Information
Journal Policies
ARC Journal of Neuroscience
Volume-2 Issue-1, 2017, Page No: 14-16
PRES with First Time Seizure in a Newly Diagnosed HIV Patient:A Case Report
Burton Tabaac1*,Gregg Khodorov2
1.Rutgers Robert Wood Johnson University Hospital, Dept. of Neurology, USA.
2.Rutgers University, Robert Wood Johnson Medical School, USA
2.Rutgers University, Robert Wood Johnson Medical School, USA
Received : May 4, 2017
Accepted : May 19, 2017
Published : May 27, 2017
Citation : SBurton Tabaac, Gregg Khodorov. PRES with First Time Seizure in a Newly Diagnosed HIV Patient:A Case Report. ARC Journal of Neuroscience. 2017; 2(1):14-16.doi:dx.doi.org/10.20431/2456-057X.0201004
Copyright : © 2017 Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
A patient presents with altered mental status and encephalopathy status post a first seizure event. The initial brain MRI obtained showed radiographic evidence of posterior reversible encephalopathy syndrome (PRES). There was no evidence of a space-occupying lesion in the brain, and cryptococcal antigen was negative, suggesting that opportunistic infection was unlikely the etiology for the patient’s seizure. The patient was started on an antiepileptic drug (AED), and electroencephalogram (EEG) was negative for epileptogenic events; (EEG was conducted while on AED prophylaxis). The patient was observed to have a waxing and waning mental status during the hospital course. At times the patient was able to converse in full sentences, while on repeat examinations, he was nonverbal. The patient intermittently complained of hallucinations. A blood serum workup aided to confirm the diagnosis of HIV in the patient; he was not on any antiviral therapy prior to presentation. Unfortunately, the patient continued to exhibit signs of delirium, attributing to HIV encephalopathy. The patient ultimately expired during the hospital stay due to natural complications of the disease course.
Posterior reversible encephalopathy syndrome (PRES) is a neurological condition characterized by magnetic resonance imaging (MRI) findings of subcortical cerebral symmetric hemispheric edema typically found in parietal and occipital regions of the brain. Alternative names for this clinical condition include reversible posterior leukoencephalopathy syndrome, reversible posterior cerebral edema syndrome and hyperperfusion encephalopathy [1]. The current literature supports that the CT and MR imaging patterns for PRES closely correlate to the brain watershed zones, affecting white matter predominantly; the edema will usually reverse completely [1]. We document a case in which a 37 year old patient with newly diagnosed HIV presents with seizure and neuro pathological imaging suggestive of PRES. The PRES found in this case could not be attributed to hypertension, or to any pharmacological etiology.
Stroke, Cerebro vascular disease, Clinical neurology, HIV, MRI.
1.Case Presentation
We present the case of a 37-year-old man newly diagnosed with HIV only a week prior to admission after being found down in a bathtub by a family member. The patient was reported to be exhibiting suspected seizure activity, although the family member did not witness the fall or any convulsions. The patient reported syncopal events for several weeks leading up to the event. The patient had unknown family, social, past medical and surgical history, and was not taking any medications. Shortly after arrival to the emergency room, the patient was intubated for airway protection and given a loading dose of Keppra (levetiracetam). On physical examination, the patient was noted to exhibit a diffuse petechial rash. Neurological exam revealed a right gaze preference with visual field testing showing that the patient did not blink to threat bilaterally. Vestibulo-ocular testing was deferred as the patient was wearing a c-collar. Corneal and gag reflexes were intact. On tone testing, the patient was noted to have increased tone (right upper extremity greater than left) and in bilateral lower extremities. Throughout the examination, the patient exhibited intermittent transient shivering-like activity, albeit no tonic posturing, clonic movements, flexion nor extension was observed. On sensation testing, the patient localized noxious stimuli on sternal rub using the right arm. The patient did not withdraw or respond to noxious stimuli on the left.
The patient had a CT scan of chest, abdomen, and pelvis in the emergency department which revealed trace pelvic free fluid, and a miliary pattern of the bilateral lungs, predominantly lower lung fields, and prominent bilateral supraclavicular mediastinal and hilar lymph nodes. CT scan of head only showed pansinusitis; no hemorrhage, acute stroke, nor mass effect. Initial EEG testing revealed the patient in a drowsy vs. coma state with diffuse background 8Hz theta and 1.5 Hz delta slowing and disorganization of background frequencies seen. This study was read as indicative of moderate diffuse cerebral dysfunction. Continuous attenuation of faster activity was seen over the right temporal region, indicative of mild focal cerebral dysfunction likely structural in etiology affecting neocortical structures A long term video EEG further detailed infrequent periods of frontally-predominant, semi-rhythmic 1.5 Hz delta activity seen and attenuation of amplitude seen in the bi-occipital regions.
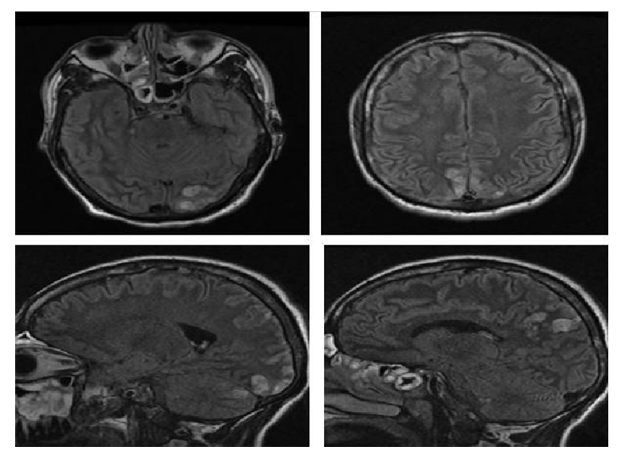
MRI of the brain with and without contrast (Image 1) included sagittal and axial FLAIR images. These sequences demonstrated bilateral high signal in the parietal cortex and in the left occipital cortex. There was also a focus of high signal in the posterior superior aspect of the left thalamus. Following neither contrast demonstration there was no abnormal enhancement nor restricted diffusion visualized. The MRI report interpreted the findings of bilateral posterior cortical high FLAIR signal as most likely representative of posterior reversible encephalopathy syndrome.
Shortly after being admitted a Code BLUE was called for the patient as he was found to be in respiratory distress and pulse less. The patient was subsequently intubated and given IV atropine x 1, IV epinephrine x 5, IV bicarbonate x 1, and Dextrose 50. Return of spontaneous circulation was obtained 20 minutes after the code was initiated. The patient was then started on Levophed and transferred to the MICU. In the ICU the patient developed bradycardia (down to the 40s) and was pulse less. A second Code BLUE was called during which the patient expired.
2. Discussion
Only a week after initial HIV diagnosis, this 37-year-old patient found himself admitted to the ER after a fall in his bathtub which left him unconscious. This report documents the workup which led to eventual diagnosis of posterior reversible encephalopathy syndrome due to HIV.
PRES has been reported in patients with advanced HIV disease on only a few occasions [2]. Among the reported cases, PRES more commonly manifests secondary to the administration of therapies relating to the patient’s symptomatic expression. For instance, antiretroviral therapy has been observed to cause PRES [3-5]. Alternatively, HIV patients receiving non-HIV-related treatment that results in additional immunosuppression, have also been reported [6-9]. PRES due to the actual immunosuppression of HIV, without the administration of HIV therapy is much less well-documented [1-11]. Among these latter reported cases not involving therapeutic medical administration, two cases included a diagnosis of end stage renal disease (ESRD), which likely contributed to the etiology of PRES [10,11].
According to Geurriero et al., [3] two potential pathophysiological explanations exist for causing PRES in this case report. First, a sudden elevation in systemic blood pressure surmounts auto regulatory brain circulation, leading to vasodilation/vasoconstriction of the arteries. This is postulated to cause transudation of fluid focally which may lead to petechial haemorrhages. Albeit, there was no documented hypertension in this case. Another potential patho physiology of PRES is that hypercalcemia adversely affects endothelium-independent vasodilation, leading to microvascular leakage; however, the patient’s calcium levels were within normal limits.
Although PRES has been shown to improve in patients with HIV (e.g., Saeed et al [4]), the outcome is most likely dependent on the both severity of HIV infection and the progression of the edema and neurological symptoms associated with PRES. In this case, marked improvement was not noted in the patient prior to expiration. PRES should be included as a differential in patients who are immunosuppressed and present with focal neurological signs. If the cause of PRES is left unaddressed, the condition has the potential to increase morbidity and mortality.
References
- Bartynski, W. (2008). Posterior Reversible Encephalopathy Syndrome, Part 1: Fundamental Imaging and Clinical Features. American Journal of Neuroradiology, 29(6), 1036-1042. doi:10.3174/ajnr.a0928
- Ribeiro, S., Monteiro, M., Moreira, B., & Franca, M. (2013). Rare posterior reversible encephalopathy syndrome in a patient with HIV. Case Reports, 2013(Nov19 1). doi:10.1136/bcr-2013-201495
- Guerriero S, Ciracì L, Dicuonzo F, et al. Bilateral Visual Loss as Presenting Symptom of Posterior Reversible Encephalopathy Syndrome in a Patient with HIV/Tuberculosis Coinfection: A Case Report. Case Reports in Ophthalmological Medicine [serial online]. January 1, 2012; 2012:850176. Available from: Africa-Wide Information, Ipswich, MA. Accessed July 1, 2016.
- Saeed M, Dacuycuy M, Kennedy D. Posterior reversible encephalopathy syndrome in HIV patients: case report and review of the literature. AIDS (London, England) [serial online]. March 30, 2007; 21(6):781-782. Available from: MEDLINE, Ipswich, MA. Accessed July 1, 2016.
- Vicente Giner, Conrado Fernández, Maria José Esteban, Maria José Galindo, Maria José Forner, José Guix, Josep Redón, Reversible posterior leukoencephalopathy secondary to indinavir-induced hypertensive crisis: A case report, American Journal of Hypertension, Volume 15, Issue 5, May 2002, Pages 465-467, ISSN08957061.
- Sasson S, Oon A, Brew B, Carr A, Chagantri J. Posterior reversible encephalopathy syndrome (PRES) in an HIV-1 infected patient with disseminated varicella zoster virus: A case report. BMC Infectious Diseases [serial online]. August 23, 2013;13(1) Available from: Scopus®, Ipswich, MA. Accessed July 1, 2016.
- Stevenson J, Taylor C. Posterior reversible encephalopathy syndrome in disseminated histoplasmosis and advanced HIV infection. International Journal of STD & Aids [serial online]. n.d.; 25(8):611-613. Available from: Science Citation Index, Ipswich, MA. Accessed July 1, 2016.
- Courand P, Christin F, Ben Cheikh A, Baillon J, Ber C, Rimmele T. Posterior reversible encephalopathy related to tacrolimus in a liver transplanted HIV patient. Gastroenterologie Clinique Et Biologique [serial online]. n.d.; 34(1):29-34. Available from: Science Citation Index, Ipswich, MA. Accessed July 1, 2016.
- Chang O, Stanculescu A, Dola C, Rothwell W. Recurrent posterior reversible encephalopathy syndrome potentially related to AIDS and end-stage renal disease: a case report and review of the literature. Case Reports In Medicine [serial online]. 2012; 2012:914035. Available from: MEDLINE, Ipswich, MA. Accessed July 1, 2016.
- Kurukumbi M, Castellanos M, Crawford A, Gowdar S, Jayam-Trouth A. Posterior Reversible Encephalopathy Syndrome in a Patient with Newly Diagnosed HIV Infection and End Stage Renal Disease. Case Reports In Neurological Medicine [serial online]. January 2013;:1-5. Available from: Academic Search Premier, Ipswich, MA. Accessed July 1, 2016.
- Mohankumar K, Maria I. C, Amanda K. C, Shreyas D. G, Annapurni J. Posterior Reversible Encephalopathy Syndrome in a Patient with Newly Diagnosed HIV Infection and End Stage Renal Disease. Case Reports In Neurological Medicine [serial online]. 2013; Available from: Directory of Open Access Journals, Ipswich, MA. Accessed July 1, 2016.