Information
Journal Policies
Knee Sepsis Following ACL Reconstruction – A Modified Approach for Management
Amro Zanfaly1*, Adel A Fouda1, Waleed Faisal1
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction: Background: Post ACL reconstruction knee sepsis is rare but disastrous. This complication should be treated as an emergency. Repeated arthroscopic debridement and lavage is considered the main line of treatment by most authors. Another promising treatment option is single arthroscopic debridement followed by repeated suction irrigation.
Patients and Methods: Seventeen infected cases of 750 cases had anatomical ACL reconstruction with hamstring autograft was managed with single arthroscopic debridement followed by repeated suction irrigation. Continuous patient monitoring both clinical and radiological during the irrigation period was done was done for all cases.
Results: During the period of irrigation clinical and laboratory parameters showed rapid improvement. Later only one case had recurrent infection. The mean Lysol score at the final follow up was 79.7. The graft was retained in 16 cases and discarded in one cases.
Conclusion: This line of treatment is successful compared with repeated arthroscopic debridement but with less cost, better tolerated by patients and avoids repeated surgical trauma.
ACL reconstruction, knee sepsis, suction irrigation, ACL surgery failure,Orthopedics
1. Introduction
Knee infection following ACL reconstruction is not common; the recorded incidence is 0.14% – 1.8 % [1,2]. The controversies about diagnosis and management of this serious complication are not too much. All arguments are concerned with graft retention versus graft rejection, duration of antibiotic therapy, to do synovectomy or not and time of revision if the graft would be discarded. There is a general agreement about repeated arthroscopic debridement up to three times to control knee sepsis following ACL reconstructionR. A modification of this technique was followed to decrease the need for repeated surgical procedures and increase patient comfort. The purpose of this study is to describe the technique of single athroscopic debridement followed by repeated arthroscopic lavage following ACL reconstruction knee sepsis and the results were recorded.
2. Patients And Methods
In the period from June 2010 to august 2015, 750 cases with ACL deficient knee had reconstruction with anatomical single bundle technique using hamstring autograft. The mean age was 25.5 years (Range 19 – 43), 713 cases were males while 37 cases were females. All cases had primary ACL reconstruction; cases with previous failed ACL reconstruction were excluded from this study. The mean follow up period was 14 months (Range: 11 - 21months). 274 cases (36.5%) had previous knee arthroscopy for diagnostic purpose within one year before ACL reconstruction. 184 cases (24.5%) had concomitant meniscal debridement along with ACL reconstruction, 114 cases (15.2%) had concomitant meniscal repair and 24 cases (3.2%) had micro fracture for chondral ulcers along with ACL reconstruction. 22 cases (2.9%) were diabetics. The number of infected cases recorded was 13 (1.7%). Infection was presented in the early post-operative period (5–28 days post-operative). The clinical presentation of all cases was nearly the same, unusual knee pain, fever, increasing effusion, deterioration of knee range of motions.
Once clinical suspicious was present diagnostic work up started. Immediate knee aspiration was routinely done for all suspected cases. Synovial fluid analysis for total and differential leucocytic count and culture and sensitivity were done. Blood examination for ESR, CRP and CBC were also done immediately.
In all cases synovial fluid analysis had high content of pus cells over 50.000 cells/uL, however not all culture and sensitivity results were positive for bacterial growth. 11 (84.5%) cases had positive cultures for bacterial growth.
Eight cases had coagulase-negative Staphylococcus (CNS), two cases had methicillin-sensitive (MSSA) Staphylococcus aureus and one case had methicillin-resistent (MRSA) Staphylococcus aureus. In all cases ESR and CRP were elevated and leucocytic count showed relative increase of polymorphs over 75% of total.
Intravenous antibiotic therapy was started once cases were clinically presented just after sample aspiration. Double therapy of I.V. third generation cephalosporins and amoxicillin/ clavulanic acid were used till the results of culture and sensitivity.
Arthroscopic management was the next step; it was carried out on the same day of clinical presentation. All cases had spinal anaesthesia with tourniquet applied to the upper thigh. The same portals for ACL reconstruction were re used. All compartments were examined with removal of blood clots, necrotic tissue and fibrin layers. Assessment of ACL graft for tension and synovial biopsy for microbiological examination followed by copious irrigation with 10 liters of saline was routinely done for all cases. Gentamicin was added to the irrigating solution in a dose of 80 mg for every 1L of saline.
ACL graft was removed in one case as it was found damaged and lax. In 16 cases the graft was intact with good tension.
A system of repeated suction irrigation was applied to the infected knee. A catheter inserted through the anterolateral portal used for irrigation and 2 wide pore tubes 16mm of the suction drain were inserted through the anteromedial portal and the far medial portals. Repeated post-operative irrigation with 1000 cc saline each time with continuous drainage was done every 4 hours. Systemic I.V. antibiotic therapy continued according to culture and sensitivity results. Temperature chart was done every six hours and serial CRP and CBC were routinely done every two days.
The catheter and drains were removed from three to four days depending on knee pain, body temperature, and state of fluid coming out of the knee and CRP levels. The parameters used as guides for cessation of continuous suction irrigation were
1. Two successive CRP of decreasing values approaching normal levels
2. No elevation of body temperatures at least for 24 hours
3. Mild usual post-operative knee pain
4. Clear fluid coming out from the knee for 24 hours at least
Intravenous antibiotic therapy was continued till CRP levels reached normal followed by oral antibiotic therapy for a period equal to I.V. therapy then stopped provided that the last two CRP levels were normal (3-5 mg/L).
Continuous quadriceps and ROM exercises the same as typical post-operative ACL rehabilitation program were encouraged.
3. Results
In all cases synovial fluid analysis had high content of pus cells over 50.000 cells/uL, however not all culture and sensitivity results were positive for bacterial growth. 11 (84.5%) cases had positive cultures for bacterial growth.
Eight cases had coagulase-negative Staphylococcus (CNS), two cases had methicillin-sensitive (MSSA) Staphylococcus aureus and one case had methicillin-resistent (MRSA) Staphylococcus aureus. In all cases ESR and CRP were elevated and leucocytic count showed relative increase of polymorphs over 75% of total.
Patient evaluation in this study was done in two stages; the first one was during the period of irrigation then after weaning from suction irrigation.
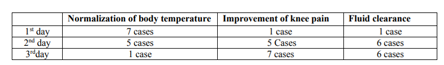
During suction irrigation period (Table 1)
Temperatures: all cases showed gradual decrease in body temperature by the first day in 7 cases, 5 cases in the second day and 1 case by the third day then became within normal values afterwards
Pain: Pain assessment was subjective, however generally pain gradually decreased in all cases to usual post-operative pain levels. There was no reported increasing pain than usual.
Range of motion: Marked restriction of knee motions was present in all cases before treatment. Range of motion improved gradually after subsidence of clinical manifestations of infection and relief of pain.
Drained fluid become clear in eight cases after two days and in nine cases after three days
CRP levels: There was gradual decrease of CRP levels in all cases to reach near normal values within 4 days. Normalization of CRP took a mean period of 17 days to be reached
The mean duration of intravenous antibiotic therapy was 17 days (range 15 –25) while the mean duration of oral antibiotic therapy was 20 days (range 15 – 28), Persistent mild knee effusion was present in 4 cases for 3 months Quadriceps wasting happened in all cases but improved with rehabilitation. Five cases had limitations of knee ROM with variable degrees. Limitation of full flexion (Range 90º – 125º) was the main deficit but full extension was regained by all cases. Although flexion deficit persists but it was tolerated by these patients
At the end of follow up period only one case reported with recurrent infection otherwise no one had neither clinical or laboratory evidence of recurrence, for that case re - arthroscopy was done, the graft and the fixing devices were removed due to the persistence of infection and deteriorated appearance and laxity of the graft.
The mean modified Lysholm knee score was 79.7, four cases were rated as excellent, five cases were good, seven cases were fair and one case had poor result .as regard the fair results were attributed to pain which is marked during severe exertion and limitations of knee ROM
4. Discussion
Post ACL reconstruction knee sepsis is rare but disastrous. This complication should be treated as an emergency to completely eradicate the infection and continue post-operative ACL rehabilitation program promptly.
Infection not only produces graft failure and arthrofibrosis but also destroys the articular cartilage of the knee joint leading to later degenerative arthritis[3]. The final outcome of this complication would be painful stiff knee, if not properly controlled.
Previous lines of treatment of post ACL reconstruction knee sepsis involved single or repeated arthroscopic lavage with graft retention or removal according to the present situations. Another line used was arthrocentesis and joint irrigation without arthroscopic intervention[4]. Nowadays most authors recommend repeated arthroscopic debridement and systemic I.V. therapy as the main treatment of post ACL reconstruction knee sepsis[5].
Sometimes single attempt of arthroscopic debridement and lavage may be insufficient to eradicate the infection and repeated procedure is required up to three times to control this complication.
Repetition of this surgical procedure although reported success by most authors to eradicate the infection and preserve the graft5 yet this requires repeated surgical trauma and repeated anaesthesia which represent a financial and psychological loads on the patient and his family.
A modified simpler approach was used to control this complication, single arthroscopic debridement followed by repeated suction irrigation for a variable period guided by clinical and laboratory parameters in combination with systemic I.V. antibiotic therapy.
This approach is well tolerated by patients as a single procedure, no need for repeated anaesthesia, no repeated surgical trauma, less cost and more psychologically tolerable.
There is a debate about addition of antibiotics to the irrigating saline some authors recommend use of intra-articular antibiotics[6,7], while others refuse this[8,9]. In the current study local gentamycin was used during the initial arthroscopic drainage but not during suction irrigation. Previous studies reported sufficient antibiotic levels in the synovium after I.V. use[10] and to avoid irreversible chondrotoxicity of continuous administration[11]. Addition of gentamycin to the irrigating solution during initial arthroscopic debridement is safe in the mentioned dose (80 mg for each 1L of irrigating saline) and for a limited time[12,13].
Clinical and laboratory evaluation of cases in the period of suction irrigation and after removal of the irrigating tubes showed nearly the same results of repeated arthroscopic debridement an lavage as regard decrease of systemic fever, improvement of knee pain, range of motion, subsidence of knee effusion and decrease CRP levels. Also the duration of systemic antibiotic therapy is nearly the same as cases treated with repeated arthroscopic debridement
Till now there are no studies that thoroughly compare the early and remote results of repeated arthroscopic drainage versus single arthroscopic drainage followed by continuous suction irrigation. Also is effect of repeated fluid infusion on the graft material and on the articular cartilage is still not documented.
Compare the study results with repeated debridement and single debridement without suction irrigation
5. Conclusion
Single arthroscopic debridement followed by continuous suction irrigation has a success comparable to repeated arthroscopic debridement and lavage but without repeated exposure to anaesthesia, no repeated surgical trauma, less cost and better psychologically tolerated than repeated surgeries.
References
- Indelli PF, Dilingham M, Fanton G, Shurman DJ Septic arthritis in postoperative anterior cruciate ligament reconstruction. Clin Orthop Rel Res (2002), 398:182–188
- Torres-Claramunt R, Pelfort X, Erquicia J, Gil-González S, Gelber PE, Puig L, Monllau JC Knee joint infection after ACL reconstruction; prevalence, management and functional outcomes. Knee Surg Sports Traumatol Arthrosc (2013), 21(12):2844–2849
- Hogan CJ, Fang GD, Scheld WM, Linden J, Dibuch DR. Inhibiting the inflammatory response in joint sepsis. Arthroscopy (2001) 17:311–315.
- Monaco E, Maestri B, Labianca L, Speranza A, Vadala` A, Iorio R, Ferretti A Clinical and radiological outcomes of postoperative septic arthritis after anterior cruciate ligament reconstruction. J Orthop Sci (2010), 15(2):198– 203.
- Cheng Wang, Yee Han Dave Lee, Rainer Siebold. Recommendations for the management of septic arthritis after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc (2014) 22:2136–2144.
- Parisien JS, Shaffer B. Arthroscopic management of pyarthrosis. Clin Orthop Relat Res. 1992;275:243–247.
- Gainor BJ. Instillation of continuous tube irrigation in the septic knee at arthroscopy. Clin Orthop Relat Res. 1984;183:96 –98.
- Thiery JA. Arthroscopic drainage in septic arthritides of the knee: a multicenter study. Arthroscopy. 1989;5:65– 69.
- Ivey M, Clark R. Arthroscopic debridement of the knee for septic arthritis. Clin Orthop Relat Res. 1985;199:201–206.
- Frimodt-Moller N, Riegels-Nielsen P. Antibiotic penetration into the infected knee. A rabbit experiment. Acta Orthop Scand. 1987;58:256–259.
- Ga¨chter A. Gelenkinfekt. Arthroskopische Spu ¨lbehandlung—Hints und Tricks. Arthroskopie. 1994;7:98 –101.
- Lescun TB, Adams SB, Wu CC, Bill RP, Van Sickle DC (2002) Effects of continuous intra-articular infusion of gentamicin on synovial membrane and articular cartilage in the tarsocrural joint of horses. Am J Vet Res 63(5):683–687.
- Hamidreza Yazdi, Amin Moradi and Mirco Herbort. The effect of gentamicin in irrigating solutions on articular infection prophylaxis during arthroscopic ACL reconstruction. Archives of Orthopaedic and Trauma Surgery. February 2014, Volume 134, Issue 2, pp 257–261.