Information
Journal Policies
Frosted Branch Angiitis - Case Report
Selegatto LT1,Batalha CP1,Alves LP1,Fonseca ALA1,Sobrinho MVA1
Copyright : © 2017 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Frosted Branch,Angiitis,Case Report,Ophthalmology
Case Report
Saia, 42 years old, male, painter.
Main Complaint: severe loss of visual acuity in both eyes for 12 hours.
He also reports violaceous skin lesions on lower limbs and polyarthritis 7 and 2 days before, respectively (the reason why cerebrospinal fluid was collected and treatment of bacterial meningitis started).
Past History: Overlapping Lupus and Sjögren Syndrome.
Systemic Treatment: azathioprine, hydroxy-chloroquine and prednisone. Ex-smoker and alcoholism.
Ocular Examination:
Visual Acuity: OD - count fingers 0,5m
OS - count fingers 0,2m.
Biomicroscopy OU: anterior chamber reaction 4+/4+.
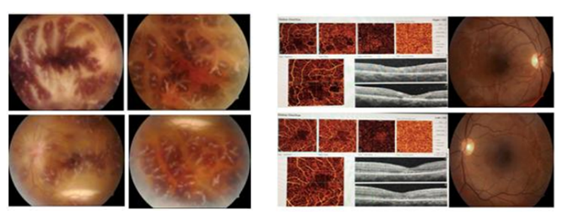
Fundoscopy OU: frosted branch angiitis and vitreous haze 2+/4+. OS: Cellular level on posterior pole (figure 1).
Management: Ceftriaxone 2g 12/12h; Oxacillin 2g 4/4h; Ganciclovir 350mg 12/2h and Dexamethasone 4mg 6/6h.
On the Following Day: severe vitreous haze.
Management: Dexamethasone 10mg 6/h; Predfort 2/2h and Mydriacyl 12/12h. Kept other medications (Ceftriaxone; Oxacillin and Ganciclovir). A skin lesion biopsy was performed – unspecific inflammatory infiltrate.
Four Months Later: visual acuity OD 20/120; OS 20/50.
SERUM SOROLOGY: Toxoplasmosis: IgG: 5,5 (reactive: >3); IgM: 0,72 (reactive: >0,6); Cytomegalovirus: IgG: >250 (reactive: >6); IgM: 0,09 (non-reactive: < 0,85). PCR: Undetectable for meningitides, streptococci, haemophilos, cytomegalovirus and herpes.
CEREBROSPINAL FLUID (CSF): Cytology: Leukocytes: 295/mm3 (0 to 3); Neutrophils: 90%, Lymphocytes: 10%; Protein: 91 (ref: 15 a 45mg/dL); Glucose: 34 (40 to 80); Bacterioscopy: Without microorganisms; Culture: negative; VDRL: negative
CSF SOROLOGY: Herpes simplex: IgM: < 0,5; IgG: < 0,5; Epstein -Barr: IgM: non-reactive; IgG: 300 (reactive); PCR: Undetectable for meningitides, streptococci, haemophilos, cytomegalovirus and herpes.
OTHER EXAMS: PCR: 6, 48; VHS: 35mm; CD4- 265; Protein/creatinine in the urine: 0.04;
Direct Coombs: negative; Anti DNA: negative; C3: 91; C4: 16; HIV: negative; VDRL negative; Hepatitis B: negative; Hepatitis C: negative.
Discussion
Frosted branch angiitis is a rare disorder (about 60 cases having been reported in the world literature) of unknown cause. It affects most children or young adults, usually bilaterally.
It is a diffuse perivasculitis, which can cause severe visual loss. There is widespread dramatic translucent sheathing of both retinal arterioles and venules, resembling the appearance of frost on a tree branch.
The cause is Unknown, has been suggested that an immune reaction may be responsible. This retinal vasculitis may also occur in association with pre-existing intraocular inflammation caused by cytomegalovirus, herpes simplex, toxoplasmosis, Behçet’s disease, systemic lupus erythematosus, leukemia, lymphoma or Crohn’s disease.
The condition probably resolves spontaneously in most cases, but responds rapidly to corticosteroids. Visual recovery may happen, with some exceptions. It is speculated that the cause of this disorder may be LUPUS inflammatory activity exacerbation (no retinal ischemic areas compatible with CMV retinal infection).
References
- Zierhut M, et al. Intraocular Inflammation. 2016, Springer-Verlag Berlin Heidelberg.
- Kleiner RC. Frosted-branch angiitis: clinical syndrome or clinical sign?. Retina 1997; 17:370–371.
- Liu IT, Chung YM, Liu JH, Hsu WM. Frosted-branch angiitis in two Chinese young girls. J Chin Med Assoc 2003; 66:501–504.
- Kleiner RC, Kaplan HJ, Shakin JL, et al. Acute frosted retinal periphlebitis. Am J Ophthalmol 1988; 106:27–34.
- Walton RC, Ashmore ED. Retinal vasculitis. Curr Opin Ophthalmol 2003; 14:413–419.
- Felipe AF, Salvosa FAM, Uy HS et al. Frosted-branch angiitis. Philipp J Ophthalmol. 2006 Jan-Jun; 31(1):39-40
- Walker S, Iguchi A, Jones NP. Frosted branch angiitis: a review. Eye (2004) 18, 527–533. Nature.