Information
Journal Policies
Clinical Performance of a New Option for Contact Lens Fitting in Corneal Ectasias in Brazil
Batalha CP1,Almeida DP1,Jorge MG1,Casagrande BPA1,Sobrinho MVA1,Selegatto LT1
Copyright : © 2017 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Clinical Performance,New Option,Contact Lens,Corneal Ectasias,Ophthalmology
1. Introdution
The cornea serves as the transparent ‘window’ of the eye that allows the entry and the refraction of light. Maintenance of cornea shape and transparency is critical for light refraction, the cornea accounting for more than two-thirds of the total refractive power of the eye and the optical properties of the cornea are determined by its transparency, surface smoothness, contour and refractive index of the tissue. Corneal ectasias, such as keratoconus and pellucid marginal degeneration, are pathological conditions that change the corneal contour and can cause loss in visual acuity[1].
Keratoconus is a Greek word (kerato: cornea; konos: cone) meaning cone-shaped protrusion of the cornea. It was first described in 1854 by Nottingham as a disease that produces corneal thinning[2] and the first contact lenses used for correction were described by Adolf Fick in 1888.[3] Keratoconus is a corneal ectatic dystrophy condition with non-inflammatory, progressive thinning and steepening of the central and / or paracentral cornea, bearing relatively normal periphery.[1,4,5] The apical protrusion causes irregular astigmatism and the apex, tapering, and disease progression leads to scarring and important loss in visual acuity.[4] It is the most common primary ectasia and it usually occurs in the second decade of life, affecting both genders and all ethnicities. The estimated prevalence in the general population is between 20-230 per 100,000.[6,5,1]
The pellucid marginal degeneration is characterized by a progressive stromal thinning of the inferior corneal segment. The term "la dystrophie marginal e infereure pellucide de la Cornee" was introduced in 1957 by Schlaeppi.[7] However, the first detailed characterization of corneal marginal degeneration pellucida (CMDP) was done by Krachmer in an article published in 1978.[8] The CMDP is a rare corneal ectasia, non-inflammatory, non-ulcer, usually bilateral, with no apparent gender preference, with no evidence of hereditary transmission and affecting individuals between 20 and 40 years old.[9] As keratoconus and ocular trauma can produce asymmetric corneal changes of difficult correction, which can be made with contact lenses.
The clinical treatment of corneal ectasia depends on the severity of the disease. In the case of keratoconus, it can be classified according to the keratometric values in: incipient, moderate, advanced and severe.[3,10] In most of cases, the visual acuity can be corrected with either glasses or contact lenses. In very advanced cases, surgery may be indicated.1 Contact lenses are one option of corneal ectasia treatment because they produce regular refractive surface, counteract aberrations and distortions of the anterior corneal surface, and improve visual acuity. The technological advances of contact lens materials and designs have allowed a good fit in almost any grade of disease severity.[11] A large amount of patients who have keratoconus are young and in economically active phase of life. This is why visual rehabilitation becomes a very important intent. In advanced stages of the disease, vision may be incompatible with work or study activities.[5,4]
The purpose of this article is to evaluate the clinical performance of a new type of contact lens for corneal ectasia.
2. Methods
We did a retrospective study of 35 patients’ charts, 55 eyes, attended at Contact Lens Clinic in Ophthalmology department of Catholic University of Campinas (PUC-Campinas), fitted with the Best Fit K contact lens (Solotica, Sao Paulo, Brazil), a contact lens with aspheric design for corneal ectasia. The adjustment method used in the clinic is trial and error, in which the adaptation starts with testing lenses that have posterior curvature equal to the base curve (K) of the patient, followed by increased curvature or diameter of the tested lens according to the adjustment obtained.
We studied the following parameters: age, sex, visual acuity with glasses, visual acuity with contact lens, base curve (BC), diameter, dioptric power (DP), average keratometry, and the diagnosis (when keratoconus: morfology and stage).
Keratoconus was classified according to the keratometry (K1) in incipient (K smaller than 45,00D in both meridians), moderate (K between 45.00 and 52,00D in both meridians), advanced (K between 52.00 and 62,00D in both meridians) and severe (K bigger than 62,00D in both meridians) In this study, when the two meridians were not in the same group, they were ranked by the steepest meridian. According to the morphology of the cone in central, oval, globus and indeterminate.[8,5,12]
3. Results
In relation to gender, there were 18 male (51.43%) and 17 female (48.57%). The age ranged from 14 to 63 years of age with an average of 33.26 years.
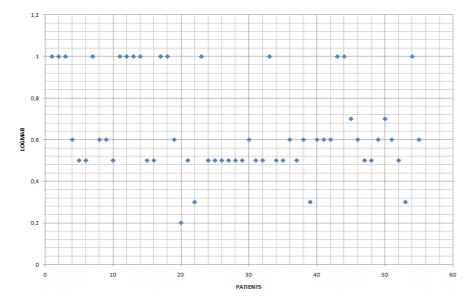
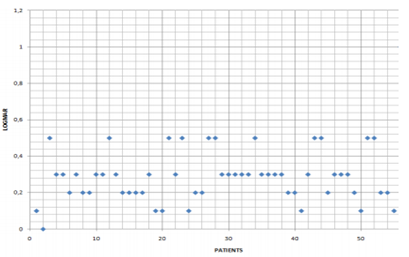
The Visual Acuity with Glasses was 0.64 LogMAR, and the Visual Acuity with Contact Lens was 0.28 LogMar. (table 1 and 2)
The mean diameter was 8.93mm, varying from 8.6 to 9.2 mm. Dioptric Power ranged from - 1.50 to -28.25 Diopters with an average of - 10.19 D. The average Base Curve of the Contact Lens was 50.33 D (47.00 to 66.50 D).
In relation of the diagnosis, the Pelucid marginal degeneration was found in one eye (1.82%), trauma in one eye (1.82%), and keratoconus in 53 eyes (96.36%).
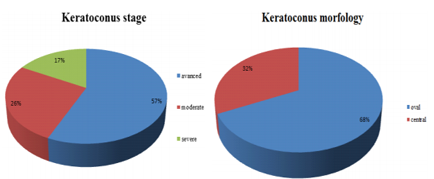
When the diagnosis was keratoconus, the morphology was oval in 36 eyes (67.92%) and central in 17 eyes (32.08%). Thirty eyes had advanced keratoconus (56.6%), 14 moderate (26.42%), and 9 (16.98%) were severe.
This new type of Contact Lens showed to be a good option for patients with corneal ectasias, trauma, and other ocular surface issues.
4. Discussion
In our study, all the 55 eyes studies reached visual acuity that was better or the same as 0.5, noting that 44 eyes reached visual acuity that was better or the same as 0.3 and 23 eyes were better of the same as 0.2. The level of acuity reached is compatible with the daily activities of most of the Brazilian population, which has been verified by the patients’ level of satisfaction at the end of the treatment.
In a study of the Department of Ophthalmology and Visual Sciences in the Escola Paulista de Medicina, involving 325 eyes, the visual acuity of patients with keratoconus with refractive reached 0.5 more or less 0.3 logMAR, and with different contact lenses (monocurve, bicurve, soft CL, multiespherical, perfect Keratoconus, MultiCurve, ultra flat) the acuity visual ranged from 0.2 more or less 0.1 logMAR.[17]
In a study published in 2006, 80 eyes were adapted with soft contact lenses World Vision Perfect Keratoconus. In this study, 45% of the eyes reached visual acuity higher than or as high as 0.1, 73 higher than 0.3 and only 7 eyes higher than 0.40 and 0.60.[14] In our study, all patients have reached visual acuity higher than or as high as 0.5.
In a work conducted at the Contact Lens Department of the Sadalla Amin Ghanem Hospital in Joinville involving 881 eyes with keratoconus, the visual acuity of contact lens’ users was of 0.2 varying between 0.0 and 1.0, noting that 86.5% of the eyes reached 0.3 or higher.[11] Regarding the evolutive aspect of keratoconus, the most advanced case was with 66.86%, similar to what was found in our work, followed by the incipient, with 18.6%.
In our study, contact lenses have been effective and provided significant improvement of visual acuity in patients with keratoconus. As the use of contact lenses are an affordable and safe method, it is of great relevance the dissemination among the patients with keratoconus, providing improved quality of life for these people.[6]
The eye diseases cause a great impact on quality of life, as a reduction of visual acuity is the major cause of disability. The quality of life has a direct influence of chronic diseases and studies suggest that patients with keratoconus have become more pessimistic, intuitive, withdrawn and insecure than the emmetropic people. The good use of contact lenses interfere positively inquality of life, making the patients more optimistic, active, outgoing, communicative and systematic than people who do not wear it.[16]
Proper contact lens fitting for these patients can even influence other aspects of the treatment. It should be noted that a large fraction of the waiting list for corneal transplant consists of keratoconus patients who have not had the opportunity to spend for contact lens adaptation test.[15]
Due to scarece literature on Best Fit K lenses and its little time in ophthalmology, it is necessary to have more follow-up time to evaluate long-term results and the eventual complications related to the chronic use of this lens.
5. Conclusion
The low visual acuity cause a social, economical and psychological harm to the patient and society.
It is worth mentioning the contribution of the Contact Lens Clinic at PUC -Campinas to patients, especially considering the low socioeconomic level of the population served and the major improvement in quality of life of patients undergoing proper contact lens fitting.
We should discuss if it is not possible for the public health system to promote appropriate demand treatment of keratoconus patients without access to the private service, considering the positive impact of this action on surgical indications in corneal ectasia, mainly cornea transplantation.[15]
Bibliography
- Krachmer JH, Mannis MJ, Holland EJ. Cornea. Fundamentals, Diagnosis and Management. Third Edition. Mosby Elsevier 2011.
- Nottingham, J. Practical observations on conical cornea. London: Churchill; 1854. p. 1-19.
- Fick AE. A contact-lens. 1888 (translation) Arch Ophthalmol. 1988; 106(10): 1373-7.
- Belfort Jr R, Kara-José N. Ceratocone. Córnea clínica e cirúrgica. São Paulo: Roca; 1997. p. 359-65
- Krachmer JH, Feder RS, Belin MW. Keratoconus and related non inflammatory corneal thinning disorders.Surv Ophthalmol. 1984; 28(4):293-322.
- Duque WP, Rehder JRCL, Leça RGC.Avaliação da eficácia na adaptação de lentes de contato com relação à melhora visual em pacientes portadores de ceratocone . Rev Bras Oftalmol. 2012; 71 (5): 313-6
- Schlaeppi V. La dystrhophie marginale inférieure pellucide de la cornée. Bibl Ophthalmol. 1957; 12(47):6727.
- Krachmer JH. Pellucid marginal corneal degeneration. Arch Ophthalmol. 1978; 96(7):1217-21.
- Maguire LJ, Klyce SD, McDonald MB, Kaufman HE. Corneal topography of pellucid marginal degeneration. Ophthalmology. 1987; 94(5):519-24.
- Rabinowitz YS, McDonnell PJ. Computer-assisted corneal topography in keratoconus. Refract Corneal Surg 1989; 5:400-8.
- Coral-Ghanem V, Coral-Ghanem C, Coral-Ghanem R, Larinho C. Ceratocone: correlação entre grau evolutivo e padrão topográfico com o tipo de lente de contato adaptada, Arq Bras Oftalmol 2003; 66:129-35
- Valbon BF, Salomão M, Isaac Ramos I, Canedo AL, Nogueira L, AmbrósioJr R. Importância da tomografia de córnea para o diagnóstico de ectasia. Rev Bras Oftalmol. 2012; 71 (5): 302-8
- Cunha MC, Lima ALH. Estudo comparativo entre pacientes adaptados com lentes de contato e pacientes com indicação de transplante de córnea. Rev Bras Oftalmol. 1997; 56(7):495-511.
- Yamazaki ES, Silva VCB, Morimitsu V, Sobrinho M, Fukushima N, Lipener C. Adaptação de lente de contato gelatinosa especial para ceratocone. Arq Bras Oftalmol. 2006; 69(4):557-60
- Schirmbeck T, Paula JS, Martin LPT, Crósio Filho H, Romão E. Eficácia e baixo custo no tratamento do ceratocone com o uso de lentes de contato rígidas gás-permeáveis. Arq Bras Oftalmol. 2005; 68(2):219-22
- Moreira LB, Alchieri JC, Belfort Jr. R, Moreira H. Aspectos psicossociais do paciente com ceratocone. Arq Bras Oftalmol. 2007; 70(2):317-22
- Lunardi LH, Arroyo D, Lipener C, Sobrinho M, Rosa JMS. Descriptive analysis of the types and parameters of contact lenses fitted in each evolutive degree and morphology of keratoconus.