Information
Journal Policies
Factors Affecting Endotracheal Tube Cuff Pressure Measurement: A Review of Literature
NahlaShaaban Ali Khalil1, Reham Ahmed Mohamed Salama2, Warda Youssef Mohammed3, Mohamed Soliman Sayed4
2.Clinical Instructor of Critical Care and Emergency Nursing, Faculty of Nursing, Cairo University.
3.Prof. of Critical care and Emergency Nursing, Faculty of Nursing, Cairo University.
4.Lecturer of Critical Care Medicine, Faculty of Medicine, Cairo University.
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Background: Maintaining the endotracheal tube cuff pressure within an optimal range is challenging because many factors influence the pressure, as the patient’s position, head and neck position, weaning from sedation, agitation, quantity of injected air and suctioning.
Purpose of the article: To review previous studies regarding factors influencing endotracheal tube cuff pressure measurement among mechanically ventilated patients.
Methodology: All previous studies that discuss and debate factors influencing endotracheal tube cuff pressure measurement since 2004 till 2015.
Result and conclusion: the most factors influencing endotracheal tube cuff pressure are changing patient body position, head and neck position, loss of cuff volume with time, quantity of injected air in cuff, sedation and suctioning.
Recommendations: measurement and regular monitoring of endotracheal tube cuff pressure is crucial to avoid over and under inflation of endotracheal tube cuff pressure and consequently prevent complications.
Factors, Endotracheal tube, Cuff pressure, Nursing and Healthcare
1. Introduction
This review describes factors influencing endotracheal tube cuff pressure measurement; there are many factors affect the ETT cuff pressure in form of patient-related factors, environmental circumstances, and therapeutic interventions. Hence there is challenging to maintain the cuff pressure within an optimal range.
Invasive ventilation is a common treatment in intensive care units (ICUs) for patients with serious breathing problems; to secure airway for those patients tracheal intubation is required. So, the purpose of an artificial airway is to release upper airway obstruction, facilitate suctioning, allow effective ventilation and prevent aspiration (Fisher, Chenelle, Marchese, Kratohvil & Kacmarek, 2014).
Cuffed ETT is usually used during invasive mechanical ventilation (IMV) as the main ETT cuff function is to provide an adequate seal of the airway, prevent the air or fluids passage around the ETT. When this seal is cooperated, pharyngeal contents aspirations and poor ventilation may occur, causing respiratory complications (Bolzan, et al, 2012).
So that it is recommended to maintain cuff pressure (CP) within therapeutic range 20–30 cmH2O. Optimal ETT cuff pressure can be defined as the minimal pressure required for airway isolation. This intra CP is influenced by several factors such as airway anatomy, cuff location, cuff material and structure, cuff size and cuff volume, and by peak inspiratory pressure (Efrati, Deutsch, & Gurman, 2012). In addition, suctioning and patient position also affect ETT cuff pressure (Jaillette, MartinLoeches, Artigas & Nseir, 2014).
2. Factors Influencing Ett Cuff Pressure Measurement
There is challenging to maintain the cuff pressure within therapeutic range because there are many factors influencing the ETT cuff pressure, the endotracheal tube cuff pressure differs according to patient-related factors, environmental circumstances, and therapeutic interventions. Patient related factors according to Jaillette, et al, 2014, Das& Kumar, 2015 and Lizy, et al, 2014 are patient position, the ratio between cuff and tracheal diameter, head and neck position and decreased core temperature.
As mentioned by Lizy, et al, 2014, environmental circumstances/factors are altitude (e g, during helicopter transport) and loss of cuff volume with time. Finally as reported by Lizy, et al, 2014, Jaillette, et al, 2014 and Memela & Gopalan, 2014, therapeutic interventions/ factors are positive pressure ventilation, ventilation with nitrous oxide, sedation and neuromuscular blockade, quantity of air injected in the cuff, Suctioning and Cuff physical characteristics.
3. Patient Related Factors
There may be considerable variation in the intra cuff pressure throughout the period of endotracheal intubation as pressure within the cuff is a dynamic process that may be altered by several factors including variation in head and neck position (Kako, et al, 2014). The ETT can be displaced by movement of the patient’s head and neck. Movement of the head and neck and the displacement of ETT can cause a change in ETT cuff pressure (Kim, et al, 2015). Rotated, extended and flexed positions of the head and neck have also been revealed to cause a greater increase in cuff pressure compared with the neutral position. (Tan, Lin, Chen& Hung, 2011).
According to Lizy, et al, 2014 changes in a patient’s body position resulted in significant deviations in the cuff pressure of endotracheal tubes. It is suggested that the patient should be turned every 2hours to alternating lateral and supine positions. The patient’s body should be turned laterally and the head of the bed elevated no higher than 30؛ to prevent pressure on the coccyx. This position may promote ventilator associated pneumonia in intubated patients and patients receiving enteral feeding (Cooper, 2013).
It is supposed to be important to select the appropriate size of endotracheal tube (ETT) to prevent ETT-induced complications, such as airway edema. An overinflated cuff or excessively large ETT relative to tracheal size may induce tracheal mucosal ischemia or hoarseness. Generally tracheal diameter can be measured by CT perfectly, but only a limited number of patients do CT images. , however, preoperatively, Chest X-ray images are frequently taken and used to evaluate the diameter of the trachea so as to determine the tracheal tube size. Yet, X-ray is not always accurate to measure tracheal diameter (Sakuraba, et al, 2010).
In this regard results of some studies show that lots of changes in body temperature along with anatomic changes which happen in cardiopulmonary bypass surgery can make change in endotracheal tube cuff pressure moreover, in laboratory conditions which was carried out by Atlas In a math model, the effect of gas emissions and temperature on the level of endotracheal tube cuff pressure was evaluated. Results showed that a mild increase of cuff pressure resulted from significant rise in temperature of the injected gas into the endotracheal tube cuff (Jaillette, et al, 2014).
The association of hypotension and high intra tracheal tube cuff pressure could be the chief reason of tracheal mucosal injury in cardiac surgery. The intra tracheal tube cuff pressure drops during the hypothermic phase of cardiopulmonary bypass (CPB) as reported by Inada et al.; this may protect the tracheal mucosa against hypotensive ischemic injury. It was concluded that the intra tracheal tube cuff pressure is higher in normothermic cardiopulmonary bypass than in hypothermic cardiopulmonary bypass (Jaillette, et al, 2014).
During hypothermic cardiopulmonary bypass; Inada et al detected that cuff pressure was significantly reduced (from a mean baseline value of20 to 8 mmHg) however; this was not found in patients receiving norm thermic cardiopulmonary bypass. They clarified that the changes observed might be due to cold-induced vasoconstriction and contraction of the microvasculature of the tracheal wall causing tracheal caliber expansion during hypothermia. (Tan, et al, 2011).
4. Environmental Factors (Environ Mental Circumstances)
Before and during flight, hospital and out-of-hospital practitioners ought to measure and adjust endotracheal cuff pressures because in a closed space gas, such as an endotracheal tube cuff, will increase with increasing elevation (ie, decreased ambient barometric pressure), the intra cuff pressure can increase substantially during aero medical transport (Bessereau, Coulange, Fournier & Michelet, 2010).
ETT cuff pressure often decreases over time. Using intermittent monitoring, Sole and colleagues, noted decreases in ETT cuff pressure within 4 to 12hours after adjustment of the pressure to 20 cm H2O.Sridermma and colleagues reported that cuff pressure decreased to 20 cm H2O in 4 to 5 hours after initial adjustment to 25 cm H2O. Similar findings were noted when cuff pressure was monitored continuously. Longer duration of intubation was associated with greater decreases in pressure over time (Sole, et al, 2011).
5. Therapeutic Interventions
Remarkably, the amount of air needed to attain a pressure of 20 cmH2O is small, extending from 2.6 mL for a 7.0-mm ETT to 3.3 mL for an 8.5-mm tube(Sole, et al, 2011).Measured cuff volumes were also similar with each tube size. Interestingly, the amount of air required to achieve a cuff pressure of 20 cmH2O was similar with each tube size. However, there was great inconsistency in the required amount of air (Sengupta, et al, 2004).
The presence of an artificial airway during mechanical ventilation makes coughing less effective or not possible. Endotracheal suctioning is therefore needed to avoid accumulation of secretions into the lung, and its associated complications. Nevertheless, endotracheal suctioning is an invasive procedure, and is not free from hazards and, exceptionally, from lethal adverse events. Numerous side effects of endotracheal suctioning have been reported. Some old studies on selected patient populations suggested a high frequency of specific adverse events, such as oxygen desaturation and arrhythmia (Maggiore, et al, 2013).
In a bench top model, it has been validated that the amount of leakage around the cuff is related to the pressure differential across the cuff, namely the difference between the pressure of the subglottic fluid above the cuff and the tracheal pressure under the cuff. Positive end-expiratory pressure (PEEP) enhances the sealing around the cuff toward fluid leakage nevertheless, this preventive effect of PEEP may be cooperated by time as tracheal suctioning maneuver, with prolonged mechanical ventilation decreases tracheal pressure and enhances fluid leakage in vitro(Beuret, Philippon, Fabre, & Kaaki, 2012).
Because of applying negative pressure during tracheal suctioning it could be associated with higher risk for micro aspiration, It has been proved that leakage rate around the cuff depends on the difference in pressure between the two areas above and below the cuff(Jaillette, et al 2014).
A higher minimum cuff pressure is essential to avoid leak of an air at higher peak airway pressures. One observational study revealed that a peak airway pressure greater than 48 cmH2O prerequisite a cuff pressure greater than 25 mmHg to prevent an air leak (Efrati, et al 2012).
In ICUs mechanically ventilated patients need sedation to enhance comfort, decrease psychological stress, control pain, and facilitate nursing procedures. The risk of ventilator associated pneumonia may develop due to excessive sedation and later withdrawal syndrome, while it prolongs mechanical ventilation and ICU length-of-stay, Alert control of sedation and regular assessment of individual sedation needs have thus been recommended. Others advocate a daily interruption of sedative infusions or even completely avoiding sedation for mechanically ventilated patients. The amount of sedation required in ICU patients depends on the underlying illness and comorbidities (Le Guen, et al, 2013).
Sedation requirements also change over time, with sudden nociceptive stimuli in hemodynamic ally unstable patients making the ICU a challenging environment for sedation. Moreover, physicians and nurses in critical care units have many responsibilities besides sedation and can thus give only limited time to this task (Le Guen,et al, 2013).Hence it is considered an essential part of intensive care practice to lessen patient discomfort and anxiety, facilitate mechanical ventilation and allow serious intensive care procedures (Shehabi, et al, 2013).N2O diffuses more rapidly into the cuff than nitrogen diffuses out of the cuff, thus creating excessive pressure even when the initial sealing pressure is satisfactory (Efrati, et al,2012).
It was noted that patients who were agitated, greater changeability in ETT cuff pressure occurred, and that change ability decreased after the patient received sedation. During agitation and some movement, the ETT cuff pressure often “dipped,” potentially increasing the risk for aspiration of oropharyngeal secretions (Lizy, Swinnen, Labeau & Blot, 2011).
6. Cuff Physical Characteristics
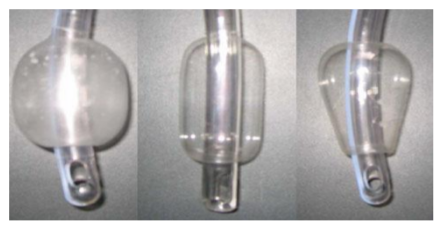
Tracheal tubes can be classified based on the relationship between volume and cuff pressure. Cuff shape and material can also differ between tracheal tubes.
The first tracheal cuffs were small-volume high-pressure. These cuffs allow sealing with a small area of contact with tracheal wall, but require high pressure (> 50 cmH2O) to obtain tracheal sealing. The cuff pressure allowing adequate sealing is much higher than the perfusion pressure of tracheal mucosa resulting in tracheal injury. Their use was associated with high incidence of ischemic tracheal lesion and subsequent complications such as tracheal stenosis and rupture.
Regrettably, on the market these cuffs are still offered and used in some patients, because of their high risk for tracheal injury they should be controlled. Now, Most used cuffs are highvolume low-pressure. Lately, low-volume lowpressure cuffs have been studied in critically ill patients. These silicone cuffs provide accurate sealing of the trachea with acceptable pressure (< 30 CmH2O). Young and colleagues results showed significantly lower leakage using these cuffs compared with conventional high-volume low pressure by evaluating these cuffs in vitro, in patients anesthetized for surgery, and in critically ill patients (Jaillette, et al, 2014).
The simple rational behind the HVLP cuffs is that when the cuff volume is greater the contact surface between the cuff and the tracheal mucosa is larger, the pressure is spread over bigger contact area and less pressure per contact point is required in order to achieve sealing. Additionally it assures no spaces due to noncircular (or near circular) tracheal shapes (Efrati, et al, 2012).
The cuff in Low volume low pressure (LVLP) is intentional to be fully inflated when used. This has two vital significances. First, the cuff does not develop longitudinal folds alongside the wall the cuff is under tension. Secondly, the pressure exerted on the tracheal wall by the cuff is less than the intra cuff pressure due to partial dissipation of intra cuff pressure into elastic forces within the cuff (Efrati, et al, 2012).
Three cuff shapes are available in barrel (standard), cylindrical, and conical (tapered). Polyurethane could reduce the risk of micro aspiration and VAP. This material is much thinner than PVC, resulting in reduced formation of folds between the cuff and tracheal wall (Jaillette, et al 2014).
Patients intubated with polyvinyl chloride (PVC)-cuffed tubes spend a large amount of time with under inflation or over inflation of the tracheal cuff. Recently, polyurethane (PU)- cuffed tracheal tubes have been commercialized. These tubes have been shown to decrease leakage of oropharyngeal secretions The PU cuff has a thinner wall (7 lm vs. the more typical 50 lm) and generates a better tracheal seal at generally accepted safe cuff inflation pressures via the creation of smaller channels that impede drainage of oropharyngeal secretions below the tracheal tube cuff (Nseir, et al, 2010).
Ultrathin polyurethane cuffs seal more consistently against the tracheal wall and may therefore allow fewer secretions to leak around the cuff and into the lungs (Klompas, et al,
2014).
References
- Bessereau, J., Coulange, M., Jacquin, L., Fournier, M., & Michelet, P. (2010). Endotracheal tube intracuff pressure during helicopter transport. Annals of emergency medicine, 56(5), 583-584.
- Beuret, P., Philippon, B., Fabre, X., & Kaaki, M. (2012). Effect of tracheal suctioning on aspiration past the tracheal tube cuff in mechanically ventilated patients. Annals of intensive care, 2(1), 45.
- Bolzan, D. W., Guizilini, S., Faresin, S. M., Carvalho, A. C., De Paola, A. A., & Gomes, W. J. (2012). Endotracheal tube cuff pressure assessment maneuver induces drop of expired tidal volume in the postoperative of coronary artery bypass grafting. Journal of cardiothoracic surgery, 7(1), 53.
- Cooper, K. L. (2013). Evidence-based prevention of pressure ulcers in the intensive care unit. Critical care nurse, 33(6), 57-66.
- Das, S., & Kumar, P. (2015). Comparison of minimal leak test and manual cuff pressure measurement technique method for inflating the endotracheal tube cuff. Indian Journal of Clinical Anaesthesia, 2(2), 78-81.
- Efrati, S., Deutsch, I., & Gurman, G. M. (2012). Endotracheal tube cuff-small important part of a big issue. Journal of clinical monitoring and computing, 26(1), 53-60.
- Fisher, D. F., Chenelle, C. T., Marchese, A. D., Kratohvil, J. P., & Kacmarek, R. M. (2014). Comparison of commercial and noncommercial endotracheal tube-securing devices. Respiratory care, respcare-02951
- Jaillette, E., Martin-Loeches, I., Artigas, A., & Nseir, S. (2014). Optimal care and design of the tracheal cuff in the critically ill patient. Annals of intensive care, 4(1), 7.
- Kako, H., Krishna, S. G., Ramesh, A. S., Merz, M. N., Elmaraghy, C., Grischkan, J., ... & Tobias, J. D. (2014). The relationship between head and neck position and endotracheal tube intra cuff pressure in the pediatric population. Pediatric Anesthesia, 24(3), 316-321.
- Kim, D., Jeon, B., Son, J. S., Lee, J. R., Ko, S., & Lim, H. (2015). The changes of endotracheal tube cuff pressure by the position changes from supine to prone and the flexion and extension of head. Korean journal of anesthesiology, 68(1), 27-31.
- Le Guen, M., Liu, N., Bourgeois, E., Chazot, T., Sessler, D. I., Rouby, J. J., & Fischler, M. (2013). Automated sedation outperforms manual administration of propofol and remifentanil in critically ill patients with deep sedation: a randomized phase II trial. Intensive care medicine, 39(3), 454-462.
- Lizy, C., Swinnen, W., Labeau, S., & Blot, S. (2011). Deviations in endotracheal cuff pressure during intensive care. American Journal of Critical Care, 20(6), 421-422.
- Lizy, C., Swinnen, W., Labeau, S., Poelaert, J., Vogelaers, D., Vandewoude, K. ... & Blot, S. (2014). Cuff pressure of endotracheal tubes after changes in body position in critically ill patients treated with mechanical ventilation. American Journal of Critical Care, 23(1), e1-e8.
- Maggiore, S. M., Lellouche, F., Pignatarro, C., Girou, E., Maitre, B., Richard, J. C. M. ... & Brochard, L. (2013). Decreasing adverse effects of endotracheal suctioning during mechanical ventilation by changing practice. Respiratory care, respcare-02265.
- Memela, M. E., & Gopalan, P. D. (2014). Variations in endotracheal tube cuff pressure: Is 8-hourly monitoring enough?. Southern African Journal of Critical Care, 30(2), 35-40.
- Sakuraba, S., Serita, R., Kuribayashi, J., Kosugi, S., Arisaka, H., Yoshida, K., & Takeda, J. (2010). Comparison of tracheal diameter measured by chest x-ray and by computed tomography. Anesthesiology research and practice, 2010.
- Sengupta, P., Sessler, D. I., Maglinger, P., Wells, S., Vogt, A., Durrani, J., & Wadhwa, A. (2004). Endotracheal tube cuff pressure in three hospitals, and the volume required to produce an appropriate cuff pressure. BMC anesthesiology, 4(1), 8.
- Shehabi, Y., Chan, L., Kadiman, S., Alias, A., Ismail, W. N., Tan, M. A. T. I. ... & Tan, C. C. (2013). Sedation depth and long-term mortality in mechanically ventilated critically ill adults: a prospective longitudinal multicentre cohort study. Intensive care medicine, 39(5), 910-918.
- Sole, M. L., Su, X., Talbert, S., Penoyer, D. A., Kalita, S., Jimenez, E. ... & Bennett, M. (2011). Evaluation of an intervention to maintain endotracheal tube cuff pressure within therapeutic range. American Journal of Critical Care, 20(2), 109-118.
- Tan, P. H., Lin, V. C., Chen, H. S., & Hung, K. C. (2011). The effect of transoesophageal echocardiography probe insertion on tracheal cuff pressure. Anaesthesia, 66(9), 791-795.