Information
Journal Policies
Early Recognition of Sepsis in the Emergency Department
Nycole D. Oliver
Copyright : © 2018 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Problem Statement: In the United States, over three-quarters of a million patients are hospitalized with sepsis each year, with a mortality rate of just over 200,000.
Purpose: Increase early sepsis recognition in the ED through utilization of early goal-directed therapy.
Methods: A retrospective chart review (pre- and post- screening tool implementation) research design was used. Subjects were chosen based on diagnosis codes placed by the emergency clinician. Inclusion criteria: patients over the age of 18 with suspected infection plus two or more systemic inflammatory response syndrome (SIRS) criteria: (a) heart rate greater than 90, (b) systolic blood pressure less than 90, (c) mean arterial pressure less than 65, (d) temperature less than 96.8◦F or above 100.5◦F, and (e) respiratory rate above 20.
Analysis: Paired sample t-tests and the Wilson Score Confidence Interval were used to evaluate data pre-and post- implementation.
Results: The data did not give sufficient evidence to conclude the screening tool decreased door to diagnosis time, door to lactate measurement, or increased the percentage of blood cultures obtained prior to antibiotic administration. The data did conclude a decrease in diagnosis to antibiotic administration.
Significance: A screening tool for early recognition of sepsis may lead to a decrease in door to antibiotic time.
Sepsis, Screening Tool, Early Recognition, Emergency Department, Goal-Directed Therapy,Nursing and Healthcare
Sepsis is a systemic inflammatory response typically triggered by an infection, and is associated with hypoperfusion, hypotension, and/or organ dysfunction (Hermans, Leffers, Jansen, Keulemans, & Stassen, 2012; Burney et al., 2012). Sepsis accounts for over a half million emergency department (ED) visits each year (Hermans, et al., 2012). According to Hermans et al. (2012), one of the biggest advancements in sepsis treatment has been promotion of early goal-directed therapy (EGDT), a key component of which is early recognition in the ED.
In the United States, sepsis is in the top ten leading causes of death, with a mortality rate between forty to sixty percent (Burney et al., 2012). With over half a million annual ED visits for sepsis, the aforementioned mortality rate must be decreased. An interest by the corporate owner of a healthcare system has placed development of an early recognition protocol at the forefront of the ED director’s agenda (Kelly Hill, personal communication, September 18, 2014).
In the United States, over three-quarters of a million patients are hospitalized with severe sepsis each year, with a mortality rate of just over 200,000 (Perman, Goyal, &Gaieski, 2012). Medical costs related to sepsis are approximately $17 billion annually (Seymour et al., 2012). From 2003 to 2007, the total number of sepsis cases increased by seventy-one percent, while the total hospital costs increased by fifty-seven percent (Lagu et al., 2012). Various cost analyses of initiating an early goal-directed sepsis protocol have been conducted, and have concluded a protocol is cost-effective in the long run, especially when patient mortality rates are considered (Jones, Troyer, & Kline, 2011).
To date, a major driver of early sepsis recognition is the Surviving Sepsis Campaign (SSC). The SSC was initiated in 2002, and is a partnership of the European Society of Intensive Care Medicine and the Society of Critical Care Medicine (Society of Critical Care Medicine, n.d.). Many organizations who have implemented the SSC have seen a drastic decrease in mortality related to sepsis.
1. Clinical Question
The clinical question identified using the elements of population/problem, intervention, comparison, and outcome (PICO) is:In an adult population in an ED setting, does implementation of an assessment tool for identifying sepsis patients increase early recognition of sepsis by decreasing door to diagnosis times, decreasing time of presentation to serum lactate measurement, decreasing diagnosis to antibiotic times, and increasingthe number of blood cultures being obtained before antibiotic administration?
2. Review Of Literature
The University of South Alabama’sBiomedical Library, MEDLINE, and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) databases were utilized for search of the literature. Terms used for exploration included sepsis, early recognition of sepsis, sepsis and emergency department, sepsis protocol and emergency department, early recognition of sepsis and emergency department, and sepsis and early goal directed therapy. Search dates were limited to the last 5 years, and further refinement to only articles with full-text availability was performed.
After refinement of only full-text articles within the last 5 years, there were 3,512 hits while searching sepsis, 15 hits with early recognition of sepsis,145 with sepsis and emergency department, 6 with sepsis protocol and emergency department,6 with early recognition of sepsis and emergency department, and 29 with sepsis and early goal directed therapy. Each abstract was reviewed by the DNP student to determine relevancy to the clinical question. Fifteen studies were chosen for the literature summary table (see Appendices A-C), and each article was graded and ranked.
Of the studies, three were ranked a level I (evidence from at least one well-designed randomized controlled trial), six were a level II-2 (data from well-designed cohort or case-control analytic studies, from more than one center or research groupif at all possible), and six were a level II-3 (comparisons between times or places with or without the intervention: results from uncontrolled studies). For grading, ten were graded 1C (strong; can apply to most patients in most circumstances), two were graded 2A (intermediate-strength; best action may differ depending on circumstances or patient or societal values), and two were graded 2B (weak; alternate approaches likely to be better for some patients under certain circumstances).
The literature supplies different tactics to approach early recognition of sepsis in the ED; however, the research employs the same principle: a standardized approach and early recognition protocol must be in place to recognize, diagnose, and treat sepsis in the ED in a timely manner in order to increase outcomes for the patient and decrease length of stay and subsequent hospital costs.Seven of the fifteen studies included in the literature review recommend employing a triage screening tool and/or sepsis protocol in the ED to facilitate early recognition so the patient can receive treatment sooner, and increase the chances of survival. The studies employing a screening tool and/or ED sepsis protocol for EGDT showed a significant reduction in the time of diagnosis to antibiotic time and had a subsequent decrease in mortality rates (see Appendix A).
3. Project Methodology
Subjects were chosen based on diagnosis codes placed by the emergency clinician. Participants included ED patients at or over the age of 18 with suspected signs and symptoms of sepsis (described with inclusion criteria later). Participants were of different ages, various racial backgrounds, and from both genders. Inclusion criteria were patients with suspected infection such as pneumonia, skin infection, urinary tract infection, meningitis, abdominal infection, bone or joint infection, indwelling device/line, flu/viral/fungal illness plus two or more systemic inflammatory response syndrome (SIRS) criteria: (a) heart rate greater than 90, (b) systolic blood pressure less than 90, (c) mean arterial pressure less than 65, (d) temperature less than 96.8◦F or above 100.5◦F, and (e) respiratory rate above 20 (Appendix D). Exclusion criteria were patients who did not meet the criteria for sepsis according to a modified version of the Surviving Sepsis Campaign’s screening tool (Surviving Sepsis, 2013) (Appendix D).
The practice setting in which the project was implemented was a rural hospital ED in Fort Smith, Arkansas. The institution had over 154,000 patient interactions in 2011, and is growing each year (Sparks Health System, 2014). The hospital is licensed for 492 beds; the ED has 33 with the potential for 10 additional overflow beds. The ED treated over 70,000 patients in 2014. During a 12-hour shift, the ED is preferably staffed with: twelve Registered Nurses (RNs)/Licensed Practical Nurses (LPNs), two Unit Secretaries, three ED Technicians, three/four physicians/Nurse Practitioners, and twoTriage Technicians, along with subsidary staff (J. W. Kennon, personal communication, January 17, 2015).
A modification of the Surviving Sepsis Campaign’s data collection tool (Appendix E) best evaluated effectiveness for the student’s project (Surviving Sepsis Campaign, n.d). The tool has been utilized by numerous hospitals as part of the Surviving Sepsis Campaign bundles and has been proven to be a valid and reliable tool in measuring each step of the process. The modified tool measured whether the patient met criteria for sepsis based on the aforementioned screening tool (Appendix D), the date and time of presentation, admission category, serum lactate measurement and time, blood culture collection and time, antibiotic administration and time, and hospital discharge date and time.
To implement the project, the student identified a phenomenon of interest, performed a needs assessment, completed a literature review, established aims and outcomes for the project, provided a QI, EBP, and nursing theory model for basis of the project, and described project methodology. First, the student set up a measuring system to gather information in a 3 month retrospective chart review to determine the success of identifying patients with sepsis and determine the door to diagnosis time, the amount of time it took for a sepsis diagnosis before antibiotic administration, the time of lactate measurement, and the percentage of blood cultures obtained before antibiotic administration. Second, the student implemented a screening tool for the triage nurse to utilize to identify potential sepsis patients (with buy-in from the ED administrative staff and physicians). A process map of the screening tool is provided for review (Appendix F). Nurses, ED physicians, and ED technicians and secretaries were educated on the new screening process in shift change reports and with handouts so they were aware of the new process. Next, the student had the ED nurses utilize the new sepsis screening tool to prospectively flag sepsis patients and measured any improvement in recognition of the patient with sepsis and subsequently decrease door to diagnosis times, decrease the time from presentation to serum lactate measurement, decrease diagnosis to antibiotic times, and increase blood culture collection prior to antibiotic administration. The screening tool was utilized for a period of two months. Each patient was given an information sheet outlining the project and informing them what would be done with the information obtained during the study (Appendix G) Next, the student did a chart review for the 2-month period of screening tool implementation to determine if the screening tool was effective in decreasing door to diagnosis times, decreasing the time from presentation to serum lactate measurement, decreasing diagnosis to antibiotic times, and increasing blood culture collection prior to antibiotic administration.
The student partnered with the information technology department in the institution to analyze data for the project by utilizing the paper data collection tool (Appendix E). Outcomes performance measures to determine the project’s effectiveness include (a) reducing door to diagnosis times, (b) decreasing time from presentation to serum lactate measurement,(c) decreasing diagnosis to antibiotic times, and (d) increasing the number of blood cultures obtained before antibiotic administration. The student did a retrospective pre/post project implementation chart review to determine the amount of time it took for a lactate measurement and sepsis diagnosis before the screening tool compared to after the screening tool, as well as the time from diagnosis to antibiotic administration before and after implementation. The student additionally calculated the percentage of blood cultures obtained prior to initial antibiotic administration prior to and after project implementation. The overall goal of the project was to increase early sepsis recognition in the ED through utilization of early goal-directed therapy.
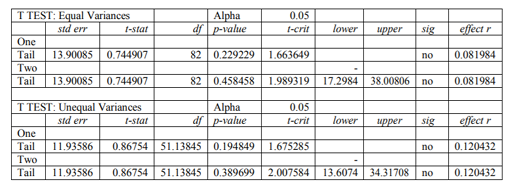
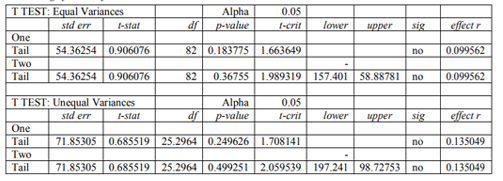
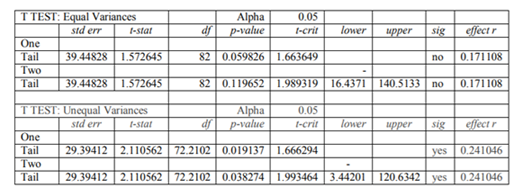
Paired sample t-tests were used to evaluate whether there was a reduction in door to sepsis diagnosis, door to lactate, and diagnosis to antibiotic times pre- and post- implementation. The Wilson Score Confidence Interval was used to compare the percentage of blood cultures collected before antibiotic administration pre-and post- implementation.
4. Results And Discussion
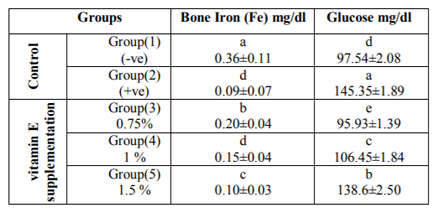
The study included 63 patients presenting to the ED before screening tool implementation, and 23 patients after implementation. There were no statistically significant differences in patient characteristics per period. Thirteen sepsis screening tools were completed in the two-month period of implementation. The data did not give sufficient evidence to conclude the screening tool decreased door to diagnosis time, door to lactate measurement, or increased the percentage of blood cultures obtained prior to antibiotic administration. The data did conclude a decrease in diagnosis to antibiotic administration (Tables 1-4).
The literature concludes sepsis outcomes can be enhanced though early recognition. The factors in this project have been studied extensively, and although the particular project did not correlate with the literature completely, with more time and data, the outcomes would likely match up.
The quality of care for sepsis patients can be increased by a relatively simple and inexpensive method such as the proposed screening tool. To further progress care for sepsis patients and improve early recognition of patients with sepsis in the ED setting, additional improvement activities and compliance with sepsis protocols put into action are required. An electronic screening tool would perhaps be more user-friendly and convenient for the nurses, since they had to remember to pull the paper screening tool each time a patient came in.
An early screening protocol utilizing the sepsis screening tool would also be beneficial. After speaking with the ED nurses in the project implementation institution, suggestions were made to make the paper tool an electronic version and tie it into the electronic health record the hospital uses. The nurses stated if the screening tool was in the computer and made a “required” point of the triage, there would be more compliance and accuracy with the tool.
5. Limitations
The study is limited in being an uncontrolled study in a single hospital. The short time frame for screening tool implementation also limits the potential. Only 13 screening tool were utilized during the two-month period of implementation, despite the fact there were 23 sepsis patients during that period. A paper screening tool may be viewed as an inconvenience for triage nurses, thus decreasing compliance rates. According to the information technology department at the hospital where the project took place, the components of the screening tool can be incorporated into the electronic chart to prospectively flag each patient meeting the criteria for sepsis, perhaps as an option in the future.
Since only providers can order antibiotics, the responsibility of that component lies with the provider. The screening tool, however, has the potential to empower the nurses to question about the need for antibiotic therapy earlier.
6. Conclusions/Significance To Advance Nursing Practice
A screening tool for early recognition of sepsis may lead to a decrease in door to antibiotic time. Sepsis is a life-threatening condition that impacts thousands of people each year. Evidence concludes early and assertive treatment in the ED can make a difference in patient outcomes (Vanzant & Schmelzer, 2011). The student’s project will make a difference in population outcomes by raising awareness of the condition early so treatment can begin in a timely manner, thus decreasing mortality rates from sepsis. The project could also impact the way care is implemented by increasing awareness of the signs and symptoms of sepsis and lessen the amount of time before action is taken.
Acknowledgements
I would like to thank the Institutional Review Board, nurses, ED providers, ED techs, ED unit assistants, and the rest of the ED staff from Sparks Health System for including the patients in the sepsis screening tool process, and for ensuring safe and effective care for sepsis patients presenting through the ED of the aforementioned institution. I would also like to thank Steward Huang, PhD for his help with statistical analysis of the project.
References
- Berger, T., Green, J., Horeczko, T., Hagar, Y., Garg, N., Suarez, A., … Shapiro, N. (2013). Shock index and early recognition of sepsis in the emergency department: Pilot study. Western Journal of Emergency Medicine, 14(2), 168-174. doi:10.5811.westjem.2012.8.11546
- Burney, M., Underwood, J., McEvoy, S., Nelson, G., Dzierba, A., Kauari, V., & Chong, D. (2012). Early detection and treatment of severe sepsis in the emergency department: Identifying barriers to implementation of a protocol-based approach. Journal of Emergency Nursing, 38(6), 512-517. doi:10.1016/ j.jen. 2011.08.011
- Calle, P., Cerro, L., Valencia, J., & Fabian, J. (2012). Usefulness of severity scores in patients with suspected infection in the emergency department: A systematic review. The Journal of Emergency Medicine, 42(4), 379-391. doi:10.1016/j/jemermed.2011.03.033
- DiCenso, A., Guyatt, G., &Ciliska, D. (2005). Evidence-based nursing: A guide to clinical practice (pp 166 & 519). St. Louis, MO: Mosby
- Hermans, M. A., Leffers, P., Jansen, L. M., Keulemans, Y. C., & Stassen, P. M. (2012). The value of the Mortality in Emergency Department Sepsis (MEDS) score, C reactive protein and lactate in predicting 28-day mortality of sepsis in a Dutch emergency department. Emergency Medicine Journal, 29(4), 295-300. doi:10.1136/emj.2010.109090
- Jones, A. E., Troyer, J. L., & Kline, J. A. (2011). Cost-effectiveness of an emergency department based early sepsis resuscitation protocol. Critical Care Medicine, 39(6), 1306-1312. doi:10.1097/CCM.0b01 3e31821201be
- Judd, W. R., Stephens, D. M., & Kennedy, C. A. (2014). Clinical and economic impact of a quality improvement initiative to enhance early recognition and treatment of sepsis. Annals of Pharmacotherapy, 48(10), 1269-1275. doi:10.1177/1060028014541792
- Lagu, T. Rothberg, M. B., Shieh, M., Pekow, P. S., Steingrub, J. S., &Lindenauer, P. K. (2012). Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003 to 2007. Critical Care Medicine, 40(3), 754-761. doi:10.1097/ccm.0b013e318232db65
- Kent, N., & Fields, W. (2012). Early recognition of sepsis in the emergency department: An evidence-based project. Journal of Emergency Nursing, 38(2), 139-143. doi:10.1016/j.jen.2010.07.022
- Nguyen, H. B., Ginkel, C. V., Batech, M., Banta, J., & Corbett, S. W. (2012). Comparison of Predisposition, Insult/Infection, Response, and Organ dysfunction, Acute Physiology And Chronic Health Evaluation II, and Mortality in Emergency Department Sepsis in patients meeting criteria for early goal-directed therapy and the severe sepsis resuscitation bundle. Journal of Critical Care, 27(4), 362-369. doi:10.1016/j.jcrc.2011.08.013
- Patocka, C., Turner, J., Xue, X., & Segal, E. (2014). Evaluation of an emergency department triage screening tool for suspected severe sepsis and septic shock. Journal for Healthcare Quality, 36(1), 52-61. doi:10.1111/jhq.12055
- Perman, S. M., Goyal, M., &Gaieski, D. F. (2012). Initial emergency department diagnosis and management of adult patients with severe sepsis and septic shock. Scandinavian Journal of Trauma, Resuscitation, and Emergency Medicine, 20(41), 1-11. doi:10.1186/1757-7241-20-41
- Puskarich, M. A., Illich, B. M., & Jones, A. E. (2014). Prognosis of emergency department patients with suspected infection and intermediate lactate levels: A systematic review. Journal of Critical Care, 29(3), 334-339. doi:10.1016/j.jcrc.2013.12.017
- Schaub, N., Boldanova, T., Noveanu, M., Arenja, N., Hermann, H., Twerenbold, R., … Mueller, C. (2014). Incremental value of multiplex real-time PCR for the early diagnosis of sepsis in the emergency department. Swiss Medical Weekly, 144(11), 1-10. doi:10.4414/smw.2014.13911
- Seymour, C. W., Rea, T. D., Kahn, J. M., Walkey, A. J., Yealy, D. M., & Angus, D. C. (2012). Severe sepsis in pre-hospital emergency care: Analysis of incidence, care, and outcome. American Journal of Respiratory and Critical Care Medicine, 186(12), 1264-1271. doi:10.1164/rccm.201204-07130C
- Society of Critical Care Medicine. (n.d.). About the Surviving Sepsis Campaign. Retrieved from http://www.survivingsepsis.org/About-SSC/Pages/default.aspx
- Sparks Health System. (2014). Mission, vision, and values. Retrieved from http:// www. sparks health.com/ about/mission
- Surviving Sepsis Campaign (n.d.) Severe sepsis chart review data collection tool for educational purposes. Retrieved from http:// www.survivingsepsis.org/SiteCollectionDocum ents/Data-Collection-Surviving-Sepsis.pdf
- Surviving Sepsis Campaign (2013). Evaluation of severe sepsis screening tool. Retrieved from http://www.survivingsepsis.org/SiteCollection Documents/ScreeningTool.pdf
- Tipler, P. S., Pamplin, J., Mysliwiec, V., Anderson, A., & Mount, C. A. (2013). Use of a protocolized approach to the management of sepsis can improve time to first dose of antibiotics. Journal of Critical Care, 28(2), 148-151. doi:10.1016/j.jcrc.2012.08.021
- Tromp, M., Hulscher, M., Bleeker-Rovers, C. P., Peters, L., van den Berg, D. T., Borm, G. F., … Pickkers, P. (2010). The role of nurses in the recognition and treatment of patients with sepsis in the emergency department: A prospective before-and-after intervention study. International Journal of Nursing Studies, 47(12), 1464-1473. doi:10.1016/ j.ijnurstu. 2010.04.007
- Turi, S. K., & Von Ah, D. (2013). Implementation of early goal-directed therapy for septic patients in the emergency department: A review of the literature. Journal of Emergency Nursing, 39(1), 13-19. doi:10. 1016/j/jen.2011.06.006
- Vanzant, A. M., &Schmelzer, M. (2011). Detecting and treating sepsis in the emergency department. Journal of Emergency Nursing, 37(1), 47-54. doi:10.1016/j.jen.2010.06.020
- Zhao, Y., Li, C., & Jia, Y. (2013). Evaluation of the Mortality in Emergency Sepsis score combined with procalcitonin in septic patients. American Journal of Emergency Medicine, 31(7), 1086-1091. doi:10.1016/j.ajem. 2013. 04.008