Information
Journal Policies
The Effectiveness of Nursing Intervention on Breastfeeding-Related Problems among Nursing Mothers in Selected Primary Health Clinics in Lagos, Nigeria
Folami, F*, Ademuyiwa, Y, Olowe, A
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Breastfeeding is a vital component of realizing every child’s right to the highest attainable standard of health, while respecting every mother’s right to make an informed decision about how to feed her baby. Several factors related to the mother and the baby have a negative effect on the duration of exclusive breastfeeding. Most breastfeeding mothers have experienced variety of difficulties because of some of the techniques used. One group pretest-posttest of quasi-experimental was used for this study. The study was conducted among mothers of children less than five years who attended the selected Primary Health Care Centers (PHCs) in Oshodi-Isolo LGA for outpatient clinics and immunization. The multistage sampling technique was used. Two hundred and fourteen participants agreed to participate but only 204 showed up for the training given a response rate of 95.3%. The study results showed that immediate nursing intervention towards lactation related problems are very significant in maintaining exclusive breastfeeding. Recommendations were made based on the findings that all pregnant women should be educated on management of breastfeeding related problems prenatally and establishment of breastfeeding support groups should be adopted.
Breastfeeding, Exclusive Breastfeeding, Breast Engorgement, Sore Nipple, Latch.
1. Background of The Study
Breastfeeding is a vital component of realizing every child’s right to the highest attainable standard of health, while respecting every mother’s right to make an informed decision about how to feed her baby (Angell, Alexander,& Hunt, 2010). Breastfeeding has many advantages for both mothers and infants. Several factors related to the mother and the baby have a negative effect on the duration of exclusive breastfeeding (Folami, 2018). Breast milk contains nutrients at percentages exactly suited to the needs of the infant for growth and development (Colen & Ramey, 2014). Breastfeeding has been associated with lower rates of gastrointestinal, respiratory, and urinary tract infection and less atopic illness in the first year. According to the American Academy of Pediatrics (AAP) policy Statement on Breastfeeding, women who do not have health problems should exclusively breastfeed their infants for at least the first six months of life (John, Cordeiro, Manjima, Reshma, 2015). The importance of appropriate infant feeding and the vital role played by breastfeeding in child survival, growth, and development cannot be over-emphasized (Ho & Yu, 2014). The World Health Organization (WHO) has recommended two years breastfeeding; first six of month’s exclusive breastfeeding; more than eight times breastfeeding per day in the first three months of an infant’s life (Imdad, Yawar, & Bhutta, 2011). The AAP suggested that a woman should try to breastfeed her infant for the first twelve months of life (Tony & Kelly, 2017). Despite the documented value of exclusive breastfeeding during the first months of a child’s life and struggles for promoting this practice, rates for exclusive breastfeeding in Nigeria are below those recommended by the World Health Organization (WHO), which advocates exclusive breastfeeding during the first six months of baby’s life (Rai, Singh, & Singh, 2012). Based on the World Health Organization global data on infant and young child feeding in Nigeria, 22.3% of children were exclusively breastfed for less than 4 months, while 17.2% were exclusively breastfed for less than 6 months, in the year 2010 (Rai, Singh, & Singh, 2012). The technique used in breastfeeding, especially mother-infant positioning and attachment or suckling by the infant, has been shown to be important for the effective transfer of milk from the breast to the child as well as for preventing nipple damage. Ziol-Guest & Hernandez (2010) evaluated mother-infant pairs in a maternity ward and observed that only 2% of pairs achieved optimal latch performance and only 0.2% achieved optimal mother-infant positioning.
Most breastfeeding mothers have experienced variety of difficulties because of some of the techniques used by the mothers. It was observed during the child welfare clinic that many of the nursing mothers failed to practice exclusive breastfeeding as a result of some of the breastfeeding related problems they encountered while breastfeeding (Johnston, & Brown, 2013). Considering that breastfeeding technique seems to be important for maintaining successful breastfeeding; this study explored the effectiveness of nursing intervention on breastfeeding-related problems among nursing mothers in selected primary health care centers in Oshodi-Isolo LGA, Lagos, Nigeria.
As reported by WHO, breastfeeding helps to protect the infant against some of the major causes of childhood morbidity and mortality (Rai, Singh, & Singh, 2012). The review of studies from developing countries shows that infants who are not breastfed are 6–10 times more likely to die in the first few months of life than infants who are breastfed (Johnston, & Brown, 2013). The American Academy of Pediatrics Section on Breastfeeding (AAPSB) currently recommended that starting within one hour of birth, infants should be exclusively breastfed for the first six months of life and that breastfeeding should continue up to 2 years of age or beyond (Padmasree, Varghese, Krishnan, 2017). Unfortunately, infant feeding practices are still far from optimal and in many parts of the world rates of exclusive breastfeeding are low and many women stop breastfeeding earlier than they intended to (Joshi, Magon, Raina, 2016; Kramer & Kakumer, 2012). It is estimated that 1.5 million lives could be saved each year if infants were fed according to recommended breastfeeding practices as reported. Research has also shown an association between duration of breastfeeding and reduction in risk of childhood obesity and cardiovascular diseases in later life (Padmasree, Varghese, Krishnan, 2017).
The nursing intervention provides formal breastfeeding education to nursing mothers on the importance of breastfeeding and its attended benefits. The antenatal period affords an opportunity for providing pregnant women and their partners and families with information about the benefits of breastfeeding at a time when many decisions about infant feeding are being contemplated. Systematic review of the available evidence suggests that breastfeeding education is effective in increasing both the rate of breastfeeding initiation and breastfeeding duration (Colen et al., 2014; Imdad et al, 2011).
- What is the existing knowledge level of nursing mothers on proper positioning of mother and baby?
- What is the knowledge level of nursing mothers on the effective latch?
- What is the knowledge of level of nursing mothers on maternal breast engorgement?
- What is the knowledge level of nursing mothers on sore nipple and its prevention?
- There is no significant difference between the pre and post knowledge level of participant on proper positioning of mother and baby after four weeks of training.
- There is no significant difference between the pre and post knowledge level of participant on maternal breast engorgement after four weeks of training.
- There will be no significant difference between the pre and post knowledge level of participant on effective latch after four weeks of training.
The theoretical model used to guide this study is the general systems theory. This theory was introduced by Ludwig Von Bertalanffy (1969) as a universal theory that could be applied to many fields of study. This theory explains the breaking of whole things into parts and the working of those parts in systems. The theory explains the relationship between wholes and parts, a description of concepts about them, and predictions about how the parts will behave and react (Kozier et al, 2008). This theory explains how effective breastfeeding is a function of the proper positioning, latch, proper emptying of the breast, and attachment of child to the mother's breast.
2. Causes of Breastfeeding-Related Problems Among Nursing Mothers
Studies conducted in North India reveal that there was good attachment in 42% mother-infant pairs and 60% mothers (Moore, Bergman, Anderson, Medley, 2016; Deshmukh, Rawool, Garg, 2010) held infants in correct position. A study in Bangladesh reported that correct breastfeeding position (74%) and good attachment (72.3%) as assessed by Health Care Workers (Deshmukh, Rawool, Garg, 2010). Positioning of the baby's body is important for good attachment and successful breastfeeding. Most difficulties can be avoided altogether if good attachment and positioning are achieved at the first and early feeds (Padmasree, Varghese, Krishnan, 2017). The baby's positioning and attachment to the breast during breastfeeding are fundamental toward the occurrence of different sorts of nipple trauma. Many studies indicate a statistically significant association between position and holding variables for causing nipple lesions (Joshi, Magon, Raina, 2016; Padmasree, Varghese, Krishnan, 2017).
Maternal breast engorgement is one of the most common problems in the postpartum period (Finello, 2015). Maternal breast engorgement is one of the common breast implication occur in third and fourth postpartum day due to excessive production of milk, obstruction to outflow of milk or poor removal of milk by the baby. Engorgement symptoms occur most commonly between days 3 and 5, in that 2-3 of them experience tenderness on day 5, however some cases late as day 9-10. Breast engorgement is a major issue in the early postpartum period as the breast, under the influence of hormonal shift, increase milk production rapidly. For most women engorgement is at its height from 3 to 5 days after birth and slowly recedes but may last for 2 weeks (Ketsuwan, Baiya, Paritakul, Laosooksathit, & Puapornpong, 2018).
Improper suction is also described as a source of trauma which if corrected can become a protective factor (Ketsuwan, Baiya, Paritakul, Laosooksathit, Puapornpong, 2018). The most frequent causes of sore nipples are incorrect positioning at the breast and suction trauma. During the first two to four days after birth, the mother's nipples may feel tender at the beginning of a feeding as the baby's early suckling stretches her nipple and areolar tissue far back into his mouth. If a baby is well positioned at the breast, this temporary tenderness usually diminishes once the milk lets down, and disappears completely within a day or two (Ketsuwan, Baiya, Paritakul, Laosooksathit, Puapornpong, 2018). A poorly latched baby may pinch off the nipple to protect his airway from a forceful milk-ejection reflex. Sometimes a baby will pinch the nipple or irritate it due to a short frenulum, short tongue, small mouth, receding chin, a high palate, or other anatomical condition. Nipple soreness that increases or lasts beyond the first week should be interpreted as a warning that something is wrong.
The most important part of successful breastfeeding is the latch. Feedings could be painful If the baby is not properly latched on to the breast. There are specific techniques that can be used when latching the baby onto the breast. The position in which the baby is held is crucial. When a good position and latch is obtained, breastfeeding can be a wonderful experience between mother and baby (Folami, 2018). Nipple damage and mastitis were more common among mothers with poor positioning and latch (Lawan, 2015). Furthermore, breastfeeding problems were 2.44 times more common among mothers who practice ineffective latch compared to who had effective latch practice (John, Cordeiro, Manjima, Reshma, 2015). The most important factor in decreasing the incidence of nipple pain is the provision of education in relation to proper breastfeeding technique and latch‐on as well as anticipatory guidance regarding the high incidence of early postpartum nipple pain.
One group pretest-posttest of quasi-experimental was used for this study. This design involved comparing participants’ pre and post after implementing an intervention. The design was chosen because it enabled the researcher to compare participants in the pre and post intervention on similar variables. This design considered appropriate because the collection of baseline data allowed the researcher to be relatively confident that the posttest difference occurs because of the intervention. The study was conducted among mothers of children less than five years who attended the selected Primary Health Care Centers (PHCs) in Oshodi-Isolo LGA for outpatient clinics and immunization. The multistage sampling technique was used. The first stage involved a random selection of Oshodi-Isolo Local Government Area among the twenty Local Government Areas in Lagos. The second stage involved the selection of the primary health care centers that used by systematic random sampling. Oshodi-Isolo is the selected Local Government Area, which has five primary health care centers. Three primary health care centers out of the five purposely selected as they are the most attended so that a good percentage of the population was covered. The third stage involved selection of participants for the study. Percentage of total respondents to participate from each center was determined by the average attendance at each center. Oshodi-Isolo is a residential and commercial LGA located on the mainland of Lagos State, Nigeria, with an area of 45 square kilometers. At the last census in year 2006, it had a population of 621,509 people.
An introductory letter was written to the heads of the Primary Health Clinics where the research was conducted. The researcher made arrangement with the head of the PHC Units to select and brief the research assistants on what to do during the training. The date and the time for the training were given to them. The venue for the program was at the children welfare clinic at the primary health care center. The inclusion criterion involves all mothers of children less than five years who breast fed their children. The participants were briefed on the program. Consent was obtained from the identified participants before enrolment into the study. The questionnaire was translated into the local language for the benefit of the participants who are not literate. Pretest was administered with the help of the research assistants and this was served as baseline data. Training was done for four consecutive weeks on effective latch, proper positioning of mother and baby, breast engorgement, and sore nipple. Post-test was administered at the end of training. Each training session lasted for one hour. Data collection was done using a structured, self- administered questionnaire to obtain information from the participants. The validated questionnaire was carefully studied and used to improve the quality of the research instrument. The reliability was pre-tested in one of the PHCS in Ogun state. The Cronbach alpha was used to test the reliability of the instrument. Correlations were made and measured errors were eliminated to ensure reliability of the instrument. This study was carried out in three phases (pre-intervention, intervention, and post intervention). The research assistants collected data using the structured questionnaire. Three trained research assistants assisted in the data collection, prior to the intervention. Four weeks after the intervention, quantitative data was collected with the same instrument from the respondents. The data was reviewed, organized and entered into a computer running the statistical package of social science (SPSS version) 22. Frequency tables were made and numerical data expressed in frequency distribution tables. The result was tested using descriptive and inferential statistical analysis of dependent t-test at 0.05 level of significance to answer the research questions and test the hypotheses.
3. Results
A total of 214 participants agreed to participate but only 204 showed up for the training. Two hundred and four questionnaires were administered, returned, and also found adequate for analysis given a response rate of 95.3%.
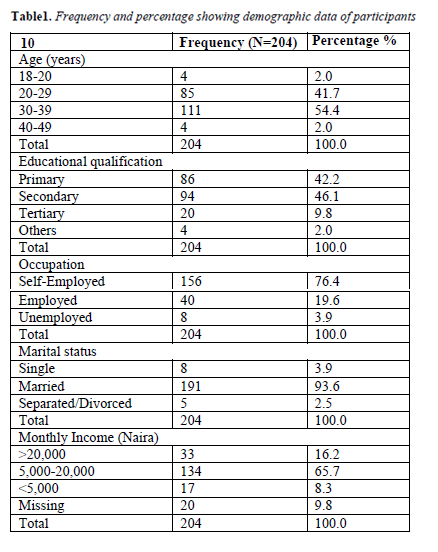
Table 1 shows that majority of the respondents 111 (54.4%) were within the age group 30-39, 191(93.6%) were married and about 46.1% were educated up to secondary school level. Majority were self-employed 156(76.4%), (3.9%) were housewives and 134(65.7%) earned N5000 - N20, 000 monthly.
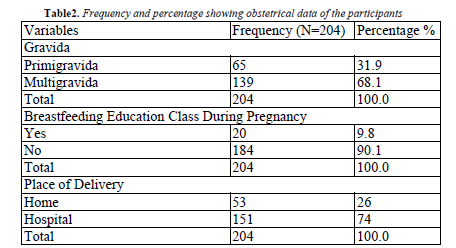
Table 2 presents the distribution of mothers according to the gravida, place of delivery, and whether they attended any breastfeeding education class.
Research Question 1: What is the existing knowledge level of nursing mothers on proper positioning of mother and baby pre intervention ?
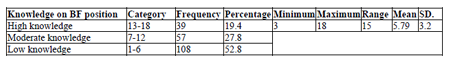
Table 3 reveals the existing knowledge level of nursing mothers on breastfeeding positioning with mean score 5.79 thus it could be said the nursing mothers have low knowledge on adequate breastfeeding positioning.
Research Question 2: What is the knowledge level of nursing mothers on effective latch pre intervention?
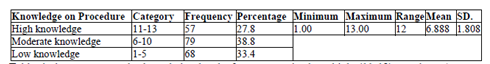
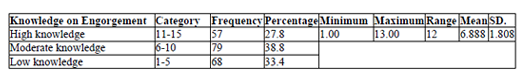
Table 4 above presents the knowledge level of nursing mothers on effective latch. The knowledge level of nursing mothers was categorized as high (11-13), moderate/average (6-10) and low (1-5). Majority 79 (38.8%) of the participants had moderate level of effective latch, 68 (33.4%) had low knowledge level of effective latch, and the remaining 57 (27.8%) had high level of effective latch.
Research Question 3: What level of knowledge do you have on maternal breast engorgement pre intervention ?
Table 5 above presents the knowledge level of nursing mothers on breast engorgement. The knowledge level of nursing mothers on breast engorgement was categorized as high (11-15), moderate/average (6-10) and poor (1-5). Majority 79(38.8%) of the participants had moderate knowledge level of breast engorgement, 68(33.4%) had poor knowledge level of breast engorgement, and the remaining 57(27.8%) had high level of breast engorgement. It could then be said that before the intervention program the knowledge level of nursing mothers on breast engorgement was good.
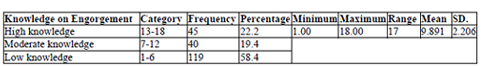
Research Question 4: What is the knowledge level of nursing mothers on sore nipple and its prevention pre intervention?
Table 6 above presents the knowledge level of nursing mothers on sore nipples. The knowledge level of nursing mothers on sore nipples was categorized as high (13-18), moderate/average (7-12) and poor (1-6). Majority 119(58.4%) of the participants had low level knowledge on sore nipples, 40(19.4%) had moderate knowledge of sore nipples, and the remaining 45(22.2%) had high level of sore nipples. The result reveals that the participants had low knowledge on sore nipples before the intervention.
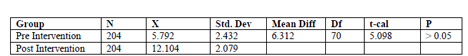
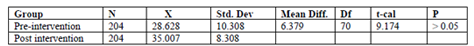
Ho1: There is no significant difference between the pre and post knowledge level of participant on proper positioning of mother and baby after 4 weeks of a training program.
Results in Table 7 indicates a significant difference between the knowledge level pre and post intervention on adequate positioning for effective latch after 4 weeks of a training program. The null hypothesis was rejected. It could be deduced from the findings that the difference between the knowledge level of participants’ pre and post intervention may be because of the educational intervention exposure.
Ho2: There is no significant difference between the pre and post knowledge level of participant on maternal breast engorgement after four weeks of training.
Results in Table 8 indicate a significant difference shows the difference between pre and post-intervention knowledge level after four weeks of training. Therefore, the null hypothesis of no significant difference between the knowledge level of intervention and control groups on breast engorgement after four weeks of training was rejected.
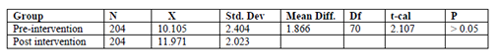
Ho3: There is no significant difference between the pre and post knowledge level of participants on effective latch after four weeks of training.
Results in Table 9 indicate a significant difference between the pre and post knowledge level of participants on effective latch after four weeks of training. The null hypothesis could not be sustained.
4. Discussion of Findings
Results from this interventional study have indicated that training combining discussion with use of educational materials and practical demonstrations for breastfeeding mothers might result in significant improvements in initiation and duration of exclusive breastfeeding. The study results showed that immediate nursing intervention towards lactation related problems are very significant in maintaining exclusive breastfeeding. The positive response of the participant post intervention on the importance of proper positioning of mother and baby and effective latch might be due to the nursing intervention. Adequate knowledge on latch is one of the most important ingredients in the breastfeeding relationship. This result is corroborated with the report of John et al. (2015) that found out that inadequate parental education will increase breastfeeding-related problems. Proper positioning and latch benefits mother because they help reducing the risk of sore and chewed nipples, bleeding nipples, raw nipples, and chafed nipples.
5.Recommendation
Based on the findings of this study, the following recommendations were made:
- All pregnant women should be informed about the benefits and management of breastfeeding problems prenatally.
- All pregnant women should be helped to initiate breastfeeding within one hour of birth.
- Foster the establishment of breastfeeding support groups and refer mothers to Lactation Consultants.
- Mass media should intensify efforts by including more programs on breast feeding problems and solutions.
References
- Angell, C., Alexander, J., & Hunt, J. (2010). Researching breastfeeding awareness in primary schools. British Journal of Midwifery, 18(8).
- Colen, C. G., & Ramey, D. M. (2014). Is breast truly best? Estimating the effects of breastfeeding on long-term child health and wellbeing in the United States using sibling comparisons. Social Science & Medicine, 109, 55-65.
- Deshmukh, P., Rawool A., Garg, B. (2010). Where and How Breastfeeding Promotion Initiatives Should Focus Its Attention? A Study from Rural Wardha. Indian Journal Community Medicine, 35, 226–229.
- Folami, F. F. (2018). Nurse–Based Intervention on Exclusive Breastfeeding Practice among Childbearing age Women in Southwestern Part of Nigeria. America Academic of Pediatrics, 142 (1), 691.
- Finello, K. (2015). Common breastfeeding discomforts and how to treat them. American Academy of Pediatric https://www.healthy children.org.
- Ho, Y. J., & Yu, C. C. (2014). Attitudes of high school and vocational school students toward breastfeeding in Taiwan. The Journal of perinatal education, 23(2), 89-95.
- Imdad, A., Yawar, M., & Bhutta, Z (2011). Effects of breastfeeding promotion intervention on breastfeeding rates with Infant Feeding Practices Survey II. Maternal and child health journal, 16(7), 1421-1430.
- Johnston, R. G., & Brown, A. E. (2013). Maternal trait personality and childbirth: the role of extraversion and neuroticism.Midwifery, 29(11), 1244-1250.
- Joshi, H., Magon, P., Raina, S (2016). Effect of mother-infant pair's latch-on position on child's health: A lesson for nursing care. Journal of Family Medicine and Primary Care, 5(2), 309-313.
- John, L., Cordeiro, M., Manjima, M., Reshma, G (2015). Knowledge regarding breast problemsamong Antenatal Mothers in a selected hospital Mangalore with a view to develop an information booklet. International Journal of Recent Scientific Research, 6 (6) 228-232.
- Ketsuwan, S., Baiya, N., Paritakul, P., Laosooksathit, W., Puapornpong, P (2018). Effect of herbal compresses for maternal breast engorgement at postpartum: A Randomized Controlled Trial, Breastfeed Medicine, 5,361- 365. doi: 10.1089/bfm.
- Kozier, B., Erb, G., Berman, A., Synder, S.J., Bouchal, D.S.R, et al. (2009). Fundamentals of nursing: concepts, process and practice (2nd Ed.). Toronto press.
- Lawan, H. (2015). Breast Feeding Problem as it Affects Mother and Infant’s Health. (A Study of Kano Metropolis, Kano State, Nigeria). International Journal of Scientific Engineering and Applied Science (IJSEAS) 1 (I5) 356-360.
- Padmasree, S., Varghese, L., Krishnan, A (2017). Effectiveness of prenatal teaching on prevention of breast engorgement. International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 6, 3927-3931.
- Rai, R., Singh, P. K., & Singh, L. (2012). Utilization of maternal health care services among married adolescent women: insights from the Nigeria Demographic and Health Survey, Women's Health Issues, 22(4), e407-e414.
- Tony, G. & Kelly, M. (2017). Breastfeeding Support: A Geographic Perspective on Access and Equity. Journal of Human Lactation, 33(4) 770-780.
- Ziol-Guest, K. M., & Hernandez, D. C. (2010). First-and second-trimester WIC participation is associated with lower rates of breastfeeding and early introduction of cow's milk during infancy. Journal of the American Dietetic Association, 110(5), 702-707.