Information
Journal Policies
Incurable Childhood Blindness in India: A Review
Haque OI1, Rizvi SA1, Akhtar N2, Maheshwari R3, Dr. A. Waris4*
2.Assistant professor, MS Ophthalmology, Institute of Ophthalmology, JNMCH, AMU, Aligarh
3.Professor, MS Ophthalmology, Institute of Ophthalmology, JNMCH, AMU, Aligarh
4.MS, FICO (UK), FICS (USA), FRCS (Glasg), FRCS (Edin), VR Faculty, Institute of Ophthalmology, JNMCH, AMU, Aligarh
Copyright : © 2019 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Visual impairment in childhood is a great socio-economic burden not only to the family and society but also to the nation. Early detection and prompt intervention for some of the treatable aetiologies can substantially reduce this burden. Previously thought ‘incurable’ aetiologies can also be taken care of by agile screening and newer diagnostic technologies, but it is important to first gauge the magnitude of this menace. In the west, we have conclusive data due to rigorous community screening and vigilant school programmes but in India only a few concrete studies are available. To address this problem, we are working in a tertiary hospital of North India with the aim of reviewing available data and suggesting possible strategic recommendations concerning the control of childhood blindness in India. In this review article, we discuss the available data based upon recent studies conducted in India and suggest the solutions for the control of the same.
Childhood blindness, retina, optic nerve, visual pathways, corneal scarring, Retinopathy of prematurity
1. Introduction
Control of childhood blindness is of paramount importance because a blind child suffers from more blind-years than a blind adult. Data on the number of children suffering from blindness and severe visual impairment in India and the causes of blindness are relatively crude as there are little reliable epidemiologic data. As a result, there is no organized evidence-based approach to the control of childhood blindness in India.
In 1990 the World Health Organization congregated a global workshop on childhood blindness which was held in London. This workshop highlighted the need for accurate epidemiological data on the prevalence and causes of blindness and severe visual loss in children in different parts of the world [1]. In 1993 Gilbert and colleagues developed and published a form for recording the causes of visual loss in children which has been accepted by the World Health Organization Prevention of Blindness Programme as the Standard Reporting Form for documenting the causes of childhood visual loss[2].
In 1994, a study was conducted to examine children attending blind schools in India [3]and a 1-week workshop on childhood blindness in South Asia was held at Aravind Eye Hospital for approximately 20 participants from different countries of the region[4].
2. Definition
Childhood is defined as birth to 16 years. The World Health Organization defines blindness as best corrected visual acuity in the better eye of less than 3/60, and severe visual impairment as best corrected visual acuity in the better eye of less than 6/60 but equal to, or better than 3/60.
3. Magnitude
A study by Gilbert and Foster shows that the prevalence of blindness in children varies according to socioeconomic development and under-5 mortality rates. In low-income countries with high under-5 mortality rates, the prevalence of childhood blindness may be as high as 1.5 per 1000 children, while in high-income countries with low under-5 mortality rates, the prevalence is around 0.3 per 1000 children. If this correlation is used to estimate the prevalence of blindness in children, the number of blind children in the world is approximately 1.4 million. About three-fourths of the world’s blind children live in the poorest regions of Africa and Asia[5]. Estimated National Prevalence of Childhood Blindness /Low Vision in India is 0.80 per thousand[6].
4. Causes
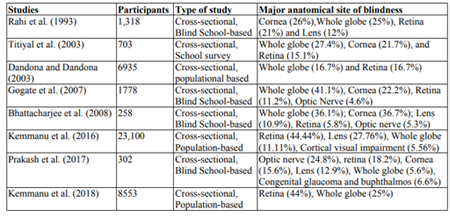
Rahi et al. (1993) examined 1,318 children with severe visual impairment or blindness in 22 schools for the blind in 9 states of India. The major causes of childhood blindness were corneal scar (26%), anomalies of the globe (25%), diseases of the retina (21%) and cataract (12%). Hereditary factors accounted for 23% of the causes of childhood blindness and postnatal factors for 28 %. in their study severely visually impaired or blind (SVI/BL) in 1318 blind school students in nine states and found that Retinal dystrophies and albinism accounted for 19.3% of the cases[3].
Titiyal et al. (2003) studied a total of 703 students less than or equal to 16 years age in 13 schools for the blind in Delhi and analyzed the causes for the 650 children who were SVI/BL after refraction. The whole globe (27.4%), cornea (21.7%), and retina (15.1%) were found to be the most frequently affected sites of abnormality [7]
Dandona and Dandona 2003, studied 6935 children ≤15 years of age and found that 50% of the blindness was due to causes that are currently not treatable or preventable, which included congenital eye anomalies (16.7%) and retinal degeneration (16.7%)[8].
Gogate et al. (2007), conducted a study of children attending special schools for blind children in Maharashtra and found that congenital anomalies accounted for 41% of which retinal disorders accounted for 11.2% of the cases of blindness, which was higher than in a similar study conducted 10 years ago[9].
Bhattacharjee et al. (2008), in their study of schools for the blind in the northeastern states of India, found that retina (5.8%) optic nerve (5.4%) are amongst the most affected anatomical sites of visual loss[10].
Kemmanu et al. (2016) conducted a population-based, cross-sectional survey of children in three phases in Pavagada and Madhugiri taluks (subdivisions) of Tumkur district in the state of Karnataka, India. In the first phase, trained fieldworkers screened 23,100 children. In the second phase, children with eye diseases were referred to the peripheral hospital to be examined by a general ophthalmologist. In the third phase, children with major eye diseases were examined by a pediatric ophthalmologist. They concluded that nearly half of the blindness in the population was due to retinal causes [11].
Prakash et al. (2017), in their study, observed that among the anatomical causes of blindness, the optic nerve was found to be the affected site in 24.8% cases, whereas retinal disorders were seen in 18.2% together which accounted for 43.0% of the cases[12].
Kemmanu et al. (2018) examined 8553 children and amongst the most common anatomical sites for SVI/blindness were retina (44%), whole-globe anomalies (25%) and uveal coloboma (25%)[13]
The table below summarizes various studies conducted in India. We can see that over the past few decades the pattern of childhood blindness is changing and retina, optic nerve, and higher visual pathways are now emerging to be major sites of visual impairment.
5. Control
The incidence of diseases like Retinopathy of prematurity, toxoplasma retinochoroiditis, congenital rubella syndrome (CRS) can be minimized by good antenatal care services like prevention of preterm births, nutritional supplementation, immunization, identification and treatment of sexually transmitted infections, providing good post-natal care to preterm and low birth weight (LBW) babies. Adequate post-natal care is crucial for the early diagnosis and management of ROP.
Genetic testing should be offered to patients with clinical findings suggestive of a Mendelian disorder whose causative gene(s) have been identified and the patient should receive counseling from a physician with expertise in inherited disease or a certified genetic counselor[14].
Recent data suggest that the prevalence of functional low vision (corrected visual acuity in the better eye ranging from < 6/18 to, and including, light perception from untreatable causes) is approximately twice the prevalence of blindness: there are almost 3 million children worldwide who have the potential to benefit from low vision care. Children with a visual acuity of less than 6/60 but equal or better than 1/60 can usually be assisted with a combination of spectacles and low vision aids (magnifiers) to read normal print. The ability to read normal print allows easier integration into normal schooling for these severely visually disabled children. Also, optic nerve atrophy and retinal dystrophy are the emerging causes of blindness. It is, therefore, essential that low vision services be part of eye care services for children at all levels of service delivery[12,15–17].
The U.S. Food and Drug Administration on December 19, 2017, approved Luxturna (voretigene neparvovec-rzyl), a new gene therapy, to treat children and adult patients with an inherited form of vision loss that may result in blindness. Luxturna is the first directly administered gene therapy approved in the U.S. that targets a disease caused by mutations in a specific gene. Luxturna is approved for the treatment of patients with confirmed biallelic RPE65 mutation-associated retinal dystrophy that leads to vision loss and may cause complete blindness in certain patients[18–20].
Retinal gene therapy clinical trials are underway for multiple genes including RPE65, ABCA4, CHM, RS1, MYO7A, CNGA3, CNGB3, ND4, and MERTK for which a molecular diagnosis may be beneficial for patients[18].
6. Conclusion
As a result of an aggressive approach towards avoidable blindness, we have been able to bring down the incidence of avoidable causes of blindness. But recent data have indicated an increased prevalence of non-avoidable blindness. In such a situation, there is an immediate need for rehabilitation programs for these children to enable them to lead a self-dependent life in the future.
In summary, it can be concluded that:
1. There are approximately 200 blind children per million total population in India.
2. The major emerging site of childhood blindness is Retina and Optic nerve, although there are marked regional variations in the pattern.
3. The provision of low vision services (by a low vision team) are necessary to enable severely visually impaired and blind children to read and write print through a combination of spectacles and magnifiers.
4. A large population-based cluster study is required with a large sample size to provide accurate data and pattern of childhood blindness.
5. Strict surveillance is required in neonatal intensive care units (NICUs) for the screening of retinopathy of prematurity as a preventable cause of childhood blindness.
7. Drawbacks
It should be noted that most data on childhood blindness in India are from school-based studies and although blind school studies are useful in identifying the major causes of childhood blindness, because a large number of children can be examined using a standard protocol by one ophthalmologist in a relatively short time, these studies suffer from selection bias. Also, blind school studies do not usually include infants andpre-school children. Children with multiple disabilities are often refused entry to blind schools and therefore causes of visual loss with other disabilities tend to be under-represented. The population-based studies are very few in number with a limited sample size so they are inadequate to represent the burden of childhood blindness in India.
References
- World Health Organization. Prevention of childhood blindness [Internet]. Geneva: Geneva: World Health Organization; 1992 [cited 2019 Jan 17]. Available from: http://apps.who.int/ iris/handle/10665/39061
- Gilbert C, Foster A, Négrel AD, Thylefors B. Childhood blindness: a new form for recording causes of visual loss in children. Bull World Health Organ 1993;71(5):485–9.
- Rahi JS, Sripathi S, Gilbert CE, Foster A. Childhood blindness in India: Causes in 1318 blind school students in nine states. Eye 1995;9(5):545–50.
- Foster A. Childhood blindness in India and Sri Lanka. Indian Journal of Ophthalmology 1996;44(1):57.
- Gilbert C, Foster A. Childhood blindness in the context of VISION 2020: the right to sight. Bull World Health Organ 2001;79:227–32.
- National Programme for Control of Blindness, Ministry of Health & Family Welfare, Government of India [Internet]. [cited 2017 Sep 17]; Available from: http://npcb.nic.in/
- Titiyal JS, Pal N, Murthy GVS, Gupta SK, Tandon R, Vajpayee RB, et al. Causes and temporal trends of blindness and severe visual impairment in children in schools for the blind in North India. Br J Ophthalmol 2003;87(8) :941–5.
- Dandona R, Dandona L. Childhood blindness in India: a population based perspective. Br J Ophthalmol 2003;87(3):263–5.
- Gogate P, Deshpande M, Sudrik S, Taras S, Kishore H, Gilbert C. Changing pattern of childhood blindness in Maharashtra, India. Br J Ophthalmol 2007;91(1):8–12.
- Bhattacharjee H, Das K, Borah RR, Guha K, Gogate P, Purukayastha S, et al. Causes of childhood blindness in the northeastern states of India. Indian J Ophthalmol 2008;56(6):495–9.
- Kemmanu V, Hegde K, Giliyar SK, Shetty BK, Kumaramanickavel G, McCarty CA. Prevalence of Childhood Blindness and Ocular Morbidity in a Rural Pediatric Population in Southern India: The Pavagada Pediatric Eye Disease Study-1. Ophthalmic Epidemiol 2016;23(3):185–92.
- Prakash MV, Sivakumar S, Dayal A, Chitra A, Subramaniam S. Ocular morbidity patterns among children in schools for the blind in Chennai. Indian Journal of Ophthalmology 2017;65(8):733.
- Kemmanu V, Giliyar SK, Shetty BK, Singh AK, Kumaramanickavel G, McCarty CA. Emerging trends in childhood blindness and ocular morbidity in India: the Pavagada Pediatric Eye Disease Study 2. Eye (Lond) 2018;32(10):1590– 8.
- Recommendations for Genetic Testing of Inherited Eye Diseases - 2014 [Internet]. American Academy of Ophthalmology2014 [cited 2018 Jan 12]; Available from: https://ww w.aao.org/clinical-statement/ recommendations-genetic-testing-of-inherited-eye-d
- al GC et. Prevalence and causes of functional low vision in school-age children: results from standardized population surveys in Asia, Africa, and Latin Amer... - PubMed - NCBI [Internet]. [cited 2018 Jan 10]; Available from: https:// www.ncbi.nlm.nih.gov/pubmed/18326706/
- Sihota, Tandon. Parsons’ Diseases of the Eye. 22 edition. Elsevier Health - INR; 2015.
- Yanoff. Ophthalmology, International Edition. 4 edition. Elsevier; 2013.
- HAFLER BP. CLINICAL PROGRESS IN INHERITED RETINAL DEGENERATIONS: GENE THERAPY CLINICAL TRIALS AND ADVANCES IN GENETIC SEQUENCING. Retina 2017;37(3):417–23.
- Commissioner O of the. Press Announcements - FDA approves novel gene therapy to treat patients with a rare form of inherited vision loss [Internet]. [cited 2018 Jan 10];Available from: https://www.fda.gov/ NewsEvents/ Newsroom/ PressAnnouncements/ucm589467.htm
- Sharif W, Sharif Z. Leber’s congenital amaurosis and the role of gene therapy in congenital retinal disorders. Int J Ophthalmol 2017;10(3):480–4.