Information
Journal Policies
Ocular Injuries among Adults in Owerri Municipal, Imo State, Nigeria
Ngozika Esther Ezinne1*, Khathutshelo Percy Mashige1, Awele Prisca Onianwa2
2.Department of Optometry, Madonna University, Nigeria
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Purpose: To determine the patterns of ocular injuries among adults in Owerri Municipal, Imo State, Nigeria.
Method: This was a retrospective chart review of all patients who at tended the Pizon eye clinic and Niger Optical services in Owerri Municipal, Imo State, Nigeria from January 2014 to January 2015.
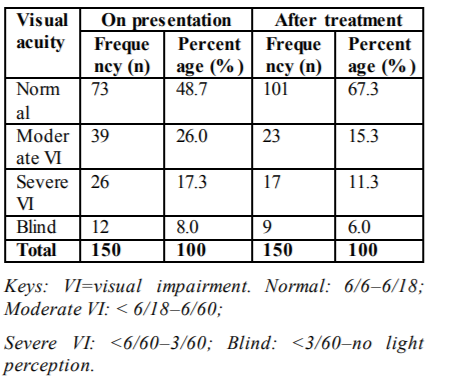
Results: Case files of 847 patients aged 21-90 years with a mean age of 37.56 ± 14.31 years were reviewed. 150 (17.7%) patients including 101 (67.3%) males and 49 (32.7%) females had ocular injuries. The major causes of ocular injuries were blunt trauma (45.3%), projectile (26%) and assault (9.3%). Contusion (54.7%) and penetrating injuries (12%) were the most common types of ocular injuries. 64 (28.7%) ocular injuries were on the conjunctiva, 42 (10.7%) on the cornea and 25 (8.7%) on the eyelids. Most (28% ) ocular injuries occurred at home, 21.3% at work places and 12.7% occurred during fights. 19 (2.7%) patients reported the injuries within 24 hours and 62 (41.3%) within 3 -7 days. 73 (48.7%) patients had visual acuity of 6/6 to 6/18 and 12 (8%) < 3/60 to no light perception on presentation and 101 (67.3%) had visual acuity of 6/6 to 6/18 and 9 (6%) 3/60 to no light perception after treatment.
Conclusion: Ocular injuries in Owerri Municipal are prevalent and their causes are largely preventable.
Ocular injuries, adults, Owerri Municipal, Imo State, Nigeria,Ophthalmology
1. Introduction
Ocular trauma was initially described as a neglected issue,[1] but has now been highlighted as a major cause of visual morbidity[2] and blindness worldwide.[3] As a cause of visual impairment, it has an immense impact on the individual, their family and the community which could lead to a variety of socioeconomic problems.[4] A review undertaken by the World Health Organization (WHO) in 1998 estimated that ocular injuries were responsible for the following: 1.6 million people blind in both eyes, 2.3 million with low vision in both eyes,19 million blind in one eye and 55 million with eye injuries that resulted in restricted activities for more than one day a year.[5] Ocular injuries also constitutes 5% of all cases admitted in hospitals in developed countries and about 12.9% in developing countries.[6] In addition, ocular injuries are common in developing countries because of issues such as non-compliance to ocular protective wear and poor working conditions among others.2 Studies[7,8] have shown that most ocular injuries can be prevented through measures such as use of protective wear at work places, home and during sporting activities that can predispose one to danger.
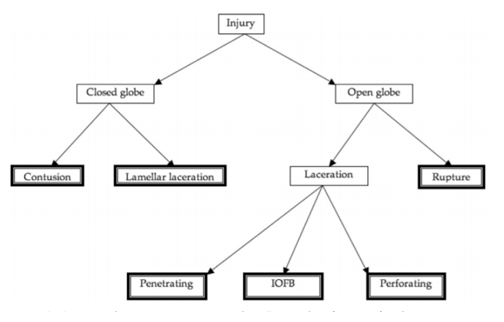
Although epidemiological data on ocular injuries has been described in the countries such as the United States[7,8] UK[9] and Australia[10], there is limited data in Africa and developing countries on this subject.[11] Ocular injury patterns including incidence and prevalence, causes and types are necessary for designing, planning and implementing preventive programmes. This study aimed to profile the patterns of ocular injuries among adults in Owerri Municipal, Imo state. Ocular injuries were classified as per World Health Organization (WHO) and Birmingham Eye Trauma Terminology System (BETTS).[9] (Figure. 1). Adnexal injuries were not included in BETTS classification. A new classification of ocular trauma was proposed in 2009 where the authors suggested that the term “ocular trauma” include structures of ocular adnexa such as the lids, orbit, lacrimal apparatus, and the conjunctival, not just the eyeball or globe[21].
2. Methods
Ethical approval to conduct this study was obtained from the Ethics Committee of the Faculty of Health Science, Madonna University, Nigeria and Clinical directors of the selected clinics in Owerri municipal. Medical records of 847 patients (aged 21 years and older) attending the selected eye clinics (Pizon eye clinic and Niger optical services) in Owerri Municipal, Imo State, Nigeria from January 2014 to January 2015 were reviewed. The records contained information on demographic characteristics, types of injuries, causes, ocular site of injury, time of injuries before presentation to the clinic, activity that led to the injury or the place where the injury occurred and visual acuities at presentation in the clinic and after treatment.
3. Data Analysis
The data obtained were imported into the Statistical Package for Social Sciences Software (SPSS) programme version 20 for analysis. Chi– square and Pearson’s correlation tests were used to investigate relationships between age, gender and occupation with type of injury. A p-value of less than 0.05 was considered statistically significant. The results were calculated in percentages and are presented in tables.
4. Results
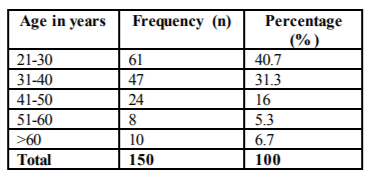
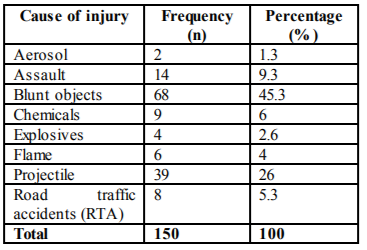
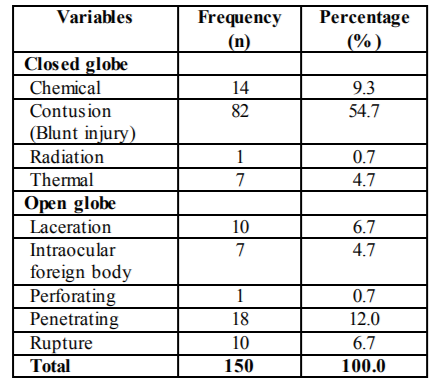
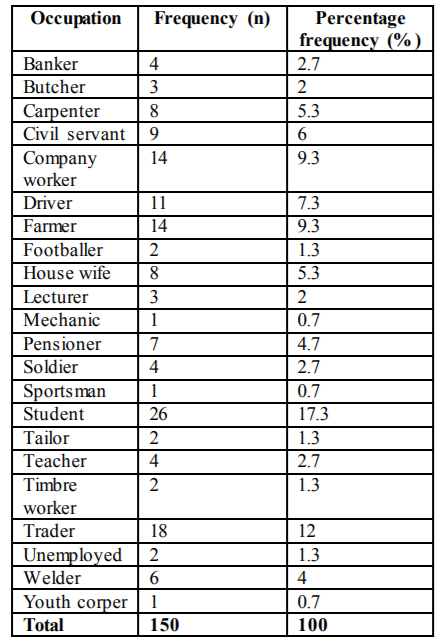
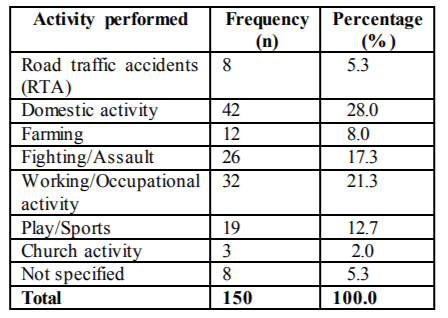
A total of 847 case files of patients aged 21 years and older with a mean age of 37.56 ± 14.3 years were reviewed. The results showed that 150 (17.7%) patients had ocular injuries. 101 (67.3%) were males and 49 (32.7%) were females. The right eye was involved in 65 (43.3%) patients, left eye in 61 (40.7%) and both eyes in 24 (16%) patients. Many (40.7%) patients with ocular injuries were between 21-30 years old followed by 31-40 years (31.3%) and 41-50 years (16%). The age distribution of the patients is shown in Table 1. The major causes of ocular injuries were blunt objects (45.3%), projectile (26%) and assault (9.3%) (Table 2). Contusion (54.7%) and penetrating injury (12%) were the most common types of ocular injuries (Table 3). There were no significant associations between age, gender and type of ocular injuries (all p-values > 0.05). Sixty four (42.7%) ocular injuries were on the conjunctiva, 42 (28%) on the cornea, 25 (16.7%) on the eyelids, 11 (7.3%) on the lens and 8 (5.3%) on the globe. Ocular injuries were found to be associated with occupation (Χ2 = 2.57, p< 0.01) and were highest in students (17.3%) followed by traders (12%) (Table 4).
Most ocular injuries occurred at home (28%) and work places (21.3%) (Table 5). 19 (2.7%) patients reported the injury within 24 hours, 40 (26.7%) within 1-3 days, 62 (41.3%) within 3-7 days (41.3%), and 29 (19.3%) after 7days. 73 (48.7%) patients had normal visual acuity (6/6 to 6/18) and 12 (8%) blind (< 3/60 to no light perception) on presentation and 101 (67.3%) had normal visual acuity and 9 (6%) blind after treatment (Table 6).
5. Discussion
Ocular injuries are among the major causes of unilateral and bilateral blindness in the working age population in developing countries, yet the types, mechanism and causes of these injuries are not fully reported.[2] Causes, types and prevalence of ocular injuries vary across countries, locations within a country and times due to differences in factors such as environmental and socioeconomic[12].
The prevalence of ocular injuries found in the current study is 17.7% which is markedly higher than 1.8% and 4.1% found in other hospital-based studies in Zaria[13] and South-South, Nigeria[14]respectively. The prevalence is more comparable to 16% reported in a study in Enugu State, Nigeria.[15] These differences may be attributed largely to the differences in age ranges and duration of review periods used. For example, studies in Zaria and South-South Nigeria used a 2 year review period compared with the one year period used in the present study. Preventive measures such as occupational health and safety rules and regulations protecting people at risk need to be designed and implemented to reduce the incidence of ocular injuries and its consequences.
The prevalence of ocular injuries was higher in males (67.3%) than in females (32.7%).This trend was also observed in a study in Benin City, Nigeria[16] where 72% males and 28% females had ocular injuries.Various studies.[8,17,18]have also shown higher prevalence figures of eye injuries in males than females.The greater proportion of males with ocular injuries is however expected given that males tend to perform more artisan jobs compared to females and these make them more prone to ocular trauma.
There was a slight predominance of injury to the right eye (43.3%) in this study which is similar to reports by Okoye15 in Enugu, Mallika et al[19] in Malaysia, and Omolase et al20 in Owo, Nigeria. Blunt object (45.3%) was the most common cause of ocular injury followed by projectile (26%) and assault (9.3%) in this study. This is consistent with findings from North- West2 and South-West [20] of Nigeria and India[21]. However, in Ethiopia[22] Tanzania [23], Southern India[24] and other Nigeria studies, [25] sharp objects (stick and thorn) were recorded as the main cause of ocular injury. Flying particles like metallic chips were reported in Singapore26 as the main cause of eye injuries. Ocular injuries from blunt and sharp objects are blinding and need urgent attention; therefore there should be awareness campaigns aimed at educating the public on preventive measures to reduce visual impairment due to ocular injuries.
The findings that most (42.7%) ocular injuries occurred on the conjunctiva are similar to those reported in other parts of Nigeria[20] and Ethiopia[27,28] and could be due to the fact that the conjunctiva is the most exposed part of the eye. Many (40.7%) patients affected by ocular injuries in this study were between 21-30 years old. This finding is not surprising as this age group is active and is likely to engage in risky activities which may predispose them to ocular injuries. Violence, which has been reported to be prevalent in Nigeria, could also have influenced this result. Okoye15 and Omolase et al20 reported similar findings in South-West Nigeria.
A significant proportion (28%) of ocular injuries occurred at home, most (53%) resulting from use of domestic equipment and assaults (38%), a finding similar to that reported in Columbia12 However; a study in Australia10 reported 60% of the eye injuries to have occurred at the work place while in rural Nepal,[29] 32% occurred at home and 37% at work place. A study in South-Western Nigeria among the elderly reported most of the injuries to have occurred at the farm (37.2%), and home (35.9%). Preventive measures aimed at encouraging the use of protective eyewear at work place and during some domestic activities are advocated.
A high proportion (41.3%) of patients presented to the clinic between 3-7 days. These results are consistent with those reported by Ezegwui[30] in which 57 (52.7%) reported within one week in South-East Nigeria. In contrast, other studies in India and South-West Nigeria reported that the most (65%) of patients with ocular trauma presented to the clinic between 24-48 hours of the injury. Proximity to health care facility could be responsible for the variations in the time of presentations. Studies in Singapore, [26] Nepal,[29] Addis Ababa[31]and Delhi India[32] reported that the risk of blindness was 2-4 times higher among patients who presented late for injuries. Studies from other countries[13,24,27,30,32,33] also showed that late presentation was associated with poor visual outcome. Early presentation to hospitals or eye clinic for treatment is important to avoid the negative consequences of ocular trauma.
Majority of patients (67.3%) had normal visual acuity (6/6 to 6/18) after treatment.Similar findings were reported in Columbia[12] and Egypt[33] and this could be due to the type of ocular injury they had which were mostly closed globe injuries and the fact that they also presented early to hospital or clinic.
The results of this study must be considered within the context of certain limitations. For example, this was retrospective chart review involving few clinics and short study period (1 year), and therefore, the results may not be generalized to the entire population.
6. Conclusion
The prevalence of ocular injuries among adults in Owerri Municipal, Imo State is relatively high and most of the causes are avoidable. Public campaigns and health education are warranted to significantly reduce the incidence of home and work related eye injuries. Assault is a significant cause of ocular injuries and a reflection of the level of violence in our society and should be addressed by all relevant stakeholders.
References
- Titiyal GS, Prakash C, Gupta S, Joshi V. Pattern of ocular trauma in tertiary care hospital of Kumaon Region, Uttarakhand, India. J Indian Acad Forensic Med. 2013; 35:116-119.
- Adamu MD, Muhammad N. Pattern of ocular trauma in Gusau, North-West Nigeria. Niger J Ophthalmol. 2017; 25:11-13.
- Shashikala P, Sadiqulla M, Shivakumar D, Prakash K H. Profile of ocular trauma in industries -related hospital. Indian J Occup Environ Med. 2013; 17: 66–70.
- Oiticica-Barbosa M M, Kasahara N. Eye trauma in children and adolescent perspective from a developing country and validation of the ocular trauma score. J Tropic Pediatrics. 2015;61: 238–243.
- Patel D. Eye injuries: improving out practice. Comm Eye Health J. 2015; 91: 41-60.
- Thylefors B. Epidemiological patterns of ocular trauma. Aust N Z J Ophthalmol. 1992; 20:95-98.
- Macgwin G, Owsley C. Rate of eye injury in the United States. Arch Ophthalmol. 2005; 123: 970-976.
- Brophy M, Sinclair SA, Hostetler SG, Xiang H. Pediatric eye injury-related hospitalizations in the United States. Pediatrics. 2006; 117: 1263-1271.
- Khun F, Morris R, Witherspoon CD, Mester V. The Brimingham Eye Trauma Terminology System (BETTS). J Fr Opthalmol. 2004; 27:206-2010.
- McCarty CA, Fu CL, Taylor HR. Epidemiology of ocular trauma in Australia. Ophthalmology. 1999; 106:1847-1852.
- Voon LW, See J, Wong TY. Epidemiology of ocular trauma in Singapore: perspective from the emergency service of a large tertiary hospital. Eye.2001; 15: 75-81.
- Serrano JC, Chalela P, Arias JD. Epidemiology of childhood ocular trauma in a North -Eastern Columbian Region. Arch Ophthalmol. 2003; 121: 1439-1445.
- Rafindal AL, Pam VA, Chinda P, Mahmud FA. Orbital and Ocular trauma at Ahmadu Bello University Teaching Hospital, Zaria, Nigeria.Med. 2013;7: 20-23.
- Emem A, Uwemedimbuk E. Prevalence of traumatic injuries in a teaching hospital in South- South Nigeria. A two year review. Adv Trop Med Pub Health Int. 2012; 2(3):102- 108.
- Okoye OI. Eye injury requiring hospitalization in Enugu Nigeria: A one-year survey. Niger J Surg Res. 2006; 8:34-37.
- Okeigbemen VW, Kayoma DH. Pattern of Eye injuries in Children in Benin City, Nigeria. Orient J Med. 2013; 25: 19-23.
- Shoja MR, Miratashi AM. Pediatric ocular trauma. Acta Med Iran. 2006; 44: 125-130.
- Aghadoost D, Fazel MR, Aghadoost HR. Pattern of pediatric ocular trauma in Kashan. Arch Trauma Res. 2012; 1:35-37.
- Mallika PS, Tan AK, Asok T, Faisal HA, Aziz S, Intan G. Pattern of ocular trauma in Kuching, Malaysia. Malaysia Fam Phys.2009; 3:140-145.
- Omolase CO, Omolade EO, Ogunleye OT, Omolase BO, Ihemedu CO, Adeosun OA. Pattern of ocular injuries in owo, Nigeria. J Ophthal Vis Res. 2011; 6:114-118.
- Qayum S, Anjun R, Rather S. Epidemiological profile of pediatric ocular trauma in a tertiary hospital of Northern, India. Chin J Traumatol. 2018; 21: 100-103.
- Abraham DI, Vitale SI, West SI, Isseme I. Epidemiology of eye injuries in rural Tanzania. Ophthalmic Epidemiol. 1999; 6:85-94.
- Onakpoya OH, Adeoye A, Adeoti CO, Ajite K. Epidemiology of ocular trauma among the elderly in a developing country. Ophthalmic Epidemiol. 2010; 17:315-320.
- Krishnaiah S, Nirmalan PK, Shamanna BR, Srinivas M, Rao GN, Thomas R. Ocular trauma in a rural population of southern India: the Andhra Pradesh Eye Disease Study. Ophthalmology. 2006; 113:1159-1164.
- Monsudi KF, Ayanniyi AA, Olatunji OF, Abdul Fattah I. Penetrating ocular injuries in a tertiary health facility. Am J Med Sci Med. 2013; 1:66-68.
- Woo J, Sundar G. Eye injuries in Singapore-- don’t risk it. Do more. A prospective study. Annals Acad Med. 2006; 35: 706-718.
- Negussie D, Bejiga A. Ocular emergencies presenting to Menelik II Hospital. Ethiopian Med J. 2011; 49:17-24.
- Addisu Z. Pattern of ocular trauma seen in Grarbet Hospital, Butajira, Central Ethiopia. Ethiop J Health Dev. 2011; 25:150-155.
- Khatry SK, Lewis AE, Schein OD, Thapa MD, Pradhan EK, Katz J. The epidemiology of ocular trauma in rural Nepal. Brit J Ophthalmol. 2004; 88:456-460.
- Ezegwui IR. Eye injuries at Abakaliki Nigeria. Int J Ophthalmol. 2004; 4: 985-988.
- Alemayehu WH, Shahin S. Epidemiology of ocular injuries in Addis Ababa Ethiopia. J Ophthalmol East Central & Southern Afr. 2014; 1: 27-34.
- Vats S, Murthy GV, Chandra M, Gupta SK, Vashist P, Gogoi M. Epidemiological study of ocular trauma in an urban slum population in Delhi, India. Indian J Ophthalmol. 2008; 56:313-316.
- Soliman MM, Macky TA. Pattern of ocular trauma in Egypt. Graef Arch Clin & Exp Ophthalmol. 2008; 246:205-212.