Information
Journal Policies
Metal Block in Primary Total Knee Arthroplasty in Severe Tibial Defect in Varus Knee
Emad AbdElhady1*, Mohammed El Sadek1, Mohammed S ElAttar2
2.Lecturer of orthopedic surgery, faculty of Medicine, Zagazig University, Egypt
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background: Bone defects are one of the challenging problem of primary total knee replacement (TKR) it can be difficult to introduce stable well-aligned components. The defects generally occur on the tibial side, but can affect the distal femur, and are typically asymmetrical and peripheral, although there may be contained deficiencies owing to cyst formation. And one of the main goals of total knee arthroplasty depends on obtaining and restoring mechanical alignment, and reconstructing substantial amounts of bone lost using metal block, wedges with/without stem augmentation.
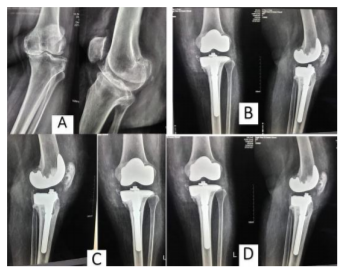
Patients and methods: Twenty-five patients (average age 67 years) who had a varus alignment of the knee of more than 20° were included in this study. The mean follow-up period was 34 months. Posterior -stabilized prosthesis were used in 12 knees and cruciate retaining in 13 knees. Surgical exposure was anterior approach in all knees. Ligament balancing and gap technique was used. Bony reconstruction using a metal medial wedge or block with a stem with offset in 12 cases. The stem length was 100 mm, stem in all cases was uncemented press fit stem was used. Metal wedge of sizing for reconstruction the bone defect was measured after doing standard tibial cut. Rehabilitation and mobilization began on the first postoperative day assisted by a physical therapist with full weight bearing. Outcomes were evaluated using the American Knee Society Score.
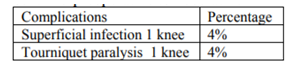
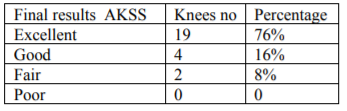
Results: The average Knee Society knee score was 45 points preoperatively and 83 points at the final follow-up. Excellent results were in 76% (19 knees) and good in 16% (4 knees) and fair in 8%. (2knees). Complications in one case with superficial infection and one case with tourniquet paralysis that recovered on final follow-up. Postoperative range of motion was improved 35±15 degrees. Height of joint line was restored and no case of patella Baja.
Conclusion: The use of modular metal block augmentation devices for proximal tibial defects could serve as a simple, rapid, and effective technique that improve the results, and the inclusion of a medullary modular stem in the implant component give greater stability for the prosthesis. There are no standards for the augmentation in primary total knee arthroplasty, and each case should be dealt with according to the degree of deformity and bony defect intraoperatively.
Knee arthroplasty, knee prosthesis, osteoarthritis, results,Orthopedics
1. Introduction
Total knee arthroplasty (TKA) provides excellent results for pain relief and functional recovery in patients with osteoarthritis (OA) of the knee [1]. Severe deformities and marked bone defects were a challenge in reconstructing bone deficiencies and achieving perfect soft-tissue balancing. Combination of bone graft or metal augmentation and stem extension is indicated in -non-contained bone deficits greater than 15-mm deep [2].
Bone grafting of bone defect restore the bone stock, need close follow-up until graft incorporation, with risk of osteonecrosis, and bone collapse [3,4]. Metal augmentation achieve early fixation, allow early postoperative rehabilitation[5,6]. In Primary total knee arthroplasty the defects either tibial or femoral or both types, classifications of medial tibial defect by Anderson orthopaedic research institute [7] classifies the defect into three types. Type 1- minor defect that not compromise the component stability. Type 2: Loss of cancellous bone require reconstruction, A: one condyle, B: both condyles. Type 3: Bone loss that compromise a major portion of the condyle. Treatment of the tibial defect in primary total knee arthroplasty related to the type either a contained or peripheral defect and size of the defect. Stable positioning of tibial components is difficult and presents technical difficulties.
Different methods for treating medial tibial bone defects include increased tibial bone resection including the defect, lateralizing and translation of the tibial component, cement filling with or without screws, allogenic or autogenous bone grafting, metal augmentation with wedge or block of different sizes, and the use of custom-made prostheses with addition of high cost [8]. Metal augmentation is one of the most common method for reconstruct tibial bone defects [8]. A wedge-shaped augmentation and a rectangular block-shaped augmentation used in such cases, metal augmentation transmits loads and decrease cement mantle strains between the tray and tibial plateau [8]. A high rate of radiolucent lines occurs beneath the metal wedge but not of progressive types [1,9,10]. The benefits of modular augments lie in the simplicity of replacing the bone defect without the additional risks associated with bone grafts. A stemmed implant is commonly used. Modular metallic augments are being increasingly indicated and used in deficient proximal tibial bone. Intramedullary stems used in conjunction with tibial metaphyseal metallic augments reduce the mechanical burden, bone stresses and micro motion between bones and implant [11].
2. Patients And Methods
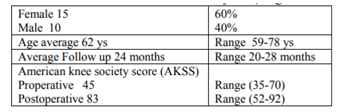
Between Jan 2013-Jul 2016, 25 knees in 15 patients with a severe varus malalignment of the knee of more than 20 degrees were included in this study. All patients were operated on at Zagazige university Hospital, arthroplasty unit. Patients were followed up for a minimum of 2 years. The mean follow-up period was 24 months (range 20–28 months). There were 15 women and 10 men (60 and 40%, respectively). The average age at the time of operation was 68 years (range 59–78 years). Table1
Standing anteroposterior X-ray and lateral radiographs were obtained preoperatively and postoperatively for alignment of the limb, position of the tibial and femoral components, and presence and site of radiolucent lines at the bone– cement interface and progressive or not on follow up. The anteromedial Para patellar approach was used in all cases. Soft tissue release was in the medial and posterior aspect in varus knees. Releasing the soft tissue gradually according to alignment gained and balancing obtained of the knee and prosthesis.
To obtain adequate balance the flexion and extension gaps should be equal by bony cuts and soft tissue balancing. Modular augmentation was used to restore the normal level of the joint line, balanced flexion- extension gaps. Preoperative assessment of the expected medial upper tibial defect was carried out for all patients on the study of anteroposterior and lateral X-ray. Shape and size of the block can be expected from preoperative radiological evaluation. All types and sizes of blocks and stem augments were available intraoperative. Nexgen Knee Replacement (Zimmer Biomet, USA) was used in all patients. Outcomes in this study were evaluated using the American Knee Society Score (0–100 points) [13].
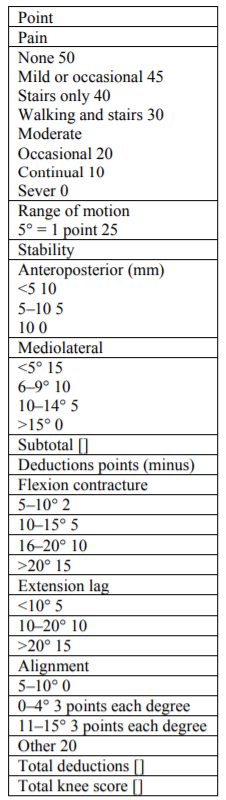
The score was recorded before surgery and at the latest follow-up and comparing the results. Range of motion was evaluated on Preoperative and postoperative clinical examination, recorded and compared. We have used a metal blocks in managing uncontained peripheral defects of ≥ 4 mm in the proximal tibial plateau. The purpose of this prospective study was to determine clinical and radiologic outcomes of primary TKA with metal block for medial tibial bone defects and the frequency and risk factors for radiolucent lines of primary TKR performed using this technique with a minimum follow-up of 2years. The American Knee Society has proposed this rating system (the American Knee Society Score) to be simple but more exact and objective (Table2).
This system is subdivided into a knee score that rates only the knee joint and a functional score that rates the patient’s ability to walk and climb stairs. There are three main parameters: pain, stability, and range of motion. A total of 100 points will be assigned to a well-aligned knee with no pain, 125’ of motion, and negligible.
3. Surgical Technique
After Spinal\epidural anesthesia and using a pneumatic tourniquet, a midline longitudinal skin incision exposing the knee joint with a medial Para patellar capsular approach. Intramedullary guides were inserted to cut the distal femur in 5-7 degrees of valgus in relation to the anatomical axis of the limb. Proximal tibia was perpendicular to the tibial mechanical axis. The measured resection technique using the epicondylar axis, Whiteside’s line, posterior condylar axis as an anatomical landmarks to adjust rotational alignment of the femur in 3 degrees external rotation. The rotational alignment of the tibia was determined using a anatomical landmark reference identified by tibial anteroposterior line that connected the medial one-third of the tibial tuberosity and the center of the tibial insertion of the posterior cruciate ligament. For tibial metal augmentation, rectangular flat blocks wedges of different sizes according to the defect were used in combination with 100-mm-long stem extensions. Perfect medial and lateral soft tissue ligamentous balancing was carried out. In varus knees, after removal tibial and femoral osteophytes, release of the deep part of medial collateral ligament, posterior and medial capsule, posterior oblique ligament on step manner, the superficial pat of medial collateral ligament and pes anserienus tendon also need release in severe deformity.
In flexion contracture knees, removal of posterior osteophytes posterior capsular release and gastrocnemius release[12]. The femoral and tibial components were fixed with cement (CEMEX Bone cement) to the cut surface by finger packing, while the stem extensions were press-fitted without cement [13,14]. Axial compressive load was applied in knee extension with a trial insert until the cement setting occurs. Postoperative early active range of knee exercises and full weight bearing on a walker started one or two days after operation, the severity of pain and general conditions of patients determines the degree of increasing patient activity postoperative rehabilitation program.
To compare patient background characteristics, we used the Mann–Whitney U and chi-square tests for continuous variables and nominal scales, respectively. In addition, we used the Kaplan-Meier method to compare implant survival rates and the log-rank test to compare the differences in survival rates between the metal augmentation and control groups. P < 0.05 was considered statistically significant.
We used the Mann–Whitney U and chi-square tests to compare patient’s background characteristics, for continuous variables and nominal scales, respectively. The Kaplan-Meier method was used also to compare implant survival rates and the log-rank test to compare the differences in survival rates between the metal augmentation and control groups. P < 0.05 was considered statistically significant.
3. Results
The mean follow-up period was 24 months (range 20–28 months). This study presents the prospective results of a clinical and radiological follow-up of 25 knees in 15 patients operated upon for primary TKA with severe varus and medial tibial bone defect using Nexgen Knee Replacement (Zimmer Biomet, USA) with metal block using metal block and press fit stems. The mean preoperative range of motion was 65±15 degrees (range 55–100).
There was significant improvement in the mean postoperative range of knee flexion which was 65+/- 15 preoperative to 100 +/-15 postoperative 35±15 was the average increase in flexion range postoperative) (p value: 0.023). The average period of physiotherapy before gaining near-normal daily activities was 25 days (range 25–40 days). The mean hospital stay was 9 days (range –12 days). The average preoperative American Knee Society Score was 45 points (range 35–70). At the final follow-up the average American Knee Society Score for all the replaced knees was 83 points (range 58–92) Improvement was significant (p value: 0.043). Radiologically, there were no signs of loosening zones at the latest follow-up for all patients. Medical complications were not recorded for any of the patients included in this study. One patient developed tourniquet pa and was managed by removal of all constrictive dressings and repositioning of the knee to 20–30 degrees of flexion.
A plantigrade ankle foot orthosis was applied and stretching was started to prevent equinus contracture. After 2 months, EMG and nerve conduction studies showed recovery, and patients done well afterward.
4. Discussion
Erosion secondary to arthritic change, trauma, osteonecrosis, and a previous osteotomy are the aetiology of bone defects in primary TKR[15,16]. The condensed sclerotic surface defects were typically observed at revision surgery, and removal of this component an osteopenic surface is revealed. Varusdeformities are always associated with medial defects, as in our series, whereas central-lateral defects often present with valgus malalignment[17,18].
If the tibial components found to be unstable during trial reduction augmentation is required, and this is occurs when > 40% of the bone-implant interface is unsupported by host bone in the presence of a defect greater than 5 mm in depth[15,16].
Options for defect treatment include; resection of more tibial bone, filling the defect with cement with or without reinforcing screws, the use of modular augments, bone grafting, or custom –designed components[15,17,19-24]. Also, the use of a long stem Oran offset stem can assist with positioning of the component, supplement fixation, and reduce stress at the bone implant interface[25-28].
Dorr et al [29] recommended that bone resection be limited to 10 mm distal to the lateral subchondral plate or 5 mm distal to the medial subchondral plate. More tibial resection with a thicker polyethylene insert should be reserved for shallow defects of < 10 mm.[17,30]It has been shown that a distal tibial resection reduces the strength of osseous support and may result in the use of a narrower tibial component, further reducing the area of support with increased loading[28-31].
Defects of < 5 mm can be filled with methyl methacrylate, [15,17,26,29] and the additional use of a cancellous screw can help to stabilize the component while the cement is polymerizing[17,30]. However, several biomechanical studies have questioned the durability of this technique and Insall [17] advised against it. Limiting the use of cement augmentation to small contained defects has been recommended by several authors[14,17,32,33].
Windsor, Insall and Sculco [32] reported using the resected femoral condyle secured with countersunk cancellous screws as an autograft to treat tibial defects in primary TKR. They reported that this enabled restoration of bone stock and more physiological load transfer when union occurs. However, Laskin [34] reported a failure rate at five years of 33% after using an autograft in primary TKR.
Although contained defects are easily filled with bone graft, peripheral defects are more difficult, as the creation of a bleeding bed of host bone may require additional deeper cuts to remove the sclerotic areas of bone, and filling the host bed with graft may be difficult in cases with severe erosions.[17,29] The use of allograft to treat massive defects at TKR has been reported, but these have limited Osseo-inductive power compared with auto grafts and can fail, along with the risk of disease transmission[30]. Dorr et al [29] recommended that graft be used for tibial defects involving > 50% of either medial or lateral plateau, requiring > 5 mm width of cement.
Modular augmentation of the component facilitates the treatment of bony defects. The devices are available in wedge and rectangular shapes, can be attached using cement or screws, allowing up to 20 mm of segmental bone loss to be replaced, [26-30] and offer immediate support with satisfactory transfer of load[26,27,31,32]. The short to medium term results of this form of augmentation have been well documented. Chen and Krackow [33] argued that while angular wedges often preserve host bone, rectangular augmentations are more stable biomechanically because they reduce shear loads at the bone-augmentation interface. Augments are suitable for peripheral tibial defects > 5 mm where there is a tendency for the trial to displace at time of reduction[14,33].
In the current series, rectangular metal augments were used to treat uncontained defects of > 4 mm. The clinical results obtained, in terms of range of movement, American Knee Society scores, OKS and WOMAC score, were good to excellent, and no failure of the prosthesis was observed. RRLs > 1 mm in width between the block-cement and bone were noted in five knees (11%) during the first postoperative year, after which no further progression occurred.
5. Conclusion
Modular metal block augmentation used in peripheral medial tibial defects in primary total knee arthroplasty gives a simple, decreased operative time, and dependable surgical method that presents a predictable result. The addition of a medullary tibial stem in the tibial component gives more stability to the prosthesis and increase prosthesis longevity. Metal augmentation in primary TKA is a case specification according to severity and depth of defect intraoperatively after achieving perfect stability and balance of the prosthesis and knee all through range of motion.
References
- Gothesen O, Espehaug B, Havelin L, Petursson G, Lygre S, Ellison P, et al. Survival rates and causes of revision in cemented primary total knee replacement: a report from the Norwegian Arthroplasty Register 1994–2009. Bone Joint J. 2013; 95-B (5):636–42.
- Brand MG, Daley RJ, Ewald FC, Scott RD. Tibial tray augmentation with modular metal wedges for tibial bone stock deficiency. Clin Orthop Relat Res. 1989; 248:71–9.
- Dorr LD, Ranawat CS, Sculco TA, McKaskill B, Orisek BS. Bone graft for tibial defects in total knee arthroplasty. Clin Orthop Relat Res. 1986; 205:153–65.
- Laskin RS. Total knee arthroplasty in the presence of large bony defects of the tibia and marked knee instability. Clin Orthop Relat Res. 1989; 248:66–70.
- Hvid I. Trabecular bone strength at the knee. Clin Orthop Relat Res. 1988; 227:210–21.
- Kikkawa T, Okano T, Hagino H, Otsuki R, Katagiri H, Teshima R. Knee deformity in rheumatoid arthritis is closely correlated with generalized osteoporosis. Mod Rheumatol. 2008; 18: 45–51.
- Engh G.A classification of bone defects in revision total knee arthroplasty. Presented at the Knee Society Interim Meeting, Philadelphia, Pennsylvania 1992
- Cuckler JM: Bone loss in total knee arthroplasty: graft augment and options. J Arthroplasty 2004, 19:S56–S58.
- Brand MG, Daley RJ, Ewald FC, Scott RD: Tibial tray augmentation with modular metal wedges for tibial bone stock deficiency. Clin Orthop Relat Res 1989, 248:71–79.
- Pagnano MW, Trousdale RT, and Rand JA: Tibial wedge augmentation for bone deficiency in total knee arthroplasty: a follow up study. Clin Orthop Relat Res 1995, 321:151–155.
- Closkey RF, Rawlinson JJ, Davis N, Wright TM, Windsor R (2008) Stemmed implants improve stability in augmented constrained condylar knees. Clin Orthop Relat Res.466 (11): 2639-2643.
- Cuckler JM. Bone loss in total knee arthroplasty: graft augment and options. J Arthroplasty 2004; 19 (4 Suppl 1): 56–58.
- Hernandez-Vaquero D, Garcia-Sandoval MA, Fernandez-Carreira JM, Gava R. Influence of the tibial stem design on bone density after cemented total knee arthroplasty: a prospective seven-year follow-up study. Int Orthop 2008; 32:47–51.
- Jazrawi LM, Bai B. The effect of stem length, diameter and the use of cement on tibial component fixation stability. J Arthroplasty 1999; 14:262–263.
- Cuckler JM. Bone loss in total knee arthroplasty: graft augment and options. J Arthroplasty 2004; 19(Suppl 1):56–58.
- Radnay CS, Scuderi GR. Management of bone loss: augments, cones, offset stems. Clin Orthop 2006; 446:83–92.
- Insall JN. Surgical techniques and instrumentation in total knee arthroplasty. In: Insall JN, ed. Surgery of the knee. Fourth ed. New York: Churchill Livingstone, 2006:1455– 52.
- Dennis DA. Repairing minor bone defects: augmentation & autograft. Orthopedics 1998; 21: 1036–1038.
- Pagnano MW, Trousdale RT, Rand JA. Tibial wedge augmentation for bone deficiency in total knee arthroplasty. Clin Orthop 1995; 321: 151–155.
- Harris AI, Poddar S, Gitelis S, Sheinkop MB, Rosenberg AG. Arthroplasty with a composite of an allograft and a prosthesis for knees with severe deficiency of bone.J Bone Joint Surg [Am] 1995; 77-A: 373–386.
- Brand MG, Daley RJ, Ewald FC, Scott RD. Tibial tray augmentation with modular metal wedges for tibial bone stock deficiency. Clin Orthop 1989; 248:71–79.
- Elia EA, Lotke PA. Results of revision total knee arthroplasty associated with significant bone loss. Clin Orthop 1991; 271:114–121.
- Engh GA, Ammeen D. Results of total knee arthroplasty with medial epicondylarosteotomy to correct varus deformity. Clin Orthop 1999; 367:141–148.
- Fipp GJ. A bone grafting technique in reconstructive joint arthroplasty. J Arthroplasty 1989; 4:285–287.
- Ritter MA, Keating EM, Faris PM. Screw and cement fixation of large defects intotal knee arthroplasty: a sequel. J Arthroplasty 1993; 8: 63–65.
- Murray PB, Rand JA, Hanssen AD. Cemented long-stem revision total knee arthroplasty. Clin Orthop 1994; 309:116–123.
- Partington PF, Sawhney J, Rorabeck CH, Barrack RL, Moore J. Joint line restoration after revision total knee arthroplasty. Clin Orthop 1999; 367:165–171.
- Harada Y, Wevers HW, Cooke TD. Distribution of bone strength in the proximal tibia. J Arthroplasty 1988; 3:167–175.
- Dorr LD, Ranawat CS, Sculco TA, McKaskill B, Orisek BS. Bone graft for tibial defects in total knee arthroplasty. Clin Orthop 1986; 205:153–165.
- Brooks PJ, Walker PS, Scott RD. Tibial component fixation in deficient tibial bone stock. Clin Orthop 1984; 184:302–308.
- Hoeffel DP, Rubash HE. Revision total knee arthroplasty: current rationale and techniques for femoral component revision. Clin Orthop 2000; 380:116–132.
- Windsor RE, Insall JN, Sculco TP. Bone grafting of tibial defects in primary and revision total knee arthroplasty. Clin Orthop 1986; 205:132–137.
- Chen F, Krackow KA. Management of tibial defects in total knee arthroplasty: a biomechanical study. Clin Orthop 1994; 305: 249–257.
- Laskin RS. Total knee arthroplasty in the presence of large bony defects of the tibia and marked knee instability. Clin Orthop 1989; 248:66–70.