Information
Journal Policies
Ocular Perfusion Pressure and Its Association with Primary Open Angle Glaucoma in Patients with Systemic Hypertension
Dr.Sandhya.R1,Dr.Fijo Kuriakose2
2.Senior Resident, Department of ophthalmology, ESIC Hospital, Udyogamandal, Ernakulam, Cochin, Kerala.
Copyright : © 2017 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Aim: To determine the association of ocular perfusion pressure with POAG in systemic hypertensive patients.
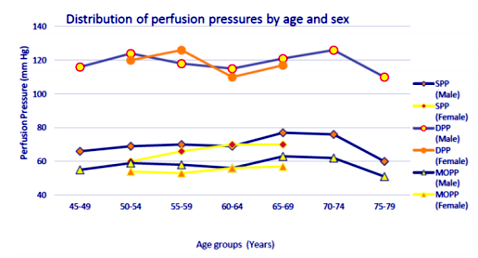
Methods: A hospital based cross sectional study was carried out to study the association of Ocular Perfusion Pressure with Primary Open Angle Glaucoma in patients with Systemic Hypertension, patients underwent complete ophthalmic examination including visual acuity, refraction, slit lamp bi-microscopy with 90D lens and gonioscopy with Goldmann three mirror lens. Systemic blood pressure was recorded by taking average of 3 readings. IOP was measured in each eye with Goldmann applanation tonometer and the median value of three measurements was taken. Visual field examination was done with Octopus/ Humphrey Field Analyzer (HFA). Mean Arterial pressure (MAP) = , Mean Ocular Perfusion Pressure (MOPP) = , Systolic perfusion pressure (SPP) =SBP-IOP, Diastolic Perfusion Pressure (DPP) =DBP-IOP were calculated.
Results: In this study 24.7% of patients with systemic hypertension had POAG.Systolic perfusion pressure was found to be positively correlated with POAG but no association was seen with Diastolic perfusion pressure. Both Systolic and Diastolic blood pressures was significantly associated with POAG and IOP was also found to be significantly associated with mean ocular perfusion pressure. However, there was no positive correlation between Glaucomatous damage and mean ocular perfusion pressure
Conclusion: Based on the results we found there was a significant association between Mean Ocular Perfusion Pressure and Intra Ocular Pressure but no association with Primary Open angle Glaucoma. Since Systemic Hypertension is a positive risk factor for development and progression of Primary Open angle Glaucoma. It is therefore fundamental to adequately control systemic hypertension in patients with primary open angle glaucoma to arrest the progression.
Ocular Perfusion,Pressure,Glaucoma,Systemic Hypertension,Ophthalmology
1. Introduction
Glaucoma is a progressive multifactorial optic neuropathy characterized with optic nerve damage, visual field loss and IOP as a modifiable risk factor. Although the mechanical effect of raised IOP on optic nerve head (ONH),[1]several vascular risk factors such as systemic hypertension, atherosclerosis, vasospasm etc., have also been implicated as potential factors capable of increasing the risk of open- angle glaucoma (OAG)[2]. The vascular hypothesis of POAG states that a low blood pressure (BP) relative to IOP can lead to low mean ocular perfusion pressure (MOPP), thus impairing vascular autoregulation of the ONH with resultant glaucomatous cupping and visual field loss [1,3].Assessment of the diurnal variations in IOP and MOPP is, therefore, clinically relevant in glaucoma patients[1,4-7].
According to American Heart Association Systemic hypertension was determined as Systolic blood pressures ≥140 mm Hg and Diastolic blood pressures ≥90 mm Hg. Long term high blood pressure, however, is a major risk factor for coronary artery disease, stroke, heart failure, peripheral vascular disease, vision loss, and chronic kidney disease.
Many studies in Baltimore[8], Bolzano[9], southern Arizona[10], and Rotterdam [11] and recently published prospective studies in Barbados [12]have shown that lower diastolic perfusion pressure (DPP), defined as diastolic blood pressure (DBP) minus IOP, is an independent risk factor for open-angle glaucoma (OAG), after adjustment for IOP and other risk factors. Clinic-based studies have further shown that non-physiologic nocturnal BP and wider circadian fluctuation in mean ocular perfusion pressure (MOPP) are significantly associated with the development and progression of OAG[13-15]. However, the relationship between perfusion pressure and glaucoma has not been well documented in Asians[16,17]. As both BP and IOP vary considerably in whites, blacks, and Asians[18], it is probable that the distribution and determinants of perfusion pressure and its relationship with glaucoma is different in Asians[19-21].
Ocular blood flow is estimated by mean ocular perfusion pressure (MOPP), conventionally defined as the difference between mean arterial blood pressure (MAP) and IOP. In view of the increasingly recognized role of vascular dysregulation in glaucoma pathogenesis, the link between MOPP and the development and progression of glaucoma is essential, as are the myriad factors that influence OPP, IOP, and MAP.
2. Materials And Methods
Seventy seven systemic hypertensive patients aged 40 years and above attending ophthalmology outpatient department in Sri Siddhartha Medical College from November 2014 to October 2016 were screened for POAG after obtaining consent. Institutional Ethical Committee approval was obtained before starting first patient enrolment.
Inclusion criteria includesall recently detected or known Systemic Hypertensive patients, Hypertensivepatients with known POAG who are on follow up, Hypertensivepatients with family history of POAGandPatients with clear media. Exclusion criteria included Diabetes mellitus, patients with corneal scarring or opacities, other causes of Optic atrophy, Secondary open angle Glaucoma, Narrow angle Glaucoma, H/o any recent intra ocular surgeries / injuriesand patients who wereon long term treatment with steroids (Systemic, topical and oral) likeUveitisand ocular inflammations.
Patients were briefly explained about the study and tests they would undergo and informed consent was obtained from all patients. A detailed ocular and medical history was taken and patients underwent complete ophthalmic examination including measurement of visual acuity, refraction, slit lamp bi-microscopy with +90D lens and gonioscopy with Goldmann three mirror lens. IOP was measured in each eye with Goldmann applanation tonometer and the median value of three measurements was taken. Visual field examination was done with Octopus/ Humphrey Field Analyzer (HFA). Systemic blood pressure was measured by random zero sphygmomanometer with the patient in sitting position. The average of three consecutive measurements of systolic and diastolic B.P was used in the analysis.Hypertension was defined as SBP≥140 mmHg/ DBP ≥90 mmHg, Mean Arterial pressure (MAP) = MOPP =, Systolic perfusion pressure (SPP) =SBP-IOP, Diastolic Perfusion Pressure (DPP) =DBP-IOP. The data obtained was entered in MS excel 2010 version, was coded and analyzed using SPSS version 11.5. Continuous variables are expressed in Mean and SD, categorical variables are expressed in Percentage. Non-parametric tests used to compare Categorical variables association was studied using chi-square test and univariate analysis. (p< 0.05 will be considered as significant).
3. Results
A total of 77 patients with systemic hypertension were included in our study. The prevalence of POAG among these patients were 24.7%.The reason for higher prevalence may be that this study was hospital based. A similar hospital based study by Smita et al39 in Northern India showed a high prevalence of POAG (33%).
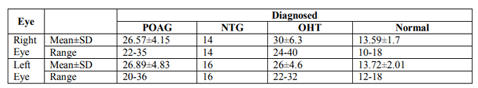
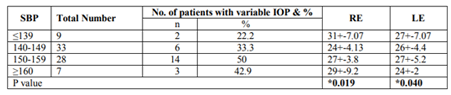
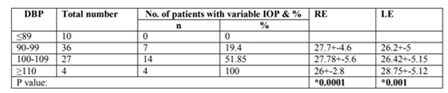
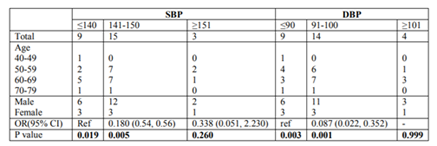
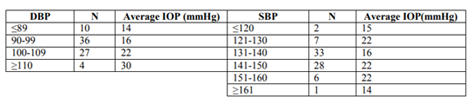
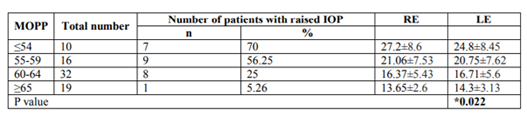
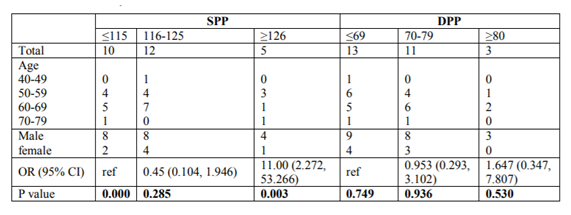
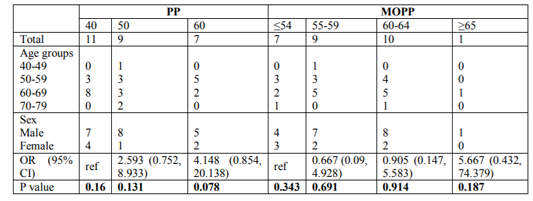
Mean Ocular perfusion pressure was found to be associated with Intra Ocular pressure. Highest no. of patients with elevated Intra Ocular pressures (>27 mm Hg &> 25 mm Hg) was seen in the lower Mean ocular pressure group (< 54 mm Hg). However, there was no significant association seen with Primary Open angle Glaucoma. Intra ocular pressure was significantly associated with systolic blood pressure and most number of patients with raised IOP was seen in the 150-159 mm Hg group.IOP was found to be strongly correlated with diastolic blood pressure and most patients with raised IOP was in the >110 mm Hg group.Intra ocular pressure increased (14mm Hg-30mm Hg) with increasing DBP. IOP did not show any such variation with SBP.Systolic blood pressure and diastolic blood pressure was found to be significantly associated with Primary open angle glaucoma. There was no significant association between pulse pressure and mean ocular perfusion pressure with POAG.There was a significant association between Systolic Perfusion pressure and POAG but no such relation was seen with Diastolic Perfusion pressure. Patients who had Systolic perfusion pressures in < 115 &>126 mm Hg groups were found to be strongly associated with Primary Open Angle Glaucoma.
4. Observations
5. Discussion
There was a positive correlation found between change in IOP and SBP, DBP and MOPP over various range.Sehi et al. had suggested that relative diurnal change in MOPP may be a risk factor for POAG[34]. The perfusion of the lamina cribrosa and NRR have been studied in various studies using scanning laser Doppler flowmeter and was found to be associated with visual field defects[35,36] .Oku et al. had found in a study that ONH ischemia is responsible for the enlargement and excavation of the disc cup with/without elevated IOP37. The circadian fluctuation of ocular perfusion pressure is responsible for the pathogenesis of glaucomatous damage. Increase in MOPP in our study, was associated with decreased Intra Ocular pressures. In other words, lower the MOPP, greater the IOP and hence greater risk of developing glaucoma. Similar results were found in various studies on ocular perfusion pressure and its relation with glaucoma. In all ocular perfusion pressure studies 24-h MOPP variation was found to be a reliable clinical risk factor in determining the severity of glaucomatous damage in patients with NTG. Sehi et al. had demonstrated in a study that the percentage decrease in diurnal MOPP was significantly larger in patients with untreated POAG than in normal subjects, suggesting that relative diurnal change in MOPP may be a risk factor for POAG[34]. Choi et al. suggested that MOPP fluctuations may be a risk factor for NTG, as reductions of OPP may lead to short-term ocular tissue ischemia, followed by reperfusion injury and consequent loss of retinal ganglion cells[38] .Similar findings of increased risk of developing glaucoma with lower diastolic, systolic or mean perfusion pressures have been reported in various other population based studies[8,9,11,12].
Blue mountain eye study and EgnaNeumarkt study showed a positive correlation between IOP and BP. In both study there was a linear rise in IOP with rise in BP levels. Klein et al in the Beaver Dam eye study observed a significant direct correlation between changes in SBP and changes in IOP.
Blue Mountain Eye study showed a positive correlation between IOP and POAG. It shows 3 mm linear rise in IOP over the spectrum of blood pressure levels. EgnaNeumarkt study also showed a positive relationship between the two and the linear rise in IOP in relation to blood pressure was about 2.5 mm Hg. Our study showed an increase of 7.36 mm Hg over that range of blood pressure Blue Mountain Eye study showed a correlation between IOP and POAG. It shows 3.2 mm linear rise in IOP over the spectrum of diastolic blood pressure levels. EgnaNeumarkt study also showed a linear rise of about 2 mm Hg. Our study showed an increase of 15.75 mm Hg over that range of blood pressure Among the 27 persons with OAG, the mean ± SD for SBP, DBP, PP, SPP, DPP and MOPP was 146.3 ± 9.26, 97.78 ± 7.51, 48.51 ± 8.18, 118.4 ±9.46, 69.5±7.81, 57.6 ±5.42 respectively. Among the 50 persons without OAG, the mean ± SD for SBP, DBP, PP, SPP, DPP and MOPP was 143.06 ± 8.95, 88.67 ± 4.01, 52.3 ± 8.85, 129.62 ± 9.02, 77.2 ± 6.93, 64.16 ± 6.40 respectively.
Lower SBP (p value -0.019 and 0.005) and DBP (p value-0.003 and 0.001) were significantly associated with OAG risk. SPP, DPP, PP and MOPP were not statistically significant (all P value > 0.05) with OAG.
The Baltimore Eye Study 22 showed a positive association between POAG and higher SBP. Patients with SBP above 130mmHg were found to have increased risk of developing POAG. A strong association between DPP < 50mmHg with the development of POAG was also noted in this study. Higher SBP and DBP are associated with increased IOP. They found a significant increase in the rates of POAG for DPP under 50.In Egna –Neumarkt study, the association was found between POAG and systemic hypertension. A positive correlation was also found between SBP and IOP[23].
Klein et al in the Beaver Dam Eye study 25 reported a 0.21 mm Hg increase in IOP for every 10 mmHg increase in SBP and 0.43 mm Hg increase in IOP for every 10 mmHg increase in DBP.Mitchel P et al in the Blue Mountain Eye Study 26 concluded that hypertension was significantly associated with OAG. Dielemans et al in Rotterdam Eye study concluded that SBP and DBP are positively associated with IOP and high tension glaucoma27. In study was carried out by Hulsman et al, no significant association was found between SBP and DBP and high tension glaucoma. An inverted association was found between low DPP and open angle glaucoma27. Pache and Flammer reported hypotension and in particular, a nocturnal drop in BP as an important risk factor for OAG[29].
Investigators from the Thessaloniki eye study reported that DBP lower than 90 mm Hg resulting from antihypertensive treatment was associated with increased cupping and a decreased rim area of the optic disc, a finding confirmed by others30. Amit K Deb showed risk reduction was higher with POAG than with glaucoma suspect. Lower the MOPP, greater the risk of developing glaucoma[31].
Tokunaga et al. showed visual field progression was evident in both the extreme dipper and the nondipper groups suggesting an underlying vascular dysregulation, and not merely nocturnal hypotension, as a contributory factor for glaucomatous damage.
The Baltimore Eye Survey identified high IOP and systemic hypertension as potential risk factors in the development of glaucomatous optic nerve damage33. Other population based studies have reported an increase in IOP ranging from 0.16 to 0.52 mm Hg with every 10 mm Hg increment in systolic pressure, and 0.35–0.52 mm Hg for every 10 mm Hg increment in DBP[22,25,32] Increased risk of developing glaucoma with lower diastolic, systolic or mean perfusion pressures have been reported in various other population based studies[22-26,28,32].
6. Conclusion
Based on the above observation and results we found a significant association between Mean Ocular Perfusion pressure and Intra ocular pressure. However, there was no positive relation with Primary Open Angle Glaucoma. These results suggest a possible role of MOPP in the pathogenesis of Glaucoma in patients on antihypertensive medications. Therefore it may be necessary to avoid administration of antihypertensive medication in known OAG patients or OAG suspects.
We also found that the prevalence of primary open angle glaucoma was significantly higher among patients with systemic hypertension. The intra ocular pressure increased with diastolic blood pressure and there was a significant association. It was also found that systolic and diastolic blood pressure was significantly associated with primary open angle glaucoma. It is therefore fundamental to adequately control systemic hypertension in patients with primary open angle glaucoma to arrest the progression of optic atrophy.
Calculation of mean OPP using theoretical formula may not reflect the real physiological status of ocular perfusion. Direct measurement of ocular blood flow could result in different outcomes. Furthermore, there can be inevitable measurement inaccuracies during assessment of BP and IOP. However due to these limitations, several large studies have shown that calculated OPP is a highly reliable parameter in glaucoma. We also agree that BP and IOP are both influenced by diurnal variations; therefore, having a single elevated/normal BP or IOP reading may not actually represent an individual's true BP or IOP status. Therefore, a study with 24 hours ambulatory BP monitoring and recording of diurnal variation of IOP and MOPP may be more appropriate. Better and continuous IOP monitoring technologies are currently emerging that can contribute significantly to the study of IOP rhythms.They may provide an invaluable tool toward a better understanding of long- and short-term IOP fluctuations.A larger sample size and a randomized control trial would be required to come to a conclusion. IOP was not corrected for central corneal thickness due to the lack of Pachymeter.
There has to be a correspondence between the physician treating hypertension and the ophthalmologist in management of primary open angle glaucoma. Routine check of intraocular pressure and hypertension together is definitely necessary to reduce the burden of inevitable blindness due to primary open angle glaucoma.
References
- Omoti AE, Enock ME, Okeigbemen VW, Akpe BA, Fuh UC. Vascular risk factors for open angle glaucoma in African eyes. Middle East Afr J Ophthalmol 2009; 16:146-50.
- Flammer J, Orgül S, Costa VP, Orzalesi N, Krieglstein GK, Serra LM, et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Res 2002; 21:359-93.
- Deokule S, Weinreb RN. Relationships among systemic blood pressure, intraocular pressure, and open-angle glaucoma. Can J Ophthalmol 2008; 43:302-7.
- Caprioli J, Coleman AL, Blood Flow in Glaucoma Discussion. Blood pressure, perfusion pressure, and glaucoma. Am J Ophthalmol 2010; 149:704-12.
- Topouzis F, Founti P. Weighing in ocular perfusion pressure in managing glaucoma. Open Ophthalmol J 2009; 3:43-5.
- Leske MC. Ocular perfusion pressure and glaucoma: Clinical trial and epidemiologic findings. CurrOpinOphthalmol 2009; 20:73-8.
- Hayreh SS. Blood flow in the optic nerve head and factors that may influence it. ProgRetin Eye Res 2001; 20:595-624.
- Tielsch JM Katz J Sommer A Quigley HA JavittJC . Hypertension, perfusion pressure, and primary open-angle glaucoma: a population-based assessment. Arch Ophthalmol. 1995; 113:216–221.
- Bonomi L Marchini G Marraffa M Bernardi P Morbio R VarottoA . Vascular risk factors for primary open angle glaucoma the Egna-Neumarkt Study. Ophthalmology. 2000; 107:1287–1293.
- Quigley HA West SK Rodriguez J Munoz B Klein R Snyder R. The prevalence of glaucoma in a population-based study of Hispanic subjects Proyecto VER. Arch Ophthalmol. 2001; 119:1819–1826.
- Hulsman CA Vingerling JR Hofman A Witteman JC de Jong PT. Blood pressure, arterial stiffness, and open-angle glaucoma: the Rotterdam study. Arch Ophthalmol. 2007; 125:805–812.
- Leske MC Wu SY Hennis A Honkanen R NemesureB. Risk factors for incident open-angle glaucoma The Barbados Eye Studies. Ophthalmology. 2008; 115:85–93.
- Deokule S WeinrebRN. Relationships among systemic blood pressure, intraocular pressure, and open-angle glaucoma. Can J Ophthalmol. 2008; 43:302–307.
- LeskeMC. Ocular perfusion pressure and glaucoma: clinical trial and epidemiologic findings. CurrOpinOphthalmol. 2009; 20:73– 78.
- Costa VP Arcieri ES Harris A. Blood pressure and glaucoma. Br J Ophthalmol. 2009; 93(10):1276–1282.
- Choi J Kim KH Jeong J Cho HS Lee CH Kook MS. Circadian fluctuation of mean ocular perfusion pressure is a consistent risk factor for normal-tension glaucoma. Invest Ophthalmol Vis Sci. 2007; 48:104–111.
- Choi J Jeong J Cho HS Kook MS. Effect of nocturnal blood pressure reduction on circadian fluctuation of mean ocular perfusion pressure: a risk factor for normal tension glaucoma. Invest Ophthalmol Vis Sci. 2006; 47:831–836.
- Xu L Wang YX Jonas JB. Ocular perfusion pressure and glaucoma: the Beijing Eye Study. Eye. 2008; 23:734–736.
- Rudnicka AR Mt-Isa S Owen CG Cook DG Ashby D. Variations in primary open-angle glaucoma prevalence by age, sex, and race: a Bayesian meta-analysis. Invest Ophthalmol Vis Sci. 2006; 47:4254–4261.
- Tielsch JM Sommer A Katz J Royall RM Quigley HA JavittJ. Racial variations in the prevalence of primary open-angle glaucoma. The Baltimore Eye Survey. JAMA. 1991; 266:369–374.
- Brown MJ. Hypertension and ethnic group. BMJ. 2006; 332:833–836.
- Tielsch JM, Katz J, Sommer A, et al. Hypertension, perfusion pressure, and primary open-angle glaucoma. A population-based assessment. Arch Ophthalmol 1995; 113:216-21.
- Bonomi L, Marchini G, Marraffa M, et al. Vascular risk factors for primary open angle glaucoma: the Egna-Neumarkt Study. Ophthalmology 2000; 107:1287-93.
- Leske MC, Connell AM, Wu SY, et al. Risk factors for open-angle glaucoma. The Barbados Eye Study. Arch Ophthalmol 1995; 113:918-24.
- Klein B K, Klein R, Knudtson M D. Intraocular pressure and systemic blood pressure: longitudinal perspective: The Beaver Dam Eye study. Br J Ophthalmol 2005; 89:284-287.
- Mitchell P, Lee AJ, Rochtchina E, Wang JJ. Open-angle glaucoma and systemic hypertension: the Blue Mountains Eye Study. Journal of Glaucoma 2004; 13: 319–26.
- Dielemans I, Vingerling JR, Algra D, et al. Primary open-angle glaucoma, intraocular pressure, and systemic blood pressure in the general elderly population: the Rotterdam Study. Ophthalmology 1995; 102:54-60.
- Hulsman C. Blood Pressure, Arterial Stiffness, and Open-angle Glaucoma. Archives of Ophthalmology. 2007; 125(6):805.
- Pache MFlammer J. A Sick Eye in a Sick Body? Systemic Findings in Patients with Primary Open-angle Glaucoma. Survey of Ophthalmology. 2006; 51(3):179-212.
- Topouzis F, Coleman A, Harris A, Jonescu-Cuypers C. Association of Blood Pressure Status With the Optic Disk Structure in Non-glaucoma Subjects: The Thessaloniki Eye Study. American Journal of Ophthalmology. 2006; 142(1):60-67.
- Deb A, Kaliaperumal S, Rao V, Sengupta S. Relationship between systemic hypertension, perfusion pressure and glaucoma: A comparative study in an adult Indian population. Indian Journal of Ophthalmology. 2014; 62(9):917.
- Memarzadeh F, Ying-Lai M, Chung J, Azen S, Varma R. Blood Pressure, Perfusion Pressure, and Open-Angle Glaucoma: The Los Angeles Latino Eye Study. Investigative Opthalmology & Visual Science. 2010; 51(6):2872.
- Sommer A, Glaucoma risk factor observed in Baltimore Eye Survey. Curr Opin Ophthalmol. 1996;7:93-8
- Sehi M, Flanagan J, Zeng L, Cook R, Trope G. Relative Change in Diurnal Mean Ocular Perfusion Pressure: A Risk Factor for the Diagnosis of Primary Open-Angle Glaucoma. Investigative Opthalmology & Visual Science. 2005; 46(2):561.
- Findl O, Rainer G, Dallinger S, Dorner G, Polak K, Kiss B, et al. Assessment of optic disk blood flow in patients with open-angle glaucoma. Am J Ophthalmol 2000; 130:589-96.
- Ciancaglini M, Carpineto P, Costagliola C, Matropasqua L. Perfusion of the optic nerve head and visual field damage in glaucomatous patients. Graefes Arch Clin Exp Ophthalmol 2001; 239:549-55.
- Oku H, Sugiyama T, Kojima S, Watanabe T, Azuma I. Experimental optic cup enlargement caused by endothelin-1-induced chronic optic nerve head ischemia. SurvOphthalmol 1999;44 Suppl 1:S74-84
- Choi J, Kim KH, Jeong J, Cho HS, Lee CH, Kook MS. Circadian fluctuation of mean ocular perfusion pressure is a consistent risk factor for normal-tension glaucoma. Invest Ophthalmol Vis Sci 2007;48:104-11
- Agarwal S. Distribution of Glaucoma in the Major Religious Communities of a North Indian Town: A Hospital Survey. Journal of Clinical and Diagnostic Research. 2013.