Information
Journal Policies
Scent on the Newborn and Pain Effects
Merve ezen1, Ayfer acikgoz1*
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Purpose: The aim of this compilation is to give information about the odors that can be applied to newborns.
Method: This study is of compilation type.
Findings: The sense of smell is much more developed in newborns compared to other senses; therefore, it is known that aromatic smells or the smells of human milk, the breast of mother, amniotic fluids, etc. that the newborn is familiar to reduces the level of stress of newborn during the first days of their life. Furthermore, there are studies researching that these smells reduce pain during painful interventions. However, it is observed that this practice is not commonly used in newborn units.
Results: The smell of human milk is an effective and easy-to-use tool for reducing the pain and stress felt by newborns. We recommend that this practice is applied in all newborn units.
Newborn, stress, pain, human milk, smell,Nursing and Healthcare
1. Introduction
The neonatal period poses extensive risks to the infant because it is a time during which the newborn should adapt to the extrauterine life [1]. The risk is especially higher in the newborns in intensive care units (ICUs) due to various health problems. The reasons for this condition may be the exposure of the infant to adverse environmental conditions (such as intense light and sounds or irritating odors in the environment) and the painful interventions the infant should undergo at the intensive care unit (ICU) [2,3]. In the 1980s, "The Newborn Individualized Developmental Care and Assessment Program" (NIDCAP) was founded by Heidelise Als to support and protect the development of newborns in the presence of pain and stress the infants are exposed to [4,5]. NIDCAP involves individual caring for each infant, establishing co-operation with parents, enhancing the mother-infant bonding, promoting collective care in nursing practices, kangaroo mother care and proper positioning of the infant, and environmental management (regulating the intensity of the sound and light) [6-8]. These initiatives help reduce the intensity of the pain and stress experienced by the infants [9]. management is odors [10].
Another important aspect of environmental Smelling is a sense having critical effects on the development of the fetus and on the transition period when the infant adapts to oral feeding in the postnatal period [11]. The newborn's reaction to the mother's breast and to breast milk represent the most important evidence of this fact. Several studies in the literature have demonstrated that the scents administered to the newborns, such as the maternal scents (the scent of the breast milk, the scent of the amniotic fluid, etc.) [12,13] or other soothing scents (vanilla, etc.) [14,15], shortened the duration of crying of the infants and reduced their scores of pain. For this reason, it is critical to implement the use of odors in the care of the newborns who have to be hospitalized at ICUs and have to undergo painful interventions during the period of adaptation to the extrauterine life.
2. The Physiology Of Scent And The Development Of Sense Of Smell In Newborns
In the human nose, there is a specialized area of tissue named as the olfactory region, which is localized high inside the nasal cavity, extending to the nasal septum and the superior conchae [16]. Physiologically, the air containing the odorant molecules filters into the nose and stimulates the olfactory cells in the olfactory epithelium [17]. The odorant first filtrates into the mucosa upon coming into contact with the surface of the olfactory area, subsequently binding to a receptor protein (cAMP). The associated receptor, then, activates the sodium channels resulting in the stimulation of the olfactory neurons by the sodium ions. The action potentials generated by these chain of events are transmitted to the central nervous system through the olfactory nerve [18,19].
Today, it is a well-recognized fact that the sense of smell is a sense that also develops sufficiently in the newborns [20]. The primary olfactory receptors are present in the eighth week of gestation and they appear mature at the end of the second trimester [21]. The olfactory marker protein has been found to develop in the olfactory mucosa and in the olfactory bulb in the 28th and the 32-35th weeks of gestation, respectively [22]. Thus, the sense of smell develops in the fetus in the 26-28th weeks of gestation [23] and an infant born prematurely in the 28th week of pregnancy can respond to different odors, by frowning, grimacing, and sneezing [24,25]. The sense of smell is not a merely momentary phenomenon in the newborn infants as they have also developed a memory for recognition of the odors. In a study [26], the investigators have administered the scent of chamomile to the newborn infants during nursing for a duration of approximately two months. It was determined that, in the 7th and 21st months following the administration, the newborns in the study were attracted to the objects with the scent of chamomile, rather than being attracted to odorless objects or objects scented with other odors.
In the light of this information, preventing the occurrence of unpleasant odors at ICUs and administering the scents which will sooth the newborns have gained importance. The odors to be introduced to the newborn can be classified into two categories, which are the familiar odors and the unfamiliar ones. The familiar odors include the scents of the mother, the breast milk, and the amniotic fluid [27]. The scents of lavender, vanilla, and etc. can be set as examples to the unfamiliar scents [28]. However, as it is presented in the study by Rattaz et al. (2005), the scent of vanilla can be a familiar odor, too, since it shares some similarities with the odor of breast milk [20].
3. The Effects Of Scent On The Newborn
The individualized developmental care practices include keeping the newborn infants away from penetrant and unpleasant odors and administrating the soothing scents. For example, alcohol, cleaning chemicals, and disinfectants pose unpleasant stimuli to the infants. When these stimuli are ameliorated, the intensity of the adverse physiological reactions and the negative experiences arising from the exposure to these odors diminish. If a newborn is exposed to the scent of alcohol every time when it undergoes an invasive intervention, it may start crying whenever it smells the scent of alcohol [23,29].
The soothing scents (the breast milk, vanilla, and etc.), on the other hand, reduce the frequency of apnea in newborns [14], regulate the respiration [15] and oxygen saturation [30], reduce the duration of the crying periods [13], and decrease the intensity of the motor agitation that results from invasive procedures [20].
4. The Recommended Scents For Newborns
4.1.1. The Scent of the Amniotic Fluid
The fetal olfactory receptors are exposed to the amniotic fluid in the intrauterine environment. Therefore, it is believed that the postpartum introduction of the scent of the amniotic fluid to the newborn infants is effective due to this familiarity [11]. In a study by Varendi et al. [31], a drop of amniotic fluid was applied to one of the breasts of the mothers right after the birth and the infants were placed on the chest of their mothers in the area between the two breasts. In this study, it was determined that 27 out of 30 infants started to suck the breast to which the amniotic fluid was applied. Another study [32] determined that newborns in the first two days of life turned their heads to the pads where amniotic fluid or colostrum was applied when they were exposed to the pads on which the amniotic fluid, colostrum or water was dropped. The four-day-old full-term newborns, on the other hand, were observed to turn their heads towards breast milk. A study [33] conducted with full-term healthy newborns in the third days of life found out that the infants turned their heads towards the pad with the scent of their own amniotic fluid when they were exposed to the pads scented with their own amniotic fluid and to the pads scented with the amniotic fluid from another person. These results suggest that prenatal memory of olfactory learning is sustained for a certain period of time after the birth; however, the postnatal factors become more prominent after some time [11].
4.1.2. Breast Milk and the Scent of the Mother
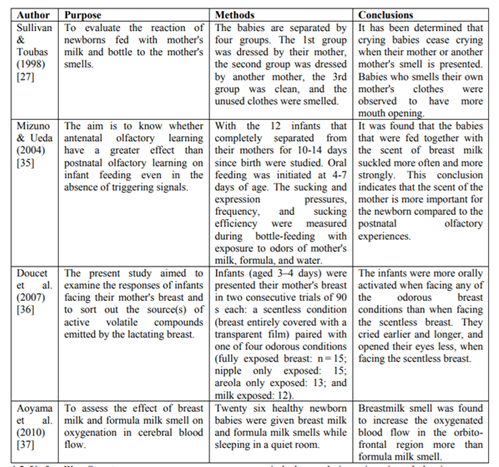
The sense of smell is one of the most developed senses creating an emotional bond between the mother and the newborn, leading to effective behavioral reactions in the newborn infants such as causing them to reach their mothers' breast [34]. On the fifth day of life, the newborns can distinguish their mother's scent from that of any other mother and they can smell and recognize the odor coming from the nipples in order to feed themselves with breast milk without any prior experience of feeding [13].
Newborns can also similarly respond to some scents other than the scents of the amniotic fluid and the breast milk. It is thought that this effect originates from the distracting properties of the scents [20]. For example, the scent of vanilla is reported to decrease the frequency of apnea in the preterm infants [14] and the introduction of lemon-scented cotton sticks help regulate the respiration in the newborn infants [15]. Rattaz et al. (2005) reported that the newborn infants cried less, their grimacing behaviors were reduced, they had fewer motor agitations during the blood sampling processes, and had lesser degrees of respiratory distress after interventions when the scent of vanilla was administered to the newborn infants during the blood sampling from the heel [20]. Akcan and Polat (2016) determined in their study that the administration of the scent of lavender diminished the intensity of the pain during the heel-lancing process to collect blood [30]. The study by Kane et al. (2004) reported that the scent of lavender diminished the intensity of the pain in the newborns while changing their dressings [38].
5. Administration Of Scents During Painful Interventions
Pain can be associated with many factors in newborns. A major cause of pain is invasive interventions which include venous blood sampling, urinary catheterization, umbilical artery catheterization, and intubation [39]. In a study conducted by Simons et al. (2003) at a newborn intensive care unit, it was determined that the newborns were exposed to 14 pain inducing interventions per 24 hours in the first 14 days of their hospitalization [40]. The pain experienced by the newborn infants due to those interventions can adversely affect their modes of behavior, their adaptation to the extrauterine life, their interactions with their mothers, their feeding patterns, and their growth and development [41]. For this reason, it is necessary to manage the pain in a timely and correct manner. There are pharmacological and non-pharmacological methods for pain control. Although the pharmacological methods display an early onset of action and they are the most effective methods to control pain [42], they may have some adverse effects on the physiological functions when used frequently and without control [43,44]. The non-pharmacological methods are suggested as reliable modalities to reduce the rate of analgesic use or to enhance their effects [45]. There are several non-pharmacological methods for pain control. These include touching, kangaroo mother care, positioning, pacifier use, breastfeeding [46,47], administration of oral sugar solutions [48], and listening to music [49]. Another effective method is the administration of scents [10].
It is suggested that odors display soothing and pain alleviating effects by inducing the release of associated neurotransmitters [50]. This effect can be explained via the chemical properties of the maternal scents, the newborn's relationship with the maternal environment, or the familiarity of the newborn with these scents [20]. The studies demonstrate that the scent of the amniotic fluid [12], the maternal scent [27], and the scents of breast milk [13,51] lavender [30], and vanilla [20] diminish the levels of pain during invasive procedures. It is suggested that the healthcare professionals at newborn intensive care units should use these methods, especially during painful interventions.
The responsibility of nurses in the control of pain is extensive as they spend most of their times with their newborn patients observing them. Nurses must apply the required interventions completely to keep the levels of pain within tolerable limits [52]. However, a study [53] has demonstrated that only 27.6% of nurses and doctors use non-pharmacological methods. Another study [54] has found that 65% of nurses administered analgesics as the first-line treatment for pain relief. These results indicate that the non-pharmacological methods are not used commonly enough. However, it is known that the non-pharmacological methods have an important role in the control of pain in the newborn infants. For this reason, the awareness of nurses on the pain-controlling interventions should be increased and their levels of knowledge should be enhanced.
6. Conclusion And Suggestions
The sense of smell develops during the intrauterine period in newborns. After birth, newborn gives various reactions to smells. Disturbing odors in the environment affect the newborn in a negative way, while sedative odors cause positive responses in the newborn. Especially in intensive care units, prevention of bad smell and application of smells that relieve the newborn is very important. Relaxing odors include maternal smells such as mother, breast milk, amniotic fluid, and soothing scents such as lavender and vanilla. Administration of scents to the newborn infants is an effective non-pharmacological method to alleviate the pain and stress. We suggest that protocols to regulate the administration of relevant scents to the infants should be developed, training programs on this issue should be provided to the healthcare providers, and support should be available for the staff in their practices especially at newborn intensive care units. It is also advisable to prove the positive effects of the smells in the newborns with more work and to share these results with the health personnel.
References
- Toruner E. and Buyukgonenc L., (Ed.) Child Health Basic Nursing Approaches, Ankara Nobel Medical Bookstores, Ankara, 2017, pp. 91-106, 233-251.
- Sehgal A. and Stack J, Developmentally Supportive Care and NIDCAP, Indian J Pediatr. 73(11), pp. 1007-110, (2006).
- Vandenberg K. A., Individualized Developmental Car Efor High Risk Newborns in the NICU: A Practice Guideline, Early Human Development. 83, pp. 433-42, (2007).
- Byers J. F., Components of Developmental Care and the Evidence for Their Use in the NICU, MCN Am J Matern Child Nurs. 28(3), pp. 174-80, (2003).
- Symington A. and Pinelli J., Developmental Care for Promoting Development and Preventing Morbidity in Preterm Infants. The Cochrane Database of Systematic Reviews, 4: No.: CD001814. doi: 10.1002/14651858.CD00 1814. (2003).
- Eras Z., Atay G., Durgut E. S., Bingoler E. B. and Dilmen U., Developmental Care in Neonatal Intensive Care Unit, The Medical Bulletin of Şişli Etfal Hospital. 47(3), pp. 97-103, (2013).
- Coughlin M., Gibbins S. and Hoath S., Core Measures for Developmentally Supportive Care in Neonatal İntensive Care Units: Theory, Precedence and Practice, Journal of Advanced Nursing. 65(10), pp. 2239–48, (2009).
- Butler S. and Als H., Individualized Developmental Care Improves The Lives of Infants Born Preterm, Acta Pediatrica Promoting Child Health. 97: 1173-5, DOI:10.1111/j.1651-2227.2008.00916.x.(2008).
- Sizun J., Ansquer H., Brpwre J., Tordjman S. and Morin J. F., Developmental Care Decreases Physicologic and Behavioral Expression in Preterm Neonates, J Pain. 2, pp. 446-50, (2002).
- Zeller B. and Giebe J., Pain in the Neonate: Focus on Nonpharmacologic Interventions, Neonatal Network. 33(6), pp. 336-340, (2014).
- Bloomfield F. H., Alexander T., Muelbert M. and Beker F., Smell and taste in the preterm infant, Early Human Development. 114, pp. 31-34, (2017).
- Varendi H., Christensson K., Porter R. H. and Winberg J., Soothing Effect of Amniotic Fluid Smell in Newborn Infants, Early Human Development. 51, pp. 47–55, (1998).
- Nishitani S., Miyamura T., Tagawa M., Sumi M., Takase R., Doi H., Moriuchi H. and Shinohara, K., The Calming Effect of a Maternal Breast Milk Odor on the Human Newborn Infant, Neuroscience Research. 63, pp. 66-71, (2009).
- Marlier L., Gaugler C. and Messer J., Olfactory Stimulation Prevents Apnea in Premature Newborns, Pediatrics. 115(1), pp. 83-8, (2005).
- Garcia A.P. and White-Traut R. Preterm İnfants Responses To Taste/Smell And Tactile Stimulation During on Apneic Episode, Journal Of Pediatric Nursing. 8(4), pp. 245-52, (1993).
- Ballenger JJ., (Çeviri: İnallı S.) Burun ve paranazal sinüslerin klinik anatomi ve fizyolojisi. Ed: Ballenger JJ. and Snow JB., Otolaringoloji Bas ve Boyun Cerrahisi, Nobel Tıp Kitapevleri, pp. 3-18, (2000)
- Nathan RA., Eccles R., Howarth PH., Steinsvag SK. and Togias A., Objective monitoring of nasal patency and nasal physiology in rhinitis, J Allergy Clin İmmunol. 115: pp. 442-59, (2005).
- Hadley K., Orlandi RR. and Fong KJ., Basic anatomy physiology of olfaction and taste, Otolaryngol Clin N Am. 37: pp. 1115-26, (2004).
- Guyton AC., Olfactory physiology, Text Book of Medical Physıology. Guyton AC. and Hall CE., (ed). 10’s edn, W.B. Saunders company, pp. 616-9, (2001).
- Rattaz C., Goubet N. and Bullinger A., The calming effect of a familiar odor on full term newborns, J Dev Behav Pediatr. 26: pp. 86-92, (2005).
- Ganchrow JR. and Mennella JA., The ontogeny of human flavor perception. In: Doty RL., (ed), Handbook of Olfaction and Gustation, 2nd edition ed. Marcel Dekker, Inc.; New York: pp. 823–946, (2003).
- Chuah M. I. and Zheng D.R., Olfactory marker protein is present in olfactory receptor cells of human fetuses, Neuroscience. 23 (1), pp. 363-370, (1987).
- McGrath JM., Feeding. In: Kenner C., and McGrath JM., (eds). Developmental Care of Newborns and Infants: A Guide for Health Professionals. St. Lo-uis, Elsevier, pp. 321-342 (2004).
- Muslu G. K., Regulation of Physical Environment in Neonatal Intensive Care Units, International 3rd National Pediatric Nursing Congress Book, İzmir, pp. 9-13, (2011).
- Yıldırım Z., Individualized Developmental Care in Prematurity, XI. National Neonatology Congress Congress Book, Samsun, pp. 236-242, (2001).
- Delaunay-El Allam M., Soussignan R., Patris B., Marlier L. and Schaal B., Long-lasting memory for an odor acquired at the mother's breast, Dev. Sci. 13 (6), pp. 849-863, (2010).
- Sullivan R. M. and Toubas P., Clinical usefulness of maternal odor in newborns: soothing and feeding preparatory responses, Biol Neonate. 74, pp. 402-408, (1998).
- Goubet N., Strasbaugh K. and Chesney J., Familiarity breeds content? Soothing effect of a familiar odor on full-term newborns, J Dev Behav Pediatr. 28(3): pp. 189-94, (2007).
- Hennessy AC., Routine care of the healthy newborn. In: De Kock J. and van der Walt C., (eds.), Maternaland Newborn Care: A Complete Guide for Midwives and Other Health Professionals, Pretoria, Juta Academic, 0340, (2004).
- Akcan E. and Polat S., Comparative Effect of the Smells of Amniotic Fluid, Breast Milk, and Lavender on Newborns' Pain During Heel Lance. Breastfeed Med. 11(6): https://doi.org/10.1089/bfm.2015.0174. (2016).
- Varendi H., Porter R. H. and Winberg J., Attractiveness of amniotic fluid odor: evidence of prenatal olfactory learning? Acta Paediatr. 85 (10), pp. 1223-1227, (1996).
- Marlier L., Schaal B. and Soussignan R., Neonatal Responsiveness to the Odor of Amniotic and Lacteal Fluids: A Test of Perinatal Chemosensory Continuity, Child Dev. 69 (3): pp. 611-623, (1998).
- Schaal B., Marlier L. and Soussignan R., Olfactory function in the human fetüs: evidence from selective neonatal responsiveness to the odor of amniotic fluid, Behav. Neurosci. 112 (6), pp. 1438-1449, (1998).
- Aboli B. P., Shamsi A. and Iranmanesh S., The Effect of Breast Milk Odor on First Breast Feeding Time and Weight Gain in Premature Infants, I-Manager’s Journal on Nursing. 5(3): pp. 27-33, (2015).
- Mizuno K. and Ueda A., Antenatal olfactory learning influences infant feding, Early Hum Dev. 76(2): pp. 83-90, (2004).
- Doucet S., Soussignan R., Sagot P. and Schaal B., The ‘‘Smellscape’’ of Mother’s Breast: Effects of Odor Masking and Selective Unmasking on Neonatal Arousal, Oral, and Visual Responses, Developmental Psychobiology. DOI 10.1002/dev: 130-8, (2007).
- Aoyama S., Toshima T., Saito Y., Konishi N., Motoshige K., Ishikawa N., Nakamura K. and Kobayashi M., Maternal Breast Milk Odour Induces Frontal Lobe Activation in Neonates: A NIRS Study, Early Human Development. 86: pp. 541-5, (2010).
- Kane F. M., Brodie E. E., Coull A., Coyne L., Howd A., Milne A., Niven C. C. and Robbins R., The analgesic effect of odour and music upon dressing change, Br J Nurs. 13: pp. 4-12, (2004).
- Yigit S., Ecevit A. and Koroglu O. A., Guidelines for Pain and Treatment During the Newborn Period, Turkish Neonatology Association.
http://www.tuseb.gov.tr/tacese/yuklemeler/ekitap/K%C4%B1lavuzlar/Yenido%C4%9Fan%20D%C3%B6neminde%20A%C 4%9Fr%C4%B1%20ve%20Tedavisi%20Rehbe ri.pdf . (2015). - Simons S.H., van Dijk M., Anand K.S., Roofthooft D., van Lingen R.A. and Tibboel D., Do We Still Hurt Newborn Babies? A Prospective Study of Procedural Pain and Analgesia in Neonates, Arch Pediatr Adolesc Med. 157(11): pp. 1058-64. doi: 10.1001/archpedi.157.11.1058. (2003).
- Canadian Paediatric Society, Prevention and Management of Pain and Stress in the Neonate, Pediatrics. 105(2): pp. 454-61, (2000).
- Neuhäuser C., Wagner B., Heckmann M., Weigand M. A. and Zimmer K.P., Analgesia and Sedation for Painful Interventions in Children and Adolescents, Deutsches Ärzteblatt International. 107(14), pp. 241-247 doi: 10.3238/arztebl.2010.0241. (2010).
- Nester T. M. and Hale L. S., Effectiveness of Pharmacist Acquired Medication History in Promoting Patient Safety, Am J Health Syst Pharm. 59: pp. 2221-5, (2002).
- Arslan S. and Celebioglu A., Postoperative Pain Management and Alternative Practices, 10th International Journal of Human Sciences. pp. 1-7, (2004).
- Derebent E. and Yiğit R., Paın In Newborn: Assesment And Management, C.Ü. Journal of Nursing School. 10(2): pp. 41-8, (2006).
- Bellieni C. V., Bagnoli F., Perrone S., Nenci A., Cordelli D. M., Fusi M., Ceccarelli S., and Buonocore G., Effect of Multisensory Stimulation on Analgesia in Term Neonates: A Randomized Controlled Trial, Pediatric Research. 51(4): pp. 460-3, (2002).
- Gormally S., Barr R. G., Wertheim L., Alkawaf R., Calinoiu, N. and Young S. N., Contact and Nutrient Caregiving Effects on Newborn Infant Pain Responses, Developmental Medicine and Child Neurology. 43: pp. 28-38, (2001).
- Greenberg C. S., A Sugar-Coated Pacifier Reduces Procedural Pain in Newborns, Pediatric Nursing. 28: pp. 271-7, (2002).
- Almerud S. and Peterson K., Music Theraphy-a Complementary Treatment for Mechanically Ventilated Intensive Care Patients, Intensive and Critical Care Nursing. 19 (1): pp. 21-30, (2003).
- Kanbur B. N. and Balci S., Smell in Preterm Newborn, Journal of Health Science and Profession. 4(3): pp. 272-6, (2017).
- Badiee Z., Asghari M. and Mohammadizadeh M., The Calming Effect of Maternal Breast Milk Odor on Premature Infants, Pediatrics and Neonatology. 54: pp. 322-5, (2013).
- Cocelli L. P., Bacaksiz B. D. and Ovayolu N., The Nurse Factor in Pain Therapy, Gaziantep Medical Journal. 14: pp. 53-8, (2008).
- Akcan E. and Yigit R., Turkish Reliability and Validity Study of Premature Infant Pain Profile, F.U. Health Sciences Medical Journal 29 (3): pp. 97-102, (2015).
- Gol I. and Onarici M., Nurses’ Knowledge and Practices About Pain and Pain Control in Children, Hacettepe University Journal of Nursing Faculty. pp. 20-9, (2015).