distal tibia.
The majority of pediatric talus fractures is undisplaced and is managed with non-weight bearing in a long leg cast for 6 to 8 weeks. In displaced fractures the principals of joint fractures should be followed to achieve an early anatomical reconstruction. Following reduction, whenever stability is questionable fixation is indicated. The approach is based on the fracture pattern and the need for both open reduction and fixation versus closed reduction and fixation. Reduction of talar neck fractures may be performed through a dorsomedial approach and fixation placed through a posterior approach.
Tourniquet application may be a further negative factor for blood supply and may contribute to subsequent osteonecrosis. Due to the concern for the development of avascular necrosis, patients must be followed with serial radiographs. Nondisplaced fractures should be followed for at least 18 months and more severe fracture patterns should be followed well beyond this timeline.
Avascular necrosis of the talus may complicate fractures and dislocations. It usually develops between several weeks to 6 months after injury. Talar avascular necrosis may lead to significant disability and post-traumatic arthritis. The incidence of avascular necrosis in children with undisplaced talus fractures may be up to 16%, which is considerably higher than the reported in adults. However, this reported incidence could be due to initially missed and therefore non-treated fractures. Other complications associated with talus fractures include non-union, malunion, loose bodies, infection, neuropraxia and wound healing issues [1-43].
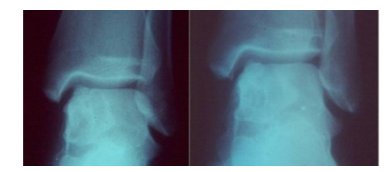
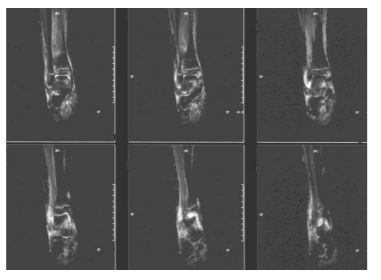
Transchondral, osteochondral, talar dome or flake fracture and osteochondritis/ osteochondrosis dissecans are all terms used to describe similar lesions of the talus (Figure.2, 3).
Their cause is controversial, since some patients have unilateral or bilateral lesions with chronic ankle pain but no history of trauma, while others (the majority) are diagnosed following trauma. The two groups are often radiographically indistinguishable. Traumatic, ischemic or micro-traumatic necrosis, abnormal patterns of vasculature, congenital factors, and spontaneous necrosis have all been proposed as etiological theories. Conservative treatment remains the mainstay of treatment of traumatic osteochondral defect in children. Surgical treatment is mandatory in unstable cartilage fragments. The lesion may be complicated by secondary osteoarthritis [44-49].
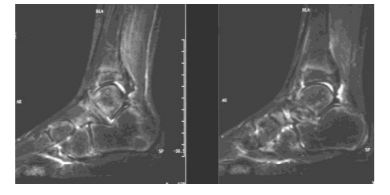
Finally, children with significant residual clinical symptoms and signs 6 weeks after an ankle injury, with no radiographic findings, should undergo a limited MRI to detect bone contusions or flake fractures (Figure.4, 5, 6).
In bone bruises, an elongated immobilisation and recovery period is required for the complete resolution of the clinical symptoms and signs. It has been shown that bone bruising represents a distinct clinical entity with ‘benign’ characteristics, since no long-term morbidity has been reported in any of the presented patients [60-64].
References
- McKeever F. Fracture of the neck of the astragalus. Arch Surg. 1943; 46: 720-735.
- Stephens NA. Fracture-dislocation of the talus in childhood; a report of two cases. Br J Surg. 1956; 43(182): 600- 604. PMID: 13342422.
- Hawkins LG. Fractures of the neck of the talus. J Bone Joint Surg Am. 1970; 52(5): 991-1002. PMID: 5479485.
- Sneppen O, Christensen SB, Krogsoe O, Lorentzen J. Fracture of the body of the talus. Acta Orthop Scand. 1977; 48(3): 317-324. PMID: 920125.
- Canale ST, Kelly FB. Fractures of the neck of the talus. Long-term evaluation of seventy-one cases. J Bone Joint Surg Am. 1978; 60(2): 143-156. PMID: 417084.
- Letts RM, Gibeault D. Fractures of the neck of the talus in children. Foot Ankle. 1980; 1(2): 74-77. PMID: 7274901.
- Mazel C, Rigault P, Padovani JP, Finidori G, Touzet P. Fractures of the talus in children. Apropos of 23 cases. Revchir Orthop Reparatrice Appar Mot. 1986; 72(3):183-95. PMID: 3749552.
- Stutz JM, Karlin JM, Daly N. Fracture-dislocation of the talus in the pediatric patient. An unusual injury. J Am Podiatr Med Assoc. 1991; 81(9): 495- 498. PMID: 1748966. DOI: 10.7547/87507315-81-9-495.\
- Jensen I, Wester JU, Rasmussen F, Lindequist S, Schantz K. Prognosis of fracture of the talus in children. 21 (7-34)-year follow-up of 14 cases. Acta Orthop Scand. 1994; 65(4): 398- 400. PMID: 7976283.
- Draijer F, Havemann D, Bielstein D. Injury analysis of pediatric talus fractures. Unfallchirurg. 1995; 98(3):130-132. PMID: 7754399.
- Pereles TR, Koval KJ, Feldman DS. Fracture- dislocation of the neck of the talus in a ten- year-old child: a case report and review of the literature. Bull Hosp Jt Dis. 1996; 55(2): 88-91. PMID: 8879745.
- Talkhani IS, Reidy D, Fogarty EE, Dowling FE, Moore DP. Avascular necrosis of the talus after a minimally displaced neck of talus fracture in a 6 year old child. Injury. 2000; 31(1): 63-65. PMID: 10716054.
- Rammelt S, Zwipp H, Gavlik JM. Avascular necrosis after minimally displaced talus fracture in a child. Foot ankle Int. 2000; 21(12): 1030-1036. PMID: 11139033.
- Leibner ED, Simanovsky N, Abu-Sneinah K, Nyska M, Porat S. Fractures of the lateral process of the talus in children. J Pediatr Orthop B. 2001; 10(1): 68-72. PMID: 11269815.
- Paterson JM. Children's fractures 'not to be missed'. Hosp Med. 2002; 63(7): 426-428. PMID: 12187604.
- Judd DB, Kim DH. Foot fractures frequently misdiagnosed as ankle sprains. Am Fam Physician. 2002; 66(5):785-794. PMID: 12322769.
- Nenopoulos SP, Papavasiliou VA, Papavasiliou A V. Talus fracture associated with a fracture dislocation of the distal tibia in an immature skeleton. Acta Orthop Belg. 2003; 69(5): 473-475. PMID: 14648961.
- Prasad KSRK. Avascular necrosis of the talus after a minimally displaced neck of talus fracture in a 6-year-old child [Injury 31 (2000) 63-65]. Is it really unique? Injury. 2004; 35(11): 1216-1217. PMID: 15488523. DOI: 10.1016/j.injury.2004.02.016.
- Ribbans WJ, Natarajan R, Alavala S. Pediatric foot fractures. Clin Orthop Relat Res. 2005; 432: 107-115. PMID: 15738810.
- Meier R, Krettek C, Griensven M, Chawda M, Thermann H. Fractures of the talus in the pediatric patient. Foot Ankle Surg. 2005; 11: 5– 10. DOI:10.1016/j.fas.2004.10.001.
- Polyzois VD, Vasiliadis E, Zgonis T, Ayazi A, Gkiokas A, Beris AE. Pediatric fractures of the foot and ankle. Clin Podiatr Med Surg. 2006; 23(2): 241-55, v. PMID: 16903152.
- Gehr J, Friedl W. Fracture of the neck of the talus in a child. Unfallchirurg. 2006; 109(10): 910913.PMID:16944078.DOI:10.1007/s00113-006-1128-z.
- Cartwright-Terry M, Pullen H. Non- operative management of a talar body fracture in a skeletally immature patient. Acta Orthop Belg. 2008; 74(1): 137-140. PMID: 18411617.
- Memisoglu K, Hürmeydan A. Total extrusion of the talus in an adolescent: a case report. J Am Podiatr Med Assoc. 2009; 99(5): 431-434. PMID: 19767550.
- Eberl R, Singer G, Schalamon J, Hausbrandt P, Hoellwarth ME. Fractures of the talus-differences between children and adolescents. J Trauma. 2010; 68(1): 126-130. PMID: 20065767.DOI:10.1097/TA.0b013e3181a74667.
- Yazdi H, Ramezan Shirazi M. An unusual presentation of talus fracture in a child: a case report. Foot Ankle Surg. 2010; 16(3): e57-e60. PMID:20655001.DOI:10.1016/j.fas.2010.03.00 5.
- Smith JT, Curtis TA, Spencer S, Kasser JR, Mahan ST. Complications of talus fractures in children. J Pediatr Orthop. 2010; 30(8): 779-784. PMID: 21102201. DOI: 10.1097/BPO.0b013e3181f73e6e.
- Byrne AM, Stephens M. Paediatric talus fracture. BMJ Case Rep. 2012; 2012. pii: bcr1020115028. PMID: 22605852. PMCID: PMC3351635. DOI: 10.1136/bcr.10.2011.5028.
- Godoy-Santos AL, Albuquerque DM, Diniz-Fernandes T, Rammelt S. Fracture of the talar neck associated with a compression fracture of the calcaneocuboid joint in a 5-year-old child: a case report. Arch Orthop Trauma Surg. 2013; 133(9): 1267-1271. PMID: 23784318. DOI: 10.1007/s00402-013-1791-9.
- Prasad KSRK, Vali H, Hussain A. Hawkins Group I fracture of neck of talus and Salter Harris Type III tibial epiphyseal injury of medial malleolus. Foot (Edinb). 2013; 23(2-3): 96-99. PMID: 23639364. DOI: 10.1016/j.foot.2013.03.002.
- Jindal N, Gupta P, Jindal S. Nonunion of paediatric talar neck fracture. Chin J Traumatol. 2014; 17(1): 48-49. PMID: 24506925.
- Patel V, Bloch B, Johnson N, Mangwani J. Delayed presentation of a loose body in undisplaced paediatric talar neck fracture. World J Orthop. 2014; 5(3): 398-401. PMID: 25035846. PMCID: PMC4095036. DOI: 10.5312/wjo.v5.i3.398.
- Inal S, Inal C. A pediatric comminuted talar fracture treated by minimal K-wire fixation without using a tourniquet. Iowa Orthop J. 2014; 34: 175-180. PMID: 25328479. PMCID: PMC4127733.
- Crosswell S, Rhee SJ, Wagner WW. Unusual fracture combination in a paediatric acute ankle (combined medial talar compression fracture with medial malleolus fracture in an immature skeleton): a case report. J Surg Case Rep. 2014; 10. pii: rju100. PMID: 25320236. PMCID: PMC4197413. DOI: 10.1093/jscr/rju100.
- Kamphuis SJ, Meijs CM, Kleinveld S, Diekerhof CH, van der Heijden FH. Talar fractures in children: A possible injury after go- karting accidents. J Foot Ankle Surg. 2015; 54(6): 1206-1212. PMID: 26364700. DOI: 10.1053/j.jfas.2015.07.013.
- Melenevsky Y, Mackey RA, Abrahams RB, Thomson NB 3rd. Talar Fractures and Dislocations: A radiologist's guide to timely diagnosis and classification. Radiographics. 2015; 35(3): 765-779. PMID: 25969933. DOI: 10.1148/rg.2015140156.
- Wu Y, Jiang H, Wang B, Miao W. Fracture of the lateral process of the talus in children: A kind of ankle injury with frequently missed diagnosis. J Pediatr Orthop. 2016; 36(3): 289-293.PMID:25785595.DOI:10.1097/BPO.00000 00000000437.
- Rammelt S, Godoy-Santos AL, Schneiders W, Fitze G, Zwipp H. Foot and ankle fractures during childhood: review of the literature and scientific evidence for appropriate treatment. Rev Bras Ortop. 2016; 51(6): 630639. PMID: 28050532.PMCID: PMC5198067.DOI: 10.1016/j.r boe.2016.09.00.
- Michel-Traverso A, Ngo TH, Bruyere C, Saglini M. Talus fracture in a 4-year-old child. BMJ Case Rep. 2017; 2017. pii: bcr- 2016-215063. PMID: 28400423. PMCID: PMC5534889. DOI: 10.1136/bcr-2016-215063.
- Kothadia S, Birole U, Ranade A. Paediatric Salter-Harris type IV injury of distal tibia with talus fracture. BMJ Case Rep. 2017; 2017. pii: bcr-2017-222226. PMID: 29183896. DOI: 10.1136/bcr-2017-222226.
- Kızılay YO, Aytan O. Low-Energy Hawkins Type III Talar neck fracture-dislocation with neurovascular and tendon entrapment in a pediatric patient. J Foot Ankle Surg. 2017; 56(6): 1288-1291. PMID: 28778631. DOI: 10.1053/j.jfas.2017.05.007.
- Hood CR Jr, Miller JR, Hollinger JK. Defining talar head and neck pathology: The Malvern classification system. J Foot Ankle Surg. 2017; pii: S1067-2516(17)30455-6. PMID: 28843549. DOI: 10.1053/j.jfas.2017.07.008.
- Talus Fractures. https://posna.org/Physician-Education/Study-Guide/Talus-Fractures
- Pettine KA, Morrey BF. Osteochondral fractures of the talus. A long-term follow-up. J Bone Joint Surg Br. 1987; 69(1): 89-92. PMID: 3818742.
- Anderson IF, Crichton KJ, Grattan-Smith T, Cooper RA, Brazier D. Osteochondral fractures of the dome of the talus. J Bone Joint Surg Am. 1989; 71(8): 1143-1152. PMID: 2777840.
- Wester JU, Jensen IE, Rasmussen F, Lindequist S, Schantz K. Osteochondral lesions of the talar dome in children.A 24(736) year follow-up of 13 cases. Acta Orthop Scand. 1994; 65(1): 110-112. PMID: 8154273.
- Higuera J, Laguna R, Peral M, Aranda E, Soleto J. Osteochondritis dissecans of the talus during childhood and adolescence. J Pediatr Orthop. 1998; 18(3): 328-332. PMID: 9600558.
- Stroud CC, Marks RM. Imaging of osteochondral lesions of the talus. Foot Ankle Clin. 2000; 5(1): 119-133. PMID: 11232076.
- Letts M, Davidson D, Ahmer A. Osteochondritis dissecans of the talus in children. J Pediatr Orthop. 2003; 23(5): 617-625. PMID: 12960624.
- Schachter AK, Chen AL, Reddy PD, Tejwani NC. Osteochondral lesions of the talus. J Am Acad Orthop Surg. 2005; 13(3): 152-158. PMID: 15938604.
- Perumal V, Wall E, Babekir N. Juvenile osteochondritis dissecans of the talus. J Pediatr Orthop. 2007; 27(7): 821-825. PMID: 17878792.DOI:10.1097/BPO.0b013e3181558961.
- Merian M, Easley M. Diagnosis and treatment of osteochondral lesions of the talus. Orthopade. 2008; 37(3): 204, 206-11. PMID: 18324387. DOI: 10.1007/s00132-008-1219-3.
- van Bergen CJ, de Leeuw PA, van Dijk CN. Treatment of osteochondral defects of the talus. Rev Chir Orthop Reparatrice Appar Mot. 2008; 94(8 Suppl): 398-408. PMID: 19046699. DOI: 10.1016/j.rco.2008.09.003.
- Thacker MM, Dabney KW, Mackenzie WG. Osteochondritis dissecans of the talar head: natural history and review of literature. J Pediatr Orthop B. 2012; 21(4):373-376. PMID: 22673051.DOI:10.1097/BPB.0b013e328346c0 76.
- Hannon CP, Smyth NA, Murawski CD, Savage-Elliott I, Deyer TW, Calder JD, Kennedy JG. Osteochondral lesions of the talus: aspects of current management. Bone Joint J. 2014; 96B (2): 164-171. PMID: 24493179. DOI: 10.1302/0301-620X.96B2.31637.
- Zanon G, DI Vico G, Marullo M. Osteochondritis dissecans of the talus. Joints. 2014; 2(3): 115-123. PMID: 25606554. PMCID: PMC4295677.
- Heyse TJ, Schüttler KF, Schweitzer A, Timmesfeld N, Efe T, Paletta JR, Fuchs-Winkelmann S, Fernandez FF. Juvenile osteochondritis dissecans of the talus: predictors of conservative treatment failure. Arch Orthop Trauma Surg. 2015; 135(10): 1337-1341.PMID:26267077.DOI: 10.1007/s00402-015-2260-4.
- Gorbachova T, Wang PS, Hu B, Horrow JC. Plantar talar head contusions and osteochondral fractures: associated findings on ankle MRI and proposed mechanism of injury. Skeletal Radiol. 2016; 45(6): 795-803. PMID: 26969200. DOI: 10.1007/s00256-016-2358-y.
- Looze CA, Capo J, Ryan MK, Begly JP, Chapman C, Swanson D, Singh BC, Strauss EJ. Evaluation and management of osteochondral lesions of the talus. Cartilage. 2017; 8(1): 19-30. PMID: 27994717.PMCID:PMC5154424.DOI:10.1177/19 47603516670708.
- Endele D, Jung C, Bauer G, Mauch F. Value of MRI in diagnosing injuries after ankle sprains in children. Foot Ankle Int. 2012; 33(12): 1063-1068.PMID:23199854.DOI:10.3113/FAI.2012. 1063.
- Sferopoulos NK. Residual symptoms of occult pediatric ankle injuries: MRI-diagnosed bone bruising. British Journal of Medicine & Medical Research 2014; 4(1): 295-303. DOI: 10.9734/BJMMR/2014/5607.
- Gill PJ, Klassen T. Revisiting radiograph-negative ankle injuries in children: Is it a fracture or a sprain? JAMA Pediatr. 2016; 170(1): e154147. PMID: 26747078. DOI: 10.1001/jamapediatrics.2015.4147.
- Boutis K, Plint A, Stimec J, Miller E, Babyn P, Schuh S, Brison R, Lawton L, Narayanan UG. Radiograph-negative lateral ankle injuries in children: Occult growth plate fracture or sprain? MA Pediatr. 2016; 170(1): e154114. PMID:26747077.DOI:10.1001/jamapediatrics.2 015.4114.
- Sferopoulos NK. The classification of physeal injuries. ARC Journal of Orthopedics 2016;1(1):237.DOI: http://dx.doi.org/10.20431/ 2456-0588.0101005