Information
Journal Policies
Central Serous Chorio Retinopathy and Bilateral Occludable Angles in A Case of Idopathic Thrombocytopenic Purpura (ITP), A Case Report
Dr.Sandhya.R1,Dr.Smitha.B.R.2
2.Senior Resident, Department of Ophthalmology, ESIC MC& PGIMSR, Bangalore
Copyright : © 2017 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Idiopathic thrombocytopenic purpura (ITP) is an auto immune disease , in which anti platelet antibodies cause platelet destruction and resultant bleeding abnormalities. The first line of treatment is immunotherapy. We present a case of CSR as a consequence of treatment to ITP. 24 yr old male patient came with complaints of DOV in LE since one month. On examination he was diagnosed to have raised IOP with occludable angles. Post PI, dilated fundus showed LE CSR, which was concluded to be a consequence of oral steroid treament for ITP.Patient steroid therapy was discontinued and was started on conservative management and followed up.
Idiopathic thrombocytopenic purpura (ITP), Cental Serous Chorio Retinipathy CSCR, Occludable angles,Ophthalmology
Idiopathic thrombocytopenic purpura (ITP) is an autoimmune disease in which antibodies directed against one’s own platelets cause their peripheral destruction and splenic sequestration, resulting in a low platelet count and, occasionally, bleeding complications. It is generally considered a benign disease, and most adult patients with ITP are in otherwise good health. ITP most often manifests with petechial skin rash, bruising or mucosal bleeding. Ophthalmic involvement is exceptionally rare. The most commonly used agents for initial treatment of ITP for those who require it are glucocorticoids and intravenous immunoglobin (IVIG). Systemic treatment with corticosteroids may damage the posterior blood-retinal barrier, leading to central serous chorioretinopathy. We report a case of ITP, initially manifesting with visual complaints secondary to treatment for ITP.
Case Report
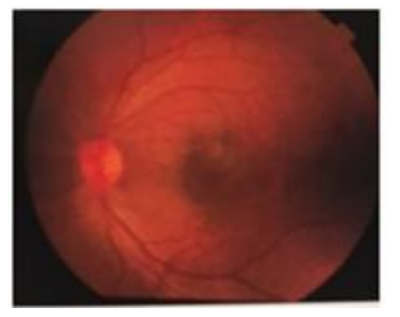
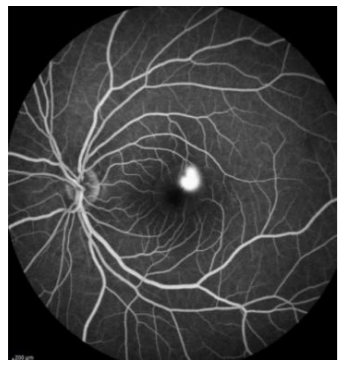
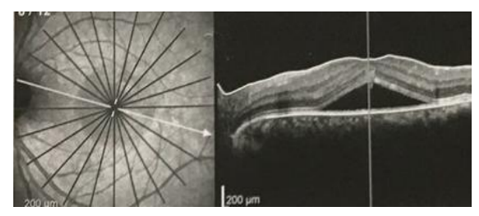
A 24 year old male presented with history of sudden painless diminution of vision in LE since 1 month. Best corrected visual acuity (BCVA) in was RE 6/6 & N6 and LE was 6/24, N36. Anterior segment examination of both eyes showed clear cornea, shallow Anterior Chamber; Van Herrick grade I –II, with normal IOP. On Gonioscopy, occludable angles were found & YAG PI was done in both eyes. Dilated fundus examination showed non specific RPE changes with mottled appearance in RE, a serous macular detachment of about 2 disc diameters in LE. FFA showed a typical ink blot pattern of hyperflourescence in the left eye and no abnormality in the right eye. HFA was within normal limits in both eyes.
On reviewing the history, he had history of fever 1 month ago with his records showed recently detected ITP while being investigated. Systemic (oral) steroids started after being diagnosed as case of ITP which was withdrawn 4-5 weeks later upon repeated recordings of high IOP.
While under our observation, the Platelet counts ranged from 15,000 to 90,000: other blood counts were within normal limits, ESR was elevated (40mm / 1st hour). Bone marrow report showed mild increase in megakaryocytes and decreased iron stores, suggestive of peripheral platelet destruction. Patient was put on Azathioprine for ITP after discontinuation of systemic steroids & Nevanac eye drops in LE and was on follow up. The BCVA on last follow up visit was 6/12(p). LE CSR had resolved and was confirmed by OCT.
Discussion
Idiopathic thrombocytopenic purpura (ITP) is an auto immune disease, in which anti platelet antibodies cause platelet destruction and resultant bleeding abnormalities. Accompanying anemia also contributes to the clinical spectrum. The reported incidence is about 100 cases in a million. The adult form of the disease is more common among females[1]. In ITP spontaneous bilateral Intra cranial hemorrhage associated vitreous hemorrhage in Terson type phenomemon is known[2]. However ophthalmic involvement is exceptionally rare. Valsalve retinopathy associated with ITP & positive anti phospholipid antibodies[3] has been reported. Spontaneous Sub conjunctival hemorrhage[4], optic tract hemorrhage[5], NAION[6] have also been noted. Thrombocytopenia alone, even severe (platelet count < 50 000), is rarely sufficient to cause significant retinal hemorrhage. However, thrombocytopenia combined with anemia is a known risk factor.
Similar hemorrhagic phenomenon involving retina & vitreous have been noted secondary to anemia in ITP[7]. CSCR is a disease characterized by serous detachment of the neurosensory retina and / or RPE. Focal leaks from the hyperpermeable choriodal vasculature results in passage of fluid through the dysfunctional RPE into the subretinal space resulting in CSCR. Type A personality[8], psychological stress[9], are known risk factors. CSCR is a well known complication of systemic steroid therapy[10]. Systemic treatment with corticosteroids may damage the posterior blood-retinal barrier, leading to CSCR and therefore the initial treatment for corticosteroid related CSCR is corticosteroid withdrawal which was done. The Diffuse RPE changes have also been attributed to systemic steroid therapy[11] .CSCR is common in mid life and commoner in men[12] .Acute ITP, with slightly higher incidence among boys is commonly seen in children (2-6 years) following viral illness, lasts for a short time, and few weeks to less than 6 months. Respiratory infections, as in this case, may precede ITP. The chronic ITP occurs later in life, is 2 to 3 times more common among female and can last from 6 months to life time[13]. CSCR is a common condition affecting the macula of young adult male. ITP & occludable angles are commoner in females. This is an unusual association of ITP, occludable angles in a young adult male presenting with CSCR. There are no reported cases of CSCR with Bilateral primary occludable angles in young adult males with ITP in literature. The CSCR can be attributed to oral steroids. Steroid response is known to cause secondary open angle glaucoma; there is no known association with primary narrow angle glaucoma. Hence detailed systemic history and treatment history is essential in cases with CSCR. Patients on systemic corticosteroid treatment for ITP must be informed about possible symptoms of central serous chorio retinopathy in order to prevent irreversible visual loss.
Conclusion
The common macular clinical entity of CSCR may be associated with other ocular & systemic comorbidities like occludable angles & ITP. Therapeutic use of oral steroids requires frequent ophthalmological monitoring, for CSCR, as in this case. The association of Primary narrow angles was unusual in this case of ITP.
Abbreviations
VA – Visual Acuity, BCVA – Best Corrected Visual Acuity, RE- Right Eye, LE- Left Eye, FFA – Fundus Fluorscein Angiography, IOP – Intra Ocular Pressure, ITP – Idiopathic Thrombocytopenic Purpura, CSCR – Cental Serous Chorio Retinipathy, OCT – Optical Coherence Tomography, RPE – Retinal Pigment Epithelium, YAG PI – YAG Peripheral Iridotomy.
References
- Cines DB, Blanchette VS. Immune thrombocytopenic purpura.N Engl J Med 2002; Mar 28; 346(13): 995-1008.
- Frankel CA, Pastore DJ, ITP with intra cranial hemorrhage and vitreous hemorrhage. ClinPediatr (Phila) 1990; 29; 725-8.
- .D.Karagiannis & Z Gregor, Eye (2006)20, 1447-1449.doi:10.1038 /sj.eye .6702313.
- Sodhi PK, Jose R., subconjunctival hemorrhage; the first presenting clinical feature of ITP. Jpn J ophthalmol 2003; 47; 316-8- 3
- Lenthall R, Gonugunta V, Jaspan.T. Pituitary apoplexy with optic tract edema & hemorrhage in a patient with ITP. Neuro radiology. 2001; 43;156-8 [PubMed]
- Killer HE, Huber A, Portman c, Forrer A, Flammer J. Bilateral non arteritic AION in a patient with auto immune thrombocytopenia. Eur J Ophthalmolo. 2000; 10: 180-2. [Pub Med].
- Majji A B , Bhatia K, Mathai A- Spontaneous bilateral peripapillary sub hyaloids & vitreous hemorrhage with severe anemia secondary to idiopathic thrombocytopenic purpura, IJO, 2010; 58: 234-236
- Yannuzzi L A. Type A behavior & central serous chorio retinopthy. Retina.1987; 111-31. Doi:10.1097/0006982-198700720 {PubMed}
- Gelber GS,Schatz H. Loss of vision due to central serous chorio retinopathy following psychological stress. Am J Psychiatry. 1987; 144:46-50. doi.:10.1176/ajp/144.1.46 [PubMed] [Cross Ref]
- Central Serous Retinopathy and Glucocorticoids Bouzas EA, Karadimas P, PournarasCJ, Survey ophthalmol. 2002 Sept-Oct; 47(5): 431-4812.
- Bettine C P Polak, G Seerp Baarsma, Bernadette Snyers, BMJ; 1995; 79; 922-925.
- Central serous chorioretinopathy, Wang M, Munch IC , Hasler PW, Prunte C, Larsen M, Acta Ophthalmolo, 2008 Mar; (2):126-45, Eupub 2001 Jul 28.
- Guide to understanding ITP, www. Itpfoundation.org.