Information
Journal Policies
Macular and Retinal Nerve Fiber Layer Analysis by Optical Coherence Tomography in Normal Children
Asmaa N. Ali1, Rania K. Farag1, Tarek A. Abd El Wahab1, Asaad A. Ghanem1*
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Aim: This study aims to evaluate macular and peripapillary retinal nerve fiber layer measurements in normal children and their correlation with age, gender, laterality, refraction and axial length.
Methods: This was an observational cross sectional study among 100 eyes of 50 child (25 boys, 25 girls) aged between 6 and 17 years. After detailed eye examination and axial length measurements, the children were scanned using swept source optical coherence tomography (3D DRI OCT Triton [plus], Topcon Corporation, Tokyo, Japan) to measure macular thickness, macular volume, peripapillary RNFL thickness and optic disc parameters.
Results: Both eyes of fifty child were included in the study. Mean age was 10.96 ± 2.75 years, average spherical equivalent refraction (SE) was 0.78±1.65 (−4.50 to +5.00) diopters and average axial length was 22.87 ± 0.90 (20.99 to 24.67) mm. Average macular thickness was 276.41±17.8 μm, central macular thickness was 225.26±20.79 μm, mean macular volume was 7.84±0.48 mm3 and mean peripapillary RNFL thickness was 111.26±20.46 μm. Axial length showed positive correlation with age unlike negative correlation with spherical equivalent. It also showed negative correlation with mean average RNFL thickness. Most of the parafoveal region quadrants correlated positively with age unlike RNFL measurements that correlated negatively. Central macular thickness values were significantly higher in males (p=0.001) but there was no difference between male and female as regard RNFL thickness. Spherical equivalent didn’t show significant effect on studied parameters. Concerning the side of the eye, it had no statistically significant difference between both eyes but good correlation.
Conclusion: Normative paediatric SS-OCT data might facilitate use of SS -OCT for assessing childhood ophthalmic diseases. This study provides a paediatric normative database of SS -OCT peripapillary RNFL and macular data.
Database – macular thickness – children – optical coherence tomography – retinal nerve fibre layer,Ophthalmology
1. Introduction
Optical coherence tomography (OCT) is a noninvasive and objective cross-sectional tissue imaging technology which has been widely used in recent years to diagnose and follow up many macular diseases, glaucoma and other optic nerve diseases[1].
Optical coherence tomography is applied by two main methods: time domain (TD-OCT) and spectral domain (SD-OCT). The advantages of SD-OCT over TD-OCT are significant improvement of the image axial resolution, decreased acquisition times, reduction of motion artifacts, increased area of retinal sampling and the possibility to create topographic maps by the three-dimensional evaluation of tissues[2].
Significant improvements in OCT technology were represented by ultrahigh resolution OCT (UHR-OCT), swept source OCT (SS-OCT), enhanced depth imaging OCT (EDI-OCT), and adaptive optics. Technological progress in OCT imaging offered new perspectives for better understanding the retinal diseases, opening new fields for clinical research[3].
Altemir et al., [4] have proved the feasibility of optical coherence tomography in the pediatric population. Compared with stereo-photography and visual field examination, peripapillary retinal nerve fiber layer thickness measurement with optical coherence tomography is particularly valuable for evaluating optic nerve damage in children[5]
For utilizing OCT information, age matched normative database will be needed to identify deviations from the normal range. Unfortunately, only limited information is available for individuals younger than 18 years of age, thus limiting its application in a pediatric population[6]
Optical coherence tomography values in children are affected by many factors such as age, gender, refraction, laterality and axial length[7]
This study was conducted to demonstrste normative values for macular thickness, macular volume and peripapillary RNFL thickness in fifty child between 6–17 years of age whom further divided into two groups from (6-10)years and from (10-17) years using DRI OCT Triton series Swept Source Optical Coherence Tomography (Topcon) and Correlated the results with biometric data.
2. Patients And Methods
This prospective observational cross-sectional and analytical study was conducted at Mansoura ophthalmic center, Mansoura University. The study protocol was approved by medical research ethics committee, faculty of medicine, Mansoura University (code number: MS/16.02.108) and informed consent was obtained from each participant in the study after assuring confidentiality. Inclusion criteria included an age from 6 to 17 years old, either genders, refractive error ± 6.00 diopters (hyperopic or myopic spherical Equivalent), astigmatism ± 3 diopters, best corrected visual acuity 0.20 logMar or better and normal Fundus.
Exclusion criteria included previous intraocular surgery or ocular injuries, Strabismus, amblyopia, anisometropia ±1.50 diopters, and retinal pathology (retinopathy of prematurity, diabetic retinopathy). Glaucoma were excluded when the IOP was >21 mm Hg. Cup disc ratio > 0.7 or difference between the two eyes > 0.2 children with history of prematurity, neurologic, metabolic or other systemic diseases (diabetes mellitus or hypertension). Media opacity does not permit optical coherence tomography acquisition with good signal strength. Optical coherence tomography scans signal strength of less than 5/10, and contraindication of pupil dilatation.
All subjects underwent an initial ophthalmic examination including measurement of the BCVA, assessment of the anterior segment of the eye using slit lamp biomicroscopy. The AL was measured three times using an optical biometer (AL-Scan, Nidek Co., Aichi, Japan) before cycloplegia, the average of three non-contac measurements was recorded. The pupils were dilated by instillation of Swixolate (Cyclopentolate Hydrochloride 10mg/ml CHEMIPHARM) eye drops three times within 30 minutes, and then the cycloplegic autorefraction was assessed. Detailed fundoscopic examination using indirect ophthalmoscope. Intraocular pressure measurement usingKeeler Pulsair intelliPuff Non-Contact Tonometer (Keeler Ltd., Windsor, Berks, UK).
Three dimensional deep range imaging OCT Triton Plus (3D DRI OCT Triton [plus], Topcon Corporation, Tokyo, Japan) with a high speed of 100,000 axial scans/s and center wavelength of 1,050 nm (version 10.07), digital and optical axial resolution of 2.6 μm and 8 μm in tissue, respectively and transverse resolution of 20 μm. The steps of OCT scanning were done as follows, the child's chin was positioned in the chin rest, and Study participants underwent SS-OCTA imaging with the following protocols. Macular map for macular thickness and macular volume: three dimensional raster scanning protocol was used, each 3D scan covered an area of 7 × 7 mm centered on the fovea with 512 A-scans × 256 B-scans 3D (H) (7.0×7.0mm-512×256). Optic disc map for Peripapillary RNFL thickness: three dimensional raster scan protocol covered an area of 6.0× 6.0 mm centered on the optic disc with 512 A-scans × 256 B-scans 3D (6.0×6.0mm-512×256). The child was asked to fix to an internal fixation light to center the scanning area (SMART Track). The OCT signal position and signal quality were automatically optimized by means of machine before acquiring OCT image. After completion of the volumetric OCT dataset, the software applied motion control technology to remove saccades and minor loss of fixation. Low-quality scans (i.e., if the child blinked or the scan had significant motion artefacts) were excluded and repeated until good-quality scans were achieved.
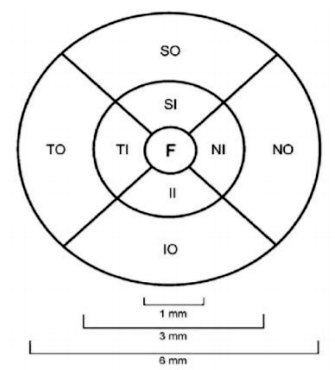
Interpretation, Macular thickness was reported in a modified Early Treatment of Diabetic Retinopathy Study (ETDRS). A 6 μm macular thickness map centered on the foveola that divided the macula into nine regions was used. It was divided into three rings, with the central ring corresponding to the fovea (1 μm diameter), the middle ring corresponding to the perifovea (2 μm diameter), and the outer ring corresponding to the parafovea (3 μm diameter) and then divided into four quadrants, namely superior, nasal, inferior and temporal except for the central circle. Central macular thickness (CMT; foveal thickness) was defined as the average macular thickness in the central 1 μm, average macular thickness was defined as the mean of thicknesses in nine regions, and macular volume was defined as the sum of volumes in all nine regions.
Peripapillary RNFL measurements, average of three measurements was taken, measurements were expressed as an average over four quadrants, 12 clock hours and mean thickness of the total circumpapillary scan. Optic nerve head parameters included disc area, cup volume, horizontal and vertical cup disc ratio and rim area.
3. Statis Tical Analys Is
Data were analyzed with Statistical Package for the Social Sciences (SPSS) version 21 (IBM corporation, Armonk, NY, USA). The normality of data was first tested with one-sample Kolmogorov-Smirnov test. Qualitative data were described using number and percent. Continuous variables were presented as mean ± SD (standard deviation). The two groups were compared with Student t test. Pearson correlation was used to correlate continuous data. Level of significance: For all above mentioned statistical tests done, the threshold of significance is fixed at 5% level (p-value). The results was considered non-significant when the probability of error is more than 5% (p > 0.05), significant when the probability of error is less than 5% (p ≤ 0.05) and highly significant when the probability of error is less than 0.1% (p ≤ 0.001). The smaller the p-value obtained, the more significant are the results.
4. Results
Data was collected and recorded at Mansoura Ophthalmic Center. A total of 100 eyes of 50 children were enrolled in the study with mean age of 10.96±2.75 ranging from 6 yrs. to17 yrs. from them 50 eyes were right and 50 eyes were left for 25 males and 25 females. The children were further divided into two groups: one group represented children from (6-10) yrs. (38%) and the other group represented children from (11-17) yrs. (62%). The best corrected visual acuity of 75 eyes of the study was (0.00) and the remaining 25 eyes had VA (0.20). Average spherical equivalent (SE) refraction was 0.78±1.65 (−4.50 to +5.00) diopters and average axial length was 22.87±0.90 (20.99-24.67) mm.
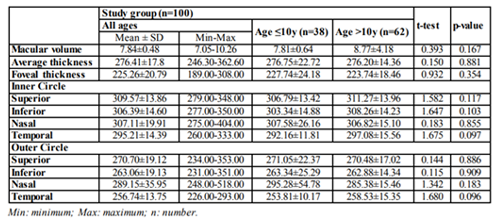
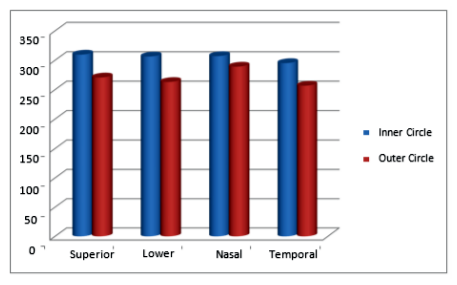
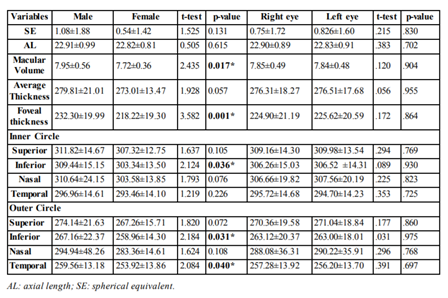
Mean central macular thickness for all children measured 225.26±20.79μm, while average macular thickness value was 276.41±17.8μm, and mean macular volume was 7.84±0.48mm3 (Table . 1). Inner circle values were significantly increased as compared to the outer macular thicknesses (p< 0.0001).
Pearson correlation was used, *Significant p-value Inner circle values were significantly increased as compared to the outer macular thicknesses (p< 0.0001) (Figure . 2).
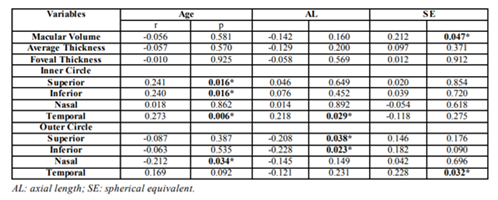
In the correlation analysis (Table . 2) of macular parameters with age there was no significant effect on macular volume, average macular thickness and central macular thickness while there was significant positive correlation between age and inner circle quadrants apart from the nasal highly significant p-value < 0.001. quadrant. The p-value was 0.016 for the superior and inferior quadrants and 0.006 for the temporal quadrant. Also age showed significant negative correlation only with the nasal quadrant of the outer circle (p-value = 0.034).
By correlating axial length with macular parameters there was no significant effect on macular volume, central macular thickness and average macular volume while it showed statistically significant positive correlation with the temporal quadrant of the parafoveal area (p-value = 0.029) and statistically significant negative correlation with the superior quadrant of perifoveal area (p-value =0.038) and the inferior quadrant of the perifoveal area (p-value=0.023).
Regarding correlation between spherical equivalent and macular parameters, macular volume and temporal quadrant of the outer circle showed significant positive correlation with spherical equivalent but other parameters did not shoe statistically significant correlation.
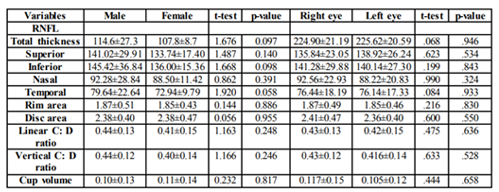
By studying the difference between male and female as regard macular parameters, male showed statistically significant higher values for macular volume, central macular thickness, inferior quadrant of the inner circle and inferior and temporal quadrant of the outer circle. However the side of the eye did not show statistically significant effect on studied parameters (Table 3).
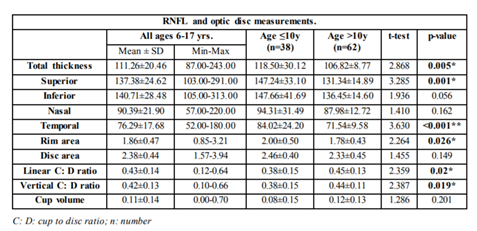
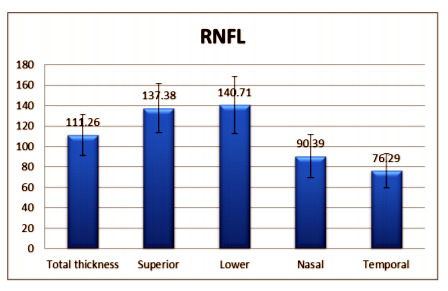
The average thickness of the RNFL was 111.26 ± 20.46 μm ranging from 87.00μm to 243.00 μm while the mean thickness of the optic disc quadrants was 137.38 ± 24.62 μm for the superior quadrant with range from 103.00 μm - 291.00 μm, 140.71 ± 28.48 μm for the lower quadrant with range from 105.00 μm to 313.00 μm, 90.39 ± 21.90 μm for the nasal quadrant with range from 57.00 μm to 220.00 μm and 76.29 ± 17.68 μm for the temporal quadrant with range from 52.00 μm to 180.00μm(Table .4).
RNFL distribution among studied group followed ISNT rule (inferior ˃ superior ˃ nasal ˃ temporal) (Figure . 3).
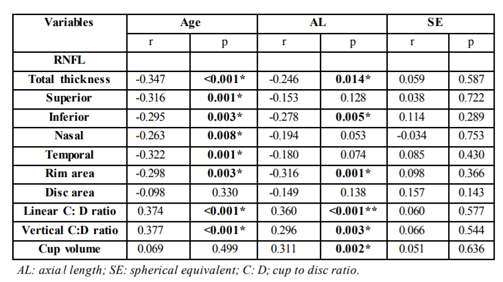
Regarding optic disc measurements, the mean of the disc area of examined children was 2.38 ± 0.44 with range from 1.57 mm² to 3.94 mm² with the mean cup volume 0.11 ± 0.14 ranging from 0.00 mm³ to 0.70 mm³. The mean of the rim area was 1.86 ± 0.47 with range from 0.85 mm² to 3.21 mm² while the mean of the vertical cup disc ratio was 0.42 ± 0.13 ranging from 0.10 to 0.66 and the mean linear cup disc ratio was 0.43 ± 0.14, which range from 0.00-0.64 By correlating RNFL thickness and optic disc parameters with age, axial length and spherical equivalent, average RNFL thickness and four quadrants thickness showed significant negative correlation with age. Linear and vertical cup disc ratio showed highly significant positive correlation with age as the p-value for both < 0.001 while the rim area shows significant negative correlation age (p-value = 0.003). Axial length there revealed significant negative correlation with total thickness (p-value = 0.014) and with the inferior sector (p-value = 0.005). It also shows significant negative correlation with rim area (p-value= 0.001), positive correlation with vertical cup disc ratio (p-value = 0.003) and cup volume (p-value = 0.002) and highly significant positive correlation with linear cup disc ratio (p-value < 0.001). Spherical equivalent showed non-significant effect on RNFL thickness and optic disc parameters (Table .5).
Regarding gender differences and interocular differences, there was no statistically significant difference between male and female and also between both sides of the eye (Table .6).
5. Discussion
Optical coherence tomography (OCT) is a noninvasive and objective cross-sectional tissue imaging device which has been widely used in modern years to detect and monitor many macular diseases, glaucoma and other optic nerve diseases[1].
The diagnosis and follow-up of children with an ocular disease is more difficult than for adults because important diagnostic tools require their cooperation. However, OCT provides fast, non- contact, objective, and reproducible measurements of the affected structures. Hence, it is an ideal diagnostic tool for use with children[9].
For utilizing OCT information, age matched normative database will be needed to identify deviations from the normal range. Unfortunately, no available normative dataset for subjects below the age of 18 years, so hinders its usage for children[6].
This study reported normative values for macular thickness, macular volume and Peripapillary RNFL thickness in fifty child between 6–17 years of age whom further divided into two groups from (6-10)years and from (10-17)years using DRI OCT Triton series Swept Source Optical Coherence Tomography (Topcon) and Correlates the results with biometric data.
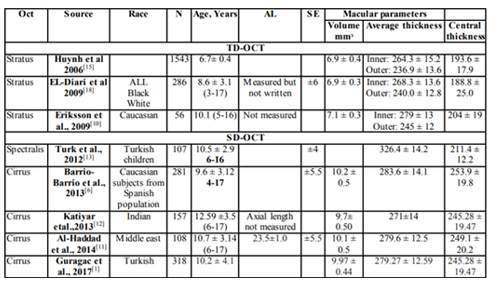
The mean macular volume in the present study was 7.84 ± 0.48 mmᶟ. This result is approximately similar to result given by Eriksson et al, [10] which was 7.1 ± 0.3 mmᶟ but lower than result given by AL-Haddad et al, [11] which was 10.1 ± 0.5 mmᶟ. This difference may be attributed to different version of OCT used (Cirrus) and different race.
Regarding average macular thickness, it was (276.41±17.8 μm) in the present study which is relatively similar to results of AL- Haddad et al,[11] as average macular thickness in their study was (279.6 ± 12.5 μm). Also similar to that detected by Gürağaç et al,[1] as they reported that average macular thickness in their study was (279.27 ± 12.59 μm).
Katiyar et al, [12] evaluated average macular thickness in Indian children aging 6-17 years by Cirrus version of OCT and found that the average macular thickness was (271±14 μm) which also approximates our result.
While these results did not coordinate with Turk et al, who reported that average macular thickness among Turkish children was (326.4 ± 14.2 μm) which is higher than the result of the current study. Regarding the mean of the central foveal thickness, it was (225.26 ± 20.79 μm) in the current study.
Turk et al,[13] evaluated the central foveal thickness in 107 eyes of Turkish children aging 6-16 years by SD-OCT (Spectralis) and found that the central foveal thickness in these children was (211.4 ± 12.2 μm). This result slightly approximates our result.
Also Barrio-Barrio et al, , [6]reported a multicenter study and evaluated the mean of the central foveal thickness among 301 Caucasian child from Spanish population by SD-OCT (Cirrus) and concluded that it was (253.9 ± 19.8 μm) which is higher than our result.
Discrepancies noted in recorded normative OCT values with other studies could be related to confounding variables like ethnicity, race, gender, age, SE and AL measurements (Table .7).
Foveal thickness in the current study was the thinnest compared by all nine quadrants. Also the nasal quadrant of the outer macular circle was the thickest which consists with convergence of retinal nerve fibers in the optic disc while the temporal quadrant was the thinnest like similar studies [1,10].
Comparison between inner and outer macular thickness values in all quadrants revealed highly statistically significant difference between both similar to results detected by Eriksson et al, and AL-Haddad et al [11].Regarding correlation of macular parameters with age in the current study we found that there was no significant correlation between age and central macular thickness. This coordinates with that reported by Molnar et al [14].In contrast to this result, AL-Haddad et al, 11reported positive correlation between age and central macular thickness.
The present study found that there was significant positive correlation between inner macular circle quadrants and age except for the nasal quadrant (did not reach statistical significance) which is similar to results given by AL-Haddad et al, [11] which also reported positive correlation between age and the thickness of inner macular circle. Katiyar et al, [12] also reported significant positive correlation between age and thickness of inner macular circle quadrants.
Regarding outer macular thickness, all quadrants showed negative correlation with age except for the temporal quadrant. But only the nasal quadrant reached statistical significance.
Katiyar et al,[12] reported positive correlation between nasal and inferior quadrants of the outer macula with age while negative correlation between superior and temporal quadrants of the outer macula with age. This does not coordinate with current study may be due to different mean of age which was 12.59 ± 3.5 yrs., different version of OCT used (Cirrus) and different refraction as they excluded any child with refractive error more than ± 0.5 D (sphere or cylinder).
Concerning correlation between gender and macular parameters, there was statistically significant increase in central thickness measurements in male over female. This result matches with that reported by Huynh et al, [15] AL-Haddad et al, [11] and Barrio-Barrio et al, 6 whom applied gender differences only on central macular thickness. Katiyar et al, [12] also found that male had higher values for central thickness than female.
In addition to that, the present study also compared between male and female from macular volume and found that male children had higher values for macular volume which correlates with that found by Qian et al, [16] whom examined Chinese children of school age.
Pokharel et al,[17] reported a study on normal eyes of Nepalese population aging from (10-37) yrs. and concluded that males have higher values for macular volume than females which coordinates with our result.
The current study also studied the correlation between axial length and average macular thickness and found no statistically significant association. This coordinates with that reported by Barrio-Barrio et al, [6]. Gürağaç et al, 1iffer from the current study as they reported that AL negatively correlates with average macular thickness.
Several studies[14] correlated spherical equivalent with central macular thickness and reported non-significant association and in the current study we also found similar result. However, macular volume in the current study showed significant positive correlation with SE. This result coordinated with that reported by AL-Haddad et al,[11] and et al, Gürağaç et al, [1] Exclusion of high refractive error might have limited our ability to assess the effect of axial length and spherical equivalent on macular parameters.
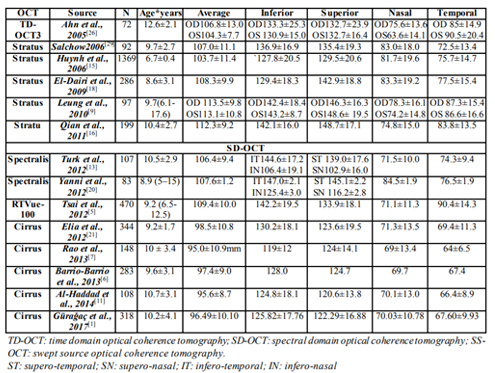
By studying the interocular difference regarding macular parameters there was no statistically significant difference between both eyes similar to results reported by Altemir et al, 4 Peripapillary RNFL Thickness Several studies have evaluated the RNFL thickness in normal children. Earlier studies used TD-OCT (OCT3-Stratus) , later SD- OCT used in measurement of RNFL thickness [1,5,11] (Table .8).
In the current study SS-OCT (Topcon) was used and it was found that the mean RNFL thickness was 111.26±20.46 μm which is similar to Qian et al, 16 (112.3±9.2 μm) , Tsai et al, [5] (109.4±10.0 μm) and Nigam et al, [19] (110.79±13) who used Stratus , RTVue and Cirrus respectively.
Turk et al,[13] and Yanni et al,[20]evaluated children between 5–16 years of age with Heidelberg Spectralis SD-OCT and reported that the mean RNFL thickness was 106.45±9.47 μm and 107.6±1.2 μm, respectively. Tsai et al, ]] evaluated 470 children aged 4 to 17 using RTVue and reported that the mean RNFL thickness was 109.4±10.0 μm. These results are slightly lower than present results.
Elía et al, [21] Barrio-Barrio et al 6 and Rao et al,[7] used cirrus and reported that the mean RNFL thickness was 98.5±10.8 μm, 95.0±10.9 μm and 97.4±9.0 μm respectively. AL-Haddad et al, [11] and Gürağaç et al, [1] also used Cirrus and reported that the mean RNFL thickness was 95. 6±8.7 μm and 96.49±10.10 μm respectively. These results are lower than current results.
The average-quadrant-wise RNFL thickness values in the current study followed the ISNT rule, it was not so for the individual eyes. The ISNT rule on the RNFL was followed by 52 eyes (52%). this result was quiet similar to another study where the ISNT rule on the NRR was followed in 30 eyes (56 %) of children between 5 and 16 years of age Larsson et al, [22]. However, this study was done on Heidelberg retinal tomography, and hence cannot be directly compared to current study.
This result is higher than Dave et al, [23] who examined children using SD-OCT and found that ISNT rule was only applicable on 30 eyes (23.8%).
The IST rule was better followed in the current study with 64 eyes (64%) obeying it. Similar results have also been found in children by Dave et al, [23] who found that 66 eyes (52.4%) obeying IST rule compared to 30 eyes (23.8%) only obeying the ISNT rule. This means that the ISNT and the IST rules for RNFL are not universally followed by all normal eyes in children. All deviations should therefore not be considered pathological.
The RNFL thickness has been considered dependent on factors such as age, AL and refraction so, the current study correlated RNFL thickness with these factors.
Regarding age, it was found that average RNFL thickness and the thickness for the four quadrants negatively correlated with age especially the average thickness as the p-value was < 0.001 unlike other studies which found that RNFL values not affected by age[6,11]. Mwanza et al, [24] have reported that the RNFL thickness decreases with age over the fifth decade in adults.
The RNFL thickness in the current study was not affected by gender similar to several studies[1,6,11,19] and different from Rao et al,[7] who reported that RNFL is thinner in female than male this may be due to different race.
Turk et al, [13]reported that significant difference between males and females only found in the temporal inferior segment (thicker in female) and no significant differences were detected in other RNFL parameters.
Axil length was negatively correlated with RNFL thickness in the present study and reached statistical significance for the average thickness and inferior quadrant thickness, this finding supported that RNFL was thinner in eyes with longer axial length. This consisted with that concluded by Savini et al, [25]. Barrio-Barrio et al,6 and Rao et al, [7]also confirmed this in their studies which evaluated children aged 4 to 17 years using Cirrus OCT. Gürağaç et al, [1] also found that negative correlation was strongest for the inferior RNFL.
On the other hand, Turk et al, [13] reported non-significant correlation between AL and RNFL thickness this may be due to different spherical equivalent, race and OCT used.
Regarding correlation between spherical equivalent and RNFL parameters we found no significant correlation between both which consisted with that concluded by Turk et al,[13] in their study on healthy Turkish children and different from AL-Haddad et al, [11] who reported strong positive correlation between SE and average RNFL but they didn’t find significant correlation with quadrant thickness similar to the current study. This may be attributed to different race and difference of SE of the excluded cases which was more than ±7D unlike more than ±6D in current study.
Regarding the side of the eye, no significant difference was detected in mean RNFL thickness of the four quadrants between right and left eyes. This results consistent with several studies[7,9,26].
Altemir et al, [4] also reported that there is no statistically significant difference between right and left eye in optic disc parameters but they reported statistically significant difference for superior, nasal and temporal quadrants of the RNFL.
Budenz et al,[27] also found no relationship between RNFL thickness and eye side in his study on 328 subjects aged 18 to 85 years. However, Gherghel et al, [28] reported that the eye side had significant influence on RNFL thickness. Difference may be attributed to using confocal scanning laser ophthalmoscopy.
Strengths of the current study include the large age range (6–17 years) of enrolled children, the use of the new generation Topcon SS-OCT, the recording of both normative RNFL and macular parameters, and the biometric correlations.
Limitations of the current study include the mostly uniform ethnic group so the effect of race and ethnicity could not be tested. We also excluded patients with high refractive errors and increased cup to disc ratios; normative data for these groups were not established. Additionally, our study was hospital based and not population-based. However, patients in this setting received a comprehensive examination and biometric data were recorded.
OCT, time domain optical coherence tomography; SD-OCT, spectral domain optical coherence tomography; SS-OCT, swept source optical coherence tomography; N, number; AL, axial length; SE, spherical equivalent.
6. Conclusion
This study established normal reference ranges for RNFL and macular parameters measured by Topcon SS-OCT in Egyptian children 6–17 years of age. This adds another database to the available literature on normative values using other OCT devices and facilitates evaluation of OCT measurements in children with optic neuropathies, glaucoma and macular diseases. The data presented are for Egyptian children; hence, other races and ethnicities should be studied in future research. Variability with age and gender axial length and refraction warrants special consideration during OCT interpretations.
References
- Gürağaç FB, Totan Y, Güler E, Tenlik A & Ertuğrul İG 2017. Normative spectral domain optical coherence tomography data in healthy Turkish children. Semin Ophthalmol, Taylor & Francis; 32: (2), 216-222.
- Major Jr JC, Wykoff CC, Mariani AF, Chen E, Croft DE & Brown DM 2014. Comparison of spectral domain and time-domain optical coherence tomography in the detection of neovascular age-related macular degeneration activity. Retina; 34: (1), 48-54.
- Medina CA, Plesec T and Singh AD 2014. Optical coherence tomography imaging of ocular and periocular tumours. Br J Ophthalmol; 98: (2), 40-46.
- Altemir I, Pueyo V, Ela N, Polo V, Larrosa JM, Oros D 2013. Reproducibility of optical coherence tomography measurements in children. Am J Ophthalmol; 155:171–176.
- Tsai DC, Huang N, Hwu JJ, Jueng RN, Chou P 2012. Estimating retinal nerve fiber layer thickness in normal school children with spectral-domain optical coherence tomography. Jpn J Ophthalmol; 56:362–370.
- Barrio‐Barrio J, Noval S, Galdós M, Ruiz‐ Canela M, Bonet E, Capote M & Lopez M 2013. Multicenter Spanish study of spectral‐ domain optical coherence tomography in normal children. Acta Ophthalmol; 91: (1).
- Rao A, Sahoo B, Kumar M, Varshney G & Kumar R 2013. Retinal nerve fiber layer thickness in children< 18 years by spectral- domain optical coherence tomography.Semin Ophthalmol, Taylor & Francis; 97-102.
- Kim MS, Kim DY, Jo YJ and Kim JY 2016. The Effect of Machine Aging on the Measurements of Optical Coherency Tomography. J Korean Ophthalmol Soc; 57: (7), 1087-1092.
- Leung, MM, Huang RY and Lam AK 2010. Retinal nerve fiber layer thickness in normal Hong Kong Chinese children measured with optical coherence tomography. J Glaucoma; 19: (2), 95-99.
- Eriksson U, Holmström G, Alm A and Larsson E 2009. A population‐based study of macular thickness in full‐term children assessed with Stratus OCT: normative data and repeatability. Acta Ophthalmol; 87: (7), 741-745.
- Al-Haddad C, Barikian A, Jaroudi M, Massoud V and Tamim H 2014. Spectral domain optical coherence tomography in children: normative data and biometric correlations. BMC Ophthalmol; 14: (1), 53.
- Katiyar V, Mugdha K, Bangwal S and Gupta SK 2013. Normative macular cirrus spectral domain optical coherence tomography data in Indian pediatric population. Egyptian Retina Journal; 1: (3), 50.
- Turk A, Ceylan OM, Arici C, Keskin S, Erdurman C, Durukan AH, Mutlu FM and Altinsoy HI 2012. Evaluation of the nerve fiber layer and macula in the eyes of healthy children using spectral-domain optical coherence tomography. Am J Ophthalmol; 153: (3), 552-559.
- Molnar A, Holmström G and Larsson E 2015. Macular thickness assessed with spectral domain OCT in a population‐based study of children: normative data, repeatability and reproducibility and comparison with time domain OCT. Acta Ophthalmol; 93: (5), 470-475.
- Huynh SC, Wang XY, Rochtchina E and Mitchell P 2006. Distribution of macular thickness by optical coherence tomography: findings from a population-based study of 6-year-old children. Invest Ophthalmol Vis Sci; 47: (6), 2351-2357.
- Qian J, Wang W, Zhang X, Wang F, Jiang Y, Wang W, Xu S, Wu Y, Su Y and Xu X 2011. Optical coherence tomography measurements of retinal nerve fiber layer thickness in chinese children and teenagers. J Glaucoma; 20: (8), 509-513.
- Pokharel A, Shrestha GS and Shrestha JB 2016. Macular thickness and macular volume measurements using spectral domain optical coherence tomography in normal Nepalese eyes. Clin Ophthalmol (Auckland, NZ); 10: 511.
- El-Dairi MA, Asrani SG, Enyedi LB and Freedman SF 2009. Optical coherence tomography in the eyes of normal children. Arch Ophthalmol; 127: (1), 50-58.
- Nigam B, Garg P and Ahmad L 2017. OCT based analysis of RNFL thickness in normal Indian paediatric population. Int J Ophthalmic Res; 3: (1), 217-219.
- Yanni SE, Wang J, Cheng CS, Locke KI, Wen Y, Birch DG and Birch EE 2013. Normative reference ranges for the retinal nerve fiber layer, macula, and retinal layer thicknesses in children. Am J Ophthalmol; 155: (2), 354-360.
- Elía N, Pueyo V, Altemir I, Oros D and Pablo LE 2012. Normal reference ranges of optical coherence tomography parameters in childhood. Br J Ophthalmol; 96: (5), 665-670.
- Larsson E, Eriksson U and Alm A 2011a. Retinal nerve fibre layer thickness in full‐term children assessed with Heidelberg retinal tomography and optical coherence tomography: normal values and interocular asymmetry. Acta Ophthalmol; 89: (2), 151-158.
- Dave P, Jethani J and Shah J 2015. Applicability of the ISNT and IST rules on retinal nerve fiber layer measurement on spectral-domain optical coherence tomography in normal Indian children. Graefe's Arch Clin Exp Ophthalmol; 253: (10), 1795-1799.
- Mwanza JC, Budenz DL, Godfrey DG, Neelakantan A, Sayyad FE, Chang RT and Lee RK 2014. Diagnostic performance of optical coherence tomography ganglion cell–inner plexiform layer thickness measurements in early glaucoma. Ophthalmology; 121: (4), 849-854.
- Savini G, Barboni P, Parisi V and Carbonelli M 2012. The influence of axial length on retinal nerve fibre layer thickness and optic-disc size measurements by spectral-domain OCT. Br J Ophthalmol; 96: (1), 57-61.
- Ahn HC, Son HW, Kim JS and Lee JH 2005. Quantitative analysis of retinal nerve fiber layer thickness of normal children and adolescents. Korean J Ophthalmol; 19: (3), 195-200.
- Budenz DL, Anderson DR, Varma R, Schuman J, Cantor L, Savell J, Greenfield DS, Patella VM, Quigley HA and Tielsch J 2007. Determinants of normal retinal nerve fiber layer thickness measured by Stratus OCT. Ophthalmology; 114: (6), 1046-1052.
- Gherghel D, Orgül S, Prünte C, Gugleta K, Lübeck P, Gekkieva M and Flammer J 2000. Interocular differences in optic disc topographic parameters in normal subjects. Curr Eye Res; 20: (4), 276-282.w
- Salchow DJ, Hutcheson KA 2007. Optical coherence tomography applications in pediatric ophthalmology. J Pediatr Ophthalmol Strabismus; 44: 335–349