Information
Journal Policies
Treatment of Talar Body Fractures with Closed Reduction and Percutaneous Fixation
Reda Hussein ElKady1*,Mohammed AbdelFattahSebae1
Copyright : © 2017 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Fractures of the talus have a relatively low incidence accounting for 0.3% of all bone fractures and 3–6% of all foot fractures. These injuries affect the neck of the talus, more than the head or the body. Talar body fractures of the talus are uncommon accounting for 7–38% of all talus fractures.
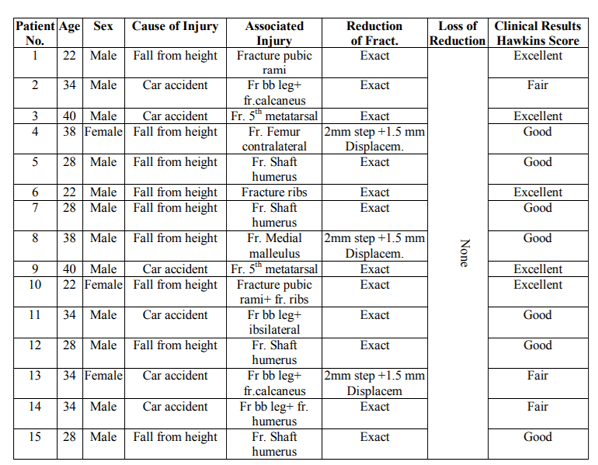
Patients and Methods: Fifteen patients with fracture of the talus were operated on using closed reduction and percutaneous screws fixation. The patients (Table 1) were followed up for an average of 20 months (range 12-30 months). In 12 patients the talar fracture was an isolated fracture of the talus in the foot and ankle region. Patient no. 2 had ipsilateral fractures of the distal tibia, fibula, and calcaneus. Patient no. 7 suffered from ipsilateral fracture of the fifth metatarsal. Patient 4 had ipsilateral medial malleolus fracture.
Results: Radiographic evaluation postoperative showed exact reduction in all cases but three which had a step of 2mm and 1.5 mm displacement. There were no re-displacements of the fractures, and all patients achieved union radiologically and clinically and could walk without external aid with full weight bearing by third to sixth month postoperative. Functional results according to Hawkins were excellent in five patients, good in seven, fair in three, and no poor results.
Conclusion: Closed reduction and percutaneous fixation of talar body fractures is a good technique with accepted clinical and radiological results, and less complications.
Talar Body, Fractures, Percutaneous, Fixation,Orthopedics
1. Introduction
Fractures of the talus have a relatively low incidence accounting for 0.3% of all bone fractures and 3–6% of all foot fractures [1-3] .These injuries affect the neck of the talus, more than the head or the body. Talar body fractures of the talus are uncommon accounting for 7– 38% of all talus fractures [4-6]. A combined talar body fracture and medial malleolus fracture is rare. We identified only three cases of this combination without any dislocation of the talar body fragment or pilon fracture. Very few reports in literature mentioning this combination of talar body fracture dislocation and medial malleolus with pilon fracture[4,7,8].
The mechanism of injury of these fractures is not clear, but is thought to be similar to the one of talar neck and pilon fractures, dorsiflexion but with added axial compression. The axial force is transmitted through the sagittal axis of the dome of talus and usually produces comminution of the talar body or tibial pilon. The medial malleolus fracture has been attributed to a rotatory element in the complex mechanism of the talar body fractures[5,8].
Sneppen et al.[6]classified talar body fractures into five groups: 1. Compression injuries; 2) Shear fracture (coronal, sagittal or horizontal); 3) Posterior process fracture; 4) Lateral process fracture; 5) Crush fracture. Sneppen et al reported the largest series of talar fracture, and recommended anatomical reduction and rigid internal fixation, wherever possible. If the talar body fracture cannot be completely exposed, a medial malleolar osteotomy gives much better access. Osteonecrosis may be less likely to occur when fracture of the talus is accompanied by a fracture of the malleolus, which preserves the soft tissue attachments to the talar body fragment[6].
Avascular necrosis of talar body represents a specific complication after talar neck and body fractures resulting from interruption of the blood supply from the sinus tarsi and tarsal tunnel at the talar neck. Even though the rates of avascular necrosis considerably differ in the literature, most studies indicate a correlation with the initial degree of dislocation and the severity of the injury. This complication is reported in about 50% after fracture dislocation of talar body [9]. Open fractures appear to bear an increased risk of avascular necrosis. Lindvall et al[10] reported an increased prevalence of post traumatic arthritis after the treatment of displaced talar fractures, which appears to be more frequent than osteonecrosis.
2. Patients And Methods
Between May 2012 and June 2017 fifteen patients with fracture of the talus were operated on using closed reduction and percutaneous screws fixation. The average follow up period was 20 months (range 12-30 months). There were 12 males, and 3 females. In 12 patients, the talar fracture was an isolated fracture of the talus in the foot and ankle region, associated injuries were remote in other limbs. The talar fractures were fixed with lag screws inserted percutaneous after closed reduction. Patient no. 2 (Fig 2) had ipsilateral fractures of the distal tibia, fibula, and calcaneus. He had an open wound associated with the tibial fracture. In this patient all fractures were fixed percutaneously using rush pin for fibula, two crossing K-wires for tibia, thick K-wire (4mm) for the calcaneus, and two lag screws for the talus. Patient no. 7(Fig 1) suffered from ipsilateral fracture of the fifth metatarsal fixed with percutaneous 2 crossing K-wires in the same setting. Patient no. 4 had ipsilateral medial malleolus fracture which was fixed with 2 lag screws, and the talar fracture was fixed with 2 K-wires inserted percutaneous after closed reduction.
Standard antero-posterior and lateral radio graphs were obtained on admission, after the operation and at regular intervals during the follow-up. The amount of displacement was measured (Table 1). Computed tomography (CT) was performed in all patients except patient no. 3. The operations were carried out in the first day in six patients with delay for 2days in other patients before arrival to hospital.
The patient was in prone position and closed reduction under image intensifier was done for all cases of isolated fracture talus in foot and ankle region, and also for the patient with ipsilateral fracture fifth metatarsal. For the other two patients they were operated on while they were in supine position. The talus was fixed first with temporary K-wires in reduced position, and then the other fractures were reduced and fixed.
The postoperative treatment was modified individually according to the patient condition, and the other injuries. Partial weight-bearing was not started before 6 weeks, and full weight-bearing was allowed after a minimum of 12 weeks depending on the radiological appearance of the talus. A plaster cast was applied in all patients for 6-10 weeks. We used the Hawkins11 method to record the final functional outcome.
3. Results
Radiographic evaluation postoperative showed exact reduction in twelve cases and in three patients there were step of 2mm and 1.5 mm displacement. There were no re-displacements of the fractures, and all patients achieved union radiologically (Figure. 3) and clinically and could walk without external aid with full weight bearing by third to sixth month postoperative. Sign of increased density in X-ray was noted in three patients, which disappeared later in follow up due to re-vascularization, but eventually no patient had avascular necrosis. There was superficial infection in patient 7 on the tibial wound, but it was controlled with IV antibiotic of third generation cephalosporin for 1week and dressing. No screw breakage or deep infection was noted in any of the patients.
Functional results according to Hawkins[11]were excellent in five patient, good in seven, fair in three, and no poor results. Twelve patients were satisfied with the results, and three patient were not satisfied as they had mild pain, and slight limping which we owed to ipsilateral fracture calcaneus, and joint arthritis.
4. Discussion
Complications in the treatment of displaced talar fractures are common due to the peculiar anatomy and function of this bone. Sixty percent of the surface of the talus is cartilage with seven articular surfaces which leaves very little space for the circulation and no muscle attachments 1.Satisfactory results have been reported in approximately 50% of patients with Hawkins type II neck fractures [9,11,12]. Gillquist et al13 reported skin problems in 10 of 13 patients treated operatively for Hawkins type II or III fractures. Lemaire and Bustin14 noted good results in all 7 of their patients, 5 type II fractures and 2 of type III. Penny and Davis 15 reported satisfactory results in only 4 of 11 of type II and 1 of 11 type III neck fractures. Pennal16 reported 8 comminuted fractures of the talar body, 3 of which were treated with early tibio-calcaneal fusion with a satisfactory result. The results of the others were poor. Sneppen et al6 reported on 17 shearing-type fractures of the talar body in their series treated mainly non-operatively. Sixteen of them had moderate or severe complaints in the follow up. Santavirta et al [17] reported 19 symptomless cases of 35 variable central talar fractures with a mean follow-up time of 8 years. Moreover, they noticed that the final clinical end result was reached at 2 years with only little or no change found in later clinical examinations.
In a series of 7 patients treated by Kankare J. and Rokkanen P.[18] with open reduction and internal fixationwith bio-degradable screws they reported that the end result of the patients after 2 years was mainly determined by the presence of injuries other than the talar fracture itself. No complications related to the intra- articular placement of these absorbable implants were detected. Moreover, the biodegradable implants produce no artifact in postoperative CT images. Thus, it would have been feasible to use magnetic resonance imaging as has previously been reported with titanium implants.
In our patients the end result was mainly determined by the presence of injuries other than the talar fracture itself. Using the closed reduction under image intensifier and percutaneous fixation technique gives little soft tissue impairment, less chances for deep infection, and preserve the vascular supply. Our patient’s clinical and functional outcome was excellent in five patients, good in seven and fair in three according to Hawkins criteria. Radiologically exact reduction was found in 12 patients, and 3 patients had step of 2 mm in the joint but we found that not affecting the final results. Union also was achieved in all patients.
5. Conclusion
Closed reduction and percutaneous fixation of talar body fractures is a good technique with accepted clinical and radiological results, and less complications.
References
- Adelaar RS:The treatment of complex fractures of the talus. orthopclin north am (1989) 20:691–707
- Coltart WD: Aviator’s astragalus. J Bone Joint Surg (1952) 34-B: 545–566.
- Kuner EH, Lindenmaier HL, Munst P:Talus fractures. In: Tscherne H, Schatzker J (eds) Major fractures of the Pilon, the Talus, and the Calcaneus: current concepts of treatment. Springer, Berlin, (1993) pp 71–85.
- Rottcher T, Lange K, Reinbold WD, Kuhn H:Sagittal burst fracture of the talus. Radiologe (1994) 34(12):759–761
- Shah K, Hakmi A:Unusual ankle injury. A case report. The Foot (2004) 14:169–172
- Sneppen O, Christensen SB, Krogsoe O:Fracture of the body of the Talus. ActaOrthopScand (1977) 48:317–324.
- Devalia KL, Ismaiel AH, Joseph G, Jesry MGH:Fourteen years follow up of an unclassified Talar body fracture with review of literature. Foot Ankle Surg (2006) 12:85–88.
- Mendonca AD, Maury AC, Makwana NK:A simultaneous fracture of the tibia and talar body. Foot Ankle Surg (2004) 10:45–47.
- Canale ST, Kelly FB:Fractures of the neck of the talus. Long-term evaluation of seventy-one cases. J Bone Joint Surg (1978) [Am] 60:143-156.
- Lindvall E, Haidukewych G, Dipasquale T, Herscovici D, Sanders R:Open reduction and stable fixation of isolated, displaced talar neck and body fractures. J Bone Joint Surg (2004) 86-A(10):2229–2234.
- Hawkins LG:Fractures of the neck of the talus. J Bone Joint Surg (1970) [Am] 52: 991-1002.
- Peterson L, Goldie IF, Irstam L:Fracture of the neck of the talus. A clinical study. ActaOrthopScand (1977) 48: 696-706.
- Gillquist J, Oretorp N, Stenstr6m A, Rieger A, Wennberg E:Late results after vertical fracture of the talus. Injury (1974) 6: 173-179.
- Lemaire RG, Bustin W:Screw fixation of fractures of the talus using a posterior approach; J Trauma (1980) 20: 669-673.
- Penny JN, Davis LA:Fractures and fracture-dislocations of the neck of the talus. J Trauma (1980) 20:1029-1037.
- Pennal GF: Fractures of the talus. Clin Orthop (1963) 30: 53-63.
- Santavirta S, Seitsalo S, Kiviluoto O, Myllynen P: Fractures of the talus. J Trauma (1984) 24: 986-989.
- Kankare J. and Rokkanen P: Dislocated fractures of the talus treated with biodegradable internal fixation; Arch Orthop Trauma Surg (1998) 117; 62-64.