Information
Journal Policies
Manual Hyperinflation Plus Suctioning for Mechanically Ventilated Patients: A Review of the Literature
Nahla Shaaban Khalil1*, Manal Sayed Ismaeel2, Ahmed Mohamed Hassan Askar3, Mohamed Soliman Sayed4
2.Professor at Critical Care Nursing Department, Cairo University, Egypt.
3.Clinical instructor at Critical Care Nursing Department, Egypt.
4.Lecturer at Critical Care Medicine Department, Cairo University, Egypt.
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
In mechanically ventilated patients, airway secretions are raised due to constant positive pressure ventilation. Also, the function of existing cilia in the airway and cough reflex are weakened in these patients and inadequate and non-efficient cough in these patients results in the secretions remaining in the airway, which that lead to pneumonia and atelectasis. Obstruction of airway in a patient connected with mechanical ventilation can ultimately result in hazardous complications such as acidosis, cyanosis, cardiac dysrhythmia, and threaten the patient’s life. These complications may increase the length of ICU stay, increase mortality rate, worsen the patient outcomes, delaying patient’s recovery and increase hospital costs. Otherwise, prevention of such complications is among the care goals of these patients. To achieve this goal, endotracheal suctioning, manual hyperinflation, frequent position change, increase of physical activity, provision of adequate humidity, and fluid therapy are some of the needed nursing interventions2. Therefore, the current literature will focus in detail on the selected techniques such as manual hyperinflation and endotracheal suctioning among mechanically ventilated patients.
mechanically ventilated patients, endotracheal suctioning, manual hyperinflation, Nursing and Healthcare
1. Introduction And Background
A primary goal of mechanical ventilation is to improve arterial oxygenation, This improvement is achieved through the endotracheal intubation to ensure the delivery of oxygen to the airway and through an increase in airway pressure. Satisfactory oxygenation is easily achieved in most patients with airway obstruction. The main challenge increases in patients with alveolar-filling disorders. Ventilator is associated with a number of complications, which increase morbidity and mortality that include: mucus plugging, e.g. (atelectasis, occlusion of the endotracheal tube), ventilation-associated pneumonia (VAP) and nosocomial infection, barotrauma, e.g. (pneumothorax, subcutaneous emphysema), hypotension[11].
Pulmonary complications such as atelectasis, secretion retention and nosocomial pneumonia are common in intubated and mechanically ventilated patients, Mechanical ventilation leads to decrease functional residual capacity, increase ventilation, perfusion mismatching, decreased compliance and a reduction in surfactant[11]. Patients unable to implement respiratory functions may be need to invasive mechanical ventilation (IMV) to provide them with a ventilation and oxygenation system for adequate alveolar ventilation, restore acid-base balance and dcrease respiratory work.
These patients present different features that hinder clearance of lung secretion such as inadequate humidification, high fractions of oxygen, use of sedatives or analgesics, basal lung disease and presence of an artificial airway mechanically hanging elimination of secretion next to the trachea. Secretion retention result in episodes of hypoxemia, atelectasis and ventilator-associated pneumonia, It is believed that bronchial hygiene can improve compliance of the respiratory system through increase of dynamic compliance (Cdyn) and static compliance (Cst)[8].
There are many techniques used as nursing interventions to liquefy, mobilize and clear secretions in the airway passages for patients who have excessive secretions and ineffective cough. These techniques are performed by trained nurses in intensive care units. These technques include chest percussion, chest vibration, postural drainage techniques, and utilizing devices used independently or in combination to help in mobilizing secretions. As well, bronchodilators, humidity, and effective cough techniques before implementation of these techniques may facilitate airway clearance and improve ventilation[1].
2. Manual Hyperinflation
Manual hyperinflation (MH) known as "bagging" or "bag-squeezing" is a continuous used maneuver in critically ill intubated and mechanically ventilated patients and is routinely used by critical care nurses for the management of retained and excessive sputum.During MH, patients are disconnected from the mechanical ventilator then their lungs are temporarily ventilated with a manual ventilation bag through applying a larger-than-normal volume at a low inspiratory flow that followed by an inspiratory pause and expiration with a high expiratory flow[9], after that movement of airway secretions from the smaller toward the larger airways then allows for easy removal of airway secretions with airway suction. Also, MH could prevent airway plugging, and even promote alveolar recruitment[7]. so that, Manual hyperinflation may be important when there is a ventilator fault, or during cardiopulmonary resuscitation[3].
"Bagging," or manually ventilating a patient with a handheld resuscitation device (Ambu, VentiSure, others), is an essential nursing skill. It is vital, not only in emergencies, but also used during ventilator or artificial airway tubing changes, before and after suctioning and during transport of a patient. A manual resuscitation device has four basic parts: a nonrebreathing valve, a bag, an adapter, and a reservoir. The valve directs the flow of air or oxygen to the patient when the bag is compressed, and away from the patient and into the atmosphere during exhalation. The bag should automatically reinflate after each squeeze. The adapter allows to attach the bag to a face mask or a tracheostomy or endotracheal (ET) tube. The best adapters are the swivel type that turn 360 degrees. The reservoir helps increase the concentration of oxygen delivered to the patient. If the bag has a reservoir, it can be in the form of a hollow tube or an additional bag attached to the end of the main bag[10].
3. The Purpose Of Manual Hyperinflation
Retained airway secretions obstruct the airways of intubated and mechanically ventilated patients that lead to atelectasis. This may impair oxygenation by increased intrapulmonary shunting and increase pulmonary vascular resistance. Large atelectasis lead to lung injury. The following of large atelectasis is a smaller lung available for ventilation, leading to the concept of "baby lung" ventilation. Permanent presence of sputum in the airways can lead to an ideal environment for colonizing organisms that result in pneumonia.
Continuous removal of sputum from the airways through tracheal suctioning is mandatory in critically ill intubated and mechanically ventilated patients. at healthy persons, mucociliary transport clears the smaller airways of airway secretions. Secretions are transported from the smaller airways into the bronchi and trachea then are removed by coughing. Critically ill patients are frequently sedated and nursed in a supine position, that result in reducing mucociliary transport and promoting retention of airway secretions. also, the cough reflex can be minimal or even absent in sedated critically ill patients, or they can decrease the force to cough efficiently. Otherwise, sputum may not be easily transported from the trachea into the translaryngeal tube or trachea cannula that remain in the larger airways. Furthermore, with airway suctioning, only the trachea is cleared of secretions, as suction catheters cannot reach sputum in the bronchi and smaller airways. SO, the aim of MHI is to: optimize alveolar ventilation through reducing atelectasis, this reduces ventilation perfusion mismatch and improves gas exchange, mobilize pulmonary secretions and improve lung compliance MHI can be indicated in patients required mechanical ventilation and self-ventilating tracheostomy patients who have Chest x-ray changes of lung collapse and/or consolidation or by areas which are poorly ventilated on auscultation. The ability to monitor patients’ response is required during manual hyperinflation for Heart rate, blood pressure and oxygen saturations[4].
4. Hazards And Complications Of Manual Hyperinflation
MHI is a form of positive pressure ventilation and if performed inappropriately carries the risk of complications such as Barotrauma and volutrauma that are terms used to describe the development of extra alveolar air and fluid that result from alveolar distention. The delivery of high peak airway pressures and or volumes lead to hemodynamic instability due to the increase in intrathoracic pressure, which can decrease, stroke volume & cardiac output, change blood pressure response, and cause tachycardia.
MHI contraindicated in patients with Extra-alveolar air e.g. Bullae or Undrained Pneumothorax or Subcutaneous emphysema of unknown cause or Severe/widespread bronchospasm, so MHI not used in patients with Pneumothorax, a bubbling chest drain , Low, high or labile blood pressure, Labile ICP , Some lung diseases, especially emphysema/ hyperinflated lungs, Cardiac arrhythmias , Post Lung surgery, High PEEP requirements combined with high Fi02 requirement and PEEP > 10cmH20 on mechanical ventilation.4
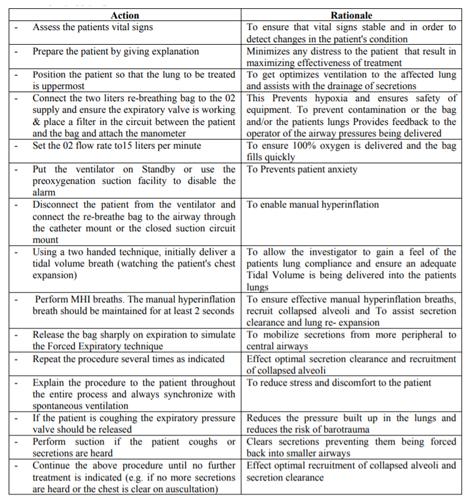
5. Procedure Of Manual Hyperinflation Technique
6. Endotracheal Suctioning (Ets)
ETS is the vital part of chest physiotherapy (CPT) and it is performed routinely in intubated patients to help in secretion removal and cough stimulation, it is a form of bronchial hygiene therapy and mechanical ventilation that involves the mechanical aspiration of pulmonary secretions to prevent the air way obstruction. ETS is usually implement every 1-2 hours or as needed to maintain airway patency and arterial oxygenation. Tracheal suctioning requires the insertion of a catheter into the upper air way where it is passed down the trachea to the level of the carina. the carina is richly innervated by the vagus nerve, when the trip of the suction, catheter comes in contact with the carina, it can provoke a strong parasympathetic response, which in turn can trigger a sudden decrease in the heart rate and produce cardiac arrhythmias, so that, the critical care nurses should monitor their patient carefully for the appearance of such events and provide supplemental oxygen during the procedure[6].
Deep suctioning is required in mechanically ventilated patients, in which the catheter is inserted until an obstruction is felt (usually the carina or wall of the right main stem bronchus), then slightly withdrawn, suction is frequently applied while the catheter is withdrawn from the airway. one of the complications of the tracheal suctioning is tracheal-laryngeal cilliary dysfunction due to irritation of the airway mucosa, the greatest mucosal damage has been noted with vacuum pressures above 120mm hg, although pressures as high as 170 mm Hg are used, the critical care nurses should use the lowest pressure as possible for removal of secretion that is effective. The procedure includes patient preparation, the suctioning event, and follow-up care, In preparation the patient for suction the critical care nurses should have base line vital signs, ABGs, SPO2 and tidal volume and asses the indications for bronchial hygiene therapy (suctioning) and CPT[6].
There are two methods of endotracheal suctioning based on the selection of catheter: open and closed. The open suctioning technique requires disconnecting the patient from the ventilator, while the closed suctioning technique involves attachment of a sterile, closed, in-line suction catheter to the ventilator circuit, which allows passage of a suction catheter through the artificial airway without disconnecting the patient from the ventilator[5].
7. Conclusion
Secretion retention continues to be a commonly challenge among mechanically ventilated patients and carries significant burdens of morbidity, mortality and cost. Studies on prevention strategies directed toward manual hyperinflation plus endotracheal suctioning have shown variable success. Routine endotracheal suction in intubated patients facilitates the removal of airway secretions, makes the airway patent and prevents chest infection. Also, apply manual hyperinflation plus endotracheal suctioningto re-expand collapsed alveoli (atelectasis), mobilize and remove excess bronchial secretions, and improve oxygenationthat consider important part of the management of patients in intensive care units. Elimination of airway secretions is one of the most significant factors that allow the successful use of ventilation support for patients with either ventilator or oxygenation impairment However, certain techniques as described in this review have been shown to improve patient outcomes and, therefore, we recommend health care providers to apply the manual hyperinflation plus suctioning as routine practice. Future research that considers clinical outcomes as primary endpoints will hopefully result in more detailed prevention strategies.
References
- Ambrosino, N., Venturelli, E., vagheggini, G., &clini, e. (2012). Rehabilitation, weaning and physical therapy strategies in chronic critically ill patients.european respiratory journal, 39(2), 487-492.
- Bousarri, m. p., shirvani, y., agha-hassan-kashani, s., &nasab, n. m. (2014). The effect of expiratory rib cage compression before endotracheal suctioning on the vital signs in patients under mechanical ventilation. iranian journal of nursing and midwifery research, 19(3), 285 : available at http://www. ncbi.nlm.nih.gov/pmc/articles/pmc4061630/
- Brooker, c., nicol, m., & alexander, m. f. (eds.). (2013). alexander's nursing practice 4: nursing the critically ill patient, chapter 29 p. 761.
- Dennis, D., Jacob, W., &Budgeon, C. (2012). Ventilator versus manual hyperinflation in clearing sputum in ventilated intensive care unit patients. Anaesthesia and intensive care, 40(1), 142.
https://search.proquest.com/openview/d98 e24c7ae9351a154b4b46b1b531048/1?pq-origsite
=gscholar&cbl=37547 - Dougherty, L., & Lister, S. (9Eds.). (2015). The Royal Marsden manual of clinical nursing procedure
- Kumar, R. (2015). Manual of ICU Procedures; respiratory procedure, Manual Chest Physiotherapy in Ventilated Patients P. 222
- Paulus, F., Binnekade, J. M., Vroom, M. B., & Schultz, M. J. (2012). Benefits and risks of manual hyperinflation in intubated and mechanically ventilated intensive care unit patients: a systematic review. Critical Care, 16(4), R145.
- Santos, f. r. a. d., schneiderjúnior, l. c., forgiarini junior, l. a., &veronezi, j. (2009). effects of manual rib-cage compression versus peep-zeep maneuver on respiratory system compliance and oxygenation in patients receiving mechanical ventilation. Revistabrasileira de terapiaintensiva, 21(2), 155-161. retrived on:
http://www.scielo.br/ scielo.php?pid= s0103507 x2009000200007 &script=sci_arttext&tlng=pt - Sheila, k. & sue, o. (2012): critical care nursing science and practice (2nd ed.): respiratory problems p. 104.
- Sally Beattie (2009) , modern medicine; baging and manual ventilating, retrrived on
http://www.modernmedicine.com/modern-medicine/content/manual-ventilation - Vanaswegen, h., & eales, c. j. (2011). the effectiveness of manual hyperinflation during the physiotherapy management of acute atelectasis: a case report. south African journal of physiotherapy, 60(1), 29-32. retrived on :
http://www.sajp.co.za/index.php/sajp/article/vie w/181