Information
Journal Policies
A Mesenteric Fibromatosis Presenting with Small Bowel Perforation
Ji-Eun Kim1,Jung-Hee Yoon1*,Seung-Ho Kim1,Yedaun Lee1
Copyright :© 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background: A small bowel mesenteric fibromatosis is a type of intra-abdominal desmoid tumor, which is a rare fibroblastic proliferative disease and benign intraabdominal tumor. A mesenteric fibromatosis is usually asymptomatic. However, it may lead to various complications, including bowel obstruction.
Case Report: Here, we report a case of a mesenteric fibromatosis with the uncommon presentation of small bowel perforation and peritonitis. A 25-year-old man presented with a 4-day history of abdominal pain. Computed tomography imaging of the abdomen and pelvis revealed a large, heterogeneously enhancing soft tissue mass abutting the distal ileal loop in the pelvic cavity as well as evidence of diffuse peritonitis with free air. The patient was surgically diagnosed with a mesenteric fibromatosis with small bowel perforation.
Why Should an Emergency Physician be Aware of this?: To our knowledge, there are few case reports published in English concerning the radiologic features of mesenteric fibromatosis presenting with bowel perforation, a surgical emergency that may be confused with gastrointestinal stromal tumor or lymphoma. CT imaging played a significant role in the diagnosis and management of this potentially lethal condition.
Abdomen; mesenteric fibromatosis; small bowel perforation; computed tomography, diagnosis,Radiology and Medical Imaging
1. Introduction
A desmoid tumor is a benign fibrous neoplasm arising from musculo-aponeurotic structures over the body. They commonly occur in post-partum women, in whom they may originate from the rectus muscle and old surgical incisions. [1] A mesenteric fibromatosis (MF), also called an intraabdominal desmoid, is a rare benign fibroblastic tumor which accounts for approximately 0.03% of all neoplasms and 8% of all desmoid tumors.[2]Most cases of MF occur in the small bowel mesentery. [3] These tumors are usually asymptomatic, although they may have variable complications. We report a rare case which has the uncommon presentation of a MF presenting as small bowel perforation with peritonitis.
2. Case Report
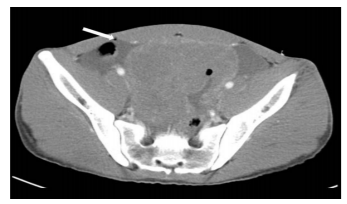
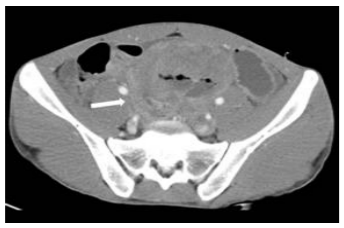
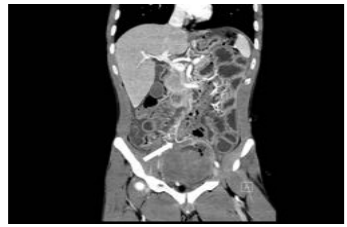
A 25-year-old man presented to our hospital emergency room with the chief complaint of abdominal pain starting 4 days earlier. He had no underlying disease or history of surgery. On physical examination, his abdomen was rigid without bowel sounds on auscultation. Additionally, there was tenderness and rebound tenderness throughout his abdomen suggestive of a surgical abdomen. Among laboratory findings, the C-reactive protein level was high (9.53 mg/dl). Abdomino-pelvic computed tomography (CT) with contrast enhancement was performed that day in our emergency room to evaluate the cause of abdominal pain. The pre-contrast CT scan revealed a well-defined large mass which contained an internal irregularly shaped cavity located within the pelvis (not shown). This mass measured 11 cm at its largest diameter and was visualized as a low-density mass without hemorrhage or calcifications. On contrast-enhanced CT images, the mass was visible as a heterogeneous mild enhancement. Additionally, there was a small amount of free air in the abdominal cavity suggestive of pneumoperitoneum, as well as a moderate amount of ascites in the abdominopelvic cavity with mild enhancement of the peritoneum (Figure 1A). This mass appeared to abut the distal ileal loop at a higher level without definite obstruction of the lumen (Figure 1B, 1C) or vascular supply, which arose from engorged ileocolic vessels (Figure 1D). There were no other definite visible wall defects throughout the entire bowel loop. We found no other abnormal findings except for multiple enlarged lymph nodes in the retroperitoneum. Under the diagnostic impression of a perforated small bowel gastrointestinal stromal tumor (GIST) or a small bowel lymphoma with panperitonitis, the patient underwent diagnostic exploratory laparotomy which evolved to a right hemicolectomy including the terminal ileum, cecum, and appendix. Surgical exploration revealed a large mesenteric mass arising from the mesentery on the surgical bed. The tumor was excised together with a segment of terminal ileum. Grossly, the tumor appeared as a solid mass measuring 14 x 11 x 9 cm abutting the terminal ileum (Figure 1E) with associated serositis and perforation. The cut surface of the mass was grayish and solid, and appeared congested.
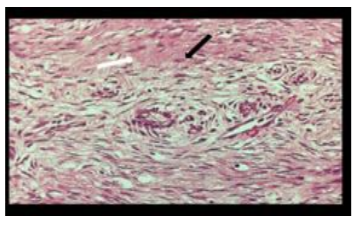
Additionally, turbid contaminated fluid was found in the abdominal cavity. No other perforation site in the gastrointestinal tract was found. Microscopic evaluation (F) revealed that the tumor was composed of collagen surrounding proliferative bland spindle cells, with mild increased cellularity, a 1/10 HPF mitotic count, and no necrosis. Immunohistochemistry staining revealed tumor cells, all of which were negative for SMA, beta catenin, desmin, S100, C-kit and CD-34. Although CD34 and C-kit were negative, this tumor was suggestive of a MF, a benign fibroblastic proliferation causing adjacent terminal ileal perforation.
3. Discussion
Desmoids can present in peripheral or intra-abdominal forms. An intra-abdominal desmoid, also known as a MF, is the least common type of fibromatosis. A MF, a rare benign fibroblastic tumor, is the most common solid primary neoplasm of the mesentery[1].
The exact etiology of MF is uncertain. However, hormonal factors may be associated, as estrogen receptors are present in some desmoid tumors. They occur in young women during and after pregnancy, and begin to regress during menopause as well as with tamoxifen and even oral contraceptive therapy.[1] Approximately 13% of patients with MF have familial adenomatous polyposis (FAP), specifically the Gardner syndrome variant of FAP.[3] Trauma has been proposed as another causative factor, although there was no specific history in our patient.
A MF is usually asymptomatic until its growth and infiltration causes compression of the viscera.[1] This can lead to gastrointestinal bleeding, ischemic bowel disease secondary to vascular compression, intestinal obstruction, fistula or abscess formation, and hydronephrosisdue to ureteric compression. [1,3] A case presenting with bowel perforation is extremely rare; to date, only two cases have been reported.[1,4]Desmoid tumors, including MF, are histologically benign. However, they may exhibit a locally aggressive pattern of tumoral growth and local recurrence after incomplete excision.[5,6]They are thought to lack the capacity to metastasize. 6Histologically, a MF is grossly anon-encapsulated, well-circumscribed mass, although its margins may infiltrate microscopically into adjacent structures, particularly the muscularis propria of the small bowel. [3] Microscopic analysis shows that a MF is composed of uninflamed fibroblasts, which are elongated spindle cells with regular uniform nuclei, abundant collagenous stroma, and scant cytoplasm.3 Mitotic activity is sparse and necrosis is absent.[7] Immunohistochemistry staining reveals that the spindle cells are positive for smooth-muscle actin and usually show nuclear staining for beta 1-catenin. [7] However, nuclear immunoreactivity for beta 1- catenin is not pathognomonic for this disease because other entities, including superficial fibromatosis, low-grade myofibroblastic sarcomas, and solitary fibrous tumors, may also show nuclear staining for beta 1-catenin. Additionally, beta 1-catenin negativity does not preclude a diagnosis of fibromatosis. [7] Stout defined MF as “the most incomprehensible group” of fibromatoses[6].
CT and magnetic resonance (MR) imaging are the diagnostic imaging modalities used for preoperative evaluation of mesenteric masses. CT and MR imaging findings associated with MF are mainly related to its underlying histologic characteristics and vascularity, including variable contrast enhancement patterns ranging from mild homogeneous enhancement to heterogeneous enhancement. [7] However, predominantly myxoid stroma lesions typically appear hypodense on CT and may contribute to the high signal intensity on T2-weighted images[7].
Differential diagnosis of a typical MF includes malignant or benign neoplasms of the mesentery (lymphoma, metastases, soft tissue sarcomas versus inflammatory pseudotumors, or extrapleural solitary fibrous tumors). However, when a MF involves the wall of the stomach or small bowel loop as in our presenting case, it may appear to have originated from that site, thereby mimicking a gastrointestinal neoplasm. [6] For example, confusion with a small bowel GIST has occurred, as findings reported by Yantiss et al indicated that a MF involving the gastrointestinal tract wall may be confused with a small bowel GIST. [8,9]Microscopic analysis shows that GISTs may be composed of spindle cells closely similar to those of mesenteric fibromatosis. However, GIST spindle cells are far more cellular and without abundant collagenous stroma. [3] Additionally, MFs are typically negative for cell markers CD34 and D117 in contrast to GISTs, which are generally positive for CD117 and commonly positive for CD34.[3] Among other differential diagnoses, small bowel lymphomas usually appear as polypoid masses with circumferential wall thickening and homogeneous enhancement, [10] not very different from the benign features of MF. However, lymphoma usually has associated lymphadenopathy and infiltrates into other abdominal solid organs, including liver and spleen, which are absent in the case of MF. [10] Complete surgical excision may be the only effective means of cure. However, complete excision is often impossible.
Therefore, there are many adjuvant treatments including radiotherapy, anti-estrogens (e.g., tamoxifen), prostaglandin inhibitors, non-steroidal anti-inflammatory drugs, and cytotoxic chemotherapy. [1]In conclusion, we have reported a rare case of MF causing small bowel perforation which was difficult to differentiate from other malignancies including small bowel GIST or lymphoma. Such a case can be difficult to detect prior to surgical resection.
Why Should An Emergency Physician Be Aware Of This?
To our knowledge, there are few case reports published in English describing the radiologic features of MF presenting with bowel perforation. MF may be confused with gastrointestinal stromal tumor or lymphoma and may present as a surgical emergency. CT imaging played a significant role in the diagnosis and management of this potentially lethal condition.
References
- Shah M, Azam B. Case report of an intra-abdominal desmoid tumour presenting with bowel perforation. Mcgill J Med 2007; 10(2):90-92.
- Kasper B, Ströbel P, Hohenberger P. Desmoid tumors: clinical features and treatment options for advanced disease. Oncologist 2011; 16(5): 682-693.
- Levy AD, Rimola J, Mehrotra AK, Sobin LH. From the archives of the AFIP: benign fibrous tumors and tumorlike lesions of the mesentery: radiologic-pathologic correlation. Radiographics 2006; 26(1); 245-264.
- Jalini L, Hemming D, Bhattacharya V. Intraabdominal desmoid tumour presenting with perforation. Surgeon 2006; 4(2):114-116.
- Ebrahimi-Daryani N, Momeni A, Azizi Asl M, Movafaghi S. Mesenteric fibromatosis (desmoid tumor) presenting as recurrent abdominal abscess: report of a rare case. Govaresh 2008;13(2):128-132.
- Weiss S, Goldblum JR, eds. Enzinger and Weiss’s soft tissue tumors, 4th ed. St Louis, MO: Mosby, 2001:309-346.
- Rodriguez JA, Guarda LA, Rosai J. Mesenteric fibromatosis with involvement of the gastrointestinal tract. A GIST simulator: a study of 25 cases. Am J Clin Pathol 2004; 121(1): 93-98.
- Braschi-Amirfarzan M, Keraliya AR, Krajewski KM, Tirumani SH, Shinagare AB, Hornick JL, et al. Role of imaging in management of desmoid-type fibromatosis: a primer for radiologists. RadioGraphics 2016; 36(3): 767-782.
- Wronski M, Ziarkiewicz-Wroblewska B, Slodkowski M, Cebulski W, Gornicka B, Krasnodebski IW. Mesenteric fibromatosis with intestinal involvement mimicking a gastrointestinal stromal tumour. Radiol Oncol 2011;45(1): 59-63.
- Ghai S, Pattison J, Ghai S, O’Malley ME, Khalili K, Stephens M. Primary gastrointestinal lymphoma: spectrum of imaging findings with pathologic correlation. Radiographics 2007; 27(5):1371-1388.