Information
Journal Policies
ARC Journal of Nephrology
Volume-4 Issue-1, 2019, Page No: 1-6
The Outcomes of Patients Undergoing Radical Cystectomy for Small Cell Bladder Cancer (SCBC): A Single Centre Experience
Simon Robinson>1*, Ailsa Butler2, Hanif Motiwala3
1.Associate Specialist, Heatherwood and Wexham Park Hospital NHS Foundation Trust.
2.Dept Epidemiology University of Oxford.
3.Consultant Urologist, Heatherwood and Wexham park hospital NHS foundation trust.
2.Dept Epidemiology University of Oxford.
3.Consultant Urologist, Heatherwood and Wexham park hospital NHS foundation trust.
Citation : Simon Robinson, Ailsa Butler, Hanif Motiwala, "The Outcomes of Patients Undergoing Radical Cystectomy for Small Cell Bladder Cancer (SCBC): A Single Centre Experience" ARC Journal of Nephrology. 2019; 4(1) : 1-6.
Copyright : © 2019 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract:
To review the literature of small cell bladder cancer (SCBC) and to compare those patients who had radical cystectomy with those having surgery for transitional cell carcinoma of the bladder.
1. Introduction
SCBC is a rare (< 1% of all bladder tumours) and aggressive form of bladder cancer. it shows similar behaviour to lung small cell cancer and is indistinguishable histologically. SCBC is from a family of neuroendocrine tumours, and is the most common epithelial subtype, that can affect the respiratory, gastrointestinal and genito-urinary tracts. Other neuroendocrine tumours include carcinoid and large cell carcinoma.
Untreated, it has a very poor prognosis with a 5 year survival less than 5% [1] due to high metastatic potential and lack of symptoms in early stage of the disease. Oncological surgery remains the most effective treatment. Systemic treatment can improve outcome.
The tumour is often mixed with urothelial cancer. Any component of SCBC drives the overall behaviour. Treatment usually involves a chemotherapeutic regime, which may be in addition to oncological surgery which should be offered to all non metastatic disease patients.
2. Methods
Papers were identified by searches of PubMed using the terms “small cell” “bladder” and “carcinoma”. Additional papers were identified from review of references of relevant articles.
3. Study Population
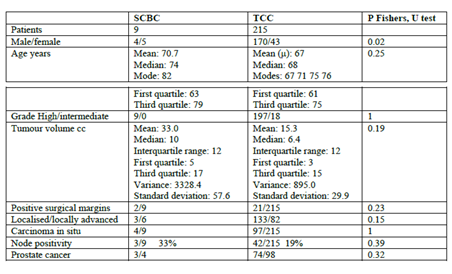
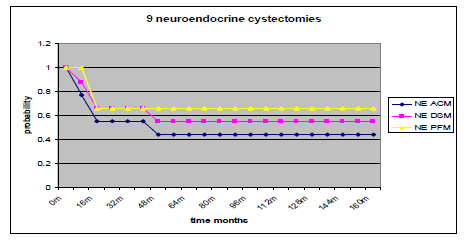
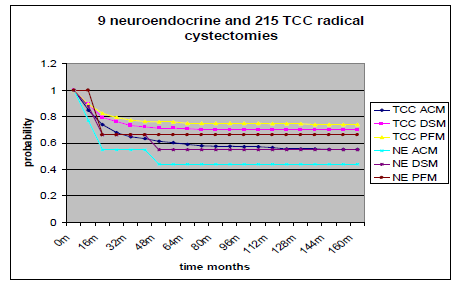
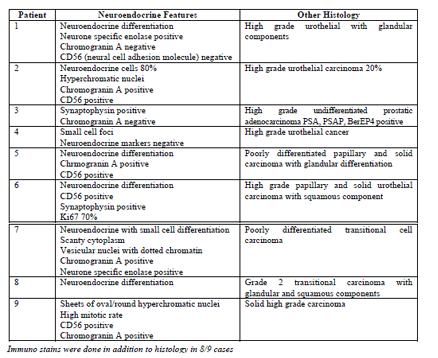
We reviewed retrospectively 258 patients having radical cystectomy from 1999 to 2013 and found 9 patients with neuroendocrine or small cell cancer (3%). Patients were considered to have SCBC if the histology showed any small cell component. We have emphasised stage, tumour volume, progression free survival (looking at local recurrence and metastasis) and compared these with patients having cystectomy for transitional cell carcinoma of the bladder. Our literature search has not shown any other study making this direct comparison.
4. Tumour Characteristics
Pathology was reviewed using TNM classification. We compared the clinical and pathological outcomes of these patients to those with solely transitional cell cancer. Multimodal therapy included 2 pts missing
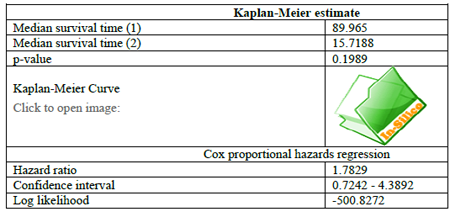
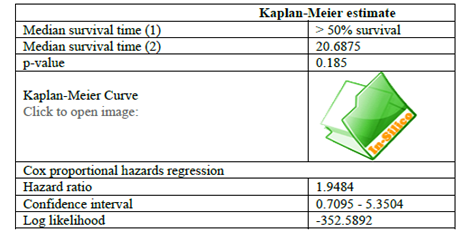
Graph pad Fishers exact test, Mann Whitney U tests, Kaplan Meier curves
5. Results
6. Discussion
This is a rare tumour forming less than 1% of all urological malignancies. The tumours are usually mixed with any small cell component felt to drive the overall aggressive behaviour of the tumour. It is one of the most common sites of extrapulmonary small cell cancer [2]. Given that this a rare disease, there have been no standard treatment regimes and extrapolation has been implemented from bronchogenic small cell cancer. Often a chemotherapeutic regime using a platinum based agent is involved, as an adjuvant treatment after oncological surgery. It seems that this improves outcomes especially for localised disease.
It is a smoking related cancer with a male predominance. Usually patients present in the sixth or seventh decade.
The origin of the tumour is unclear. Perhaps a transformation from a bladder neuroendocrine cell or from a stem cell element [3]. There are a variety of chromosomal deletions seen in SCBC that are also seen in small cell cancer of the lung [4] suggesting a commonality in aetiology. There is also hypermethylation of tumour suppressor genes and amplification of oncogenes.
The tumour is composed of sheets of round and spindle cells with little cytoplasm. The nuclei are hyperchromatic with a a high mitotic rate and a “salt and pepper” chromatin [5]. The tumour is usually mixed with other urological tumours seen, urothelail, squamous and adenocarcinoma.
Immunohistochemcial stains are used to support the diagnosis of SCBC such as chromogranin A, synaptophysin, serotonin and neurone specific enolase. Perinuclear dot like immunoreactivity may be identified for cytokeratins [6]. The finding of numerous positive markers supports the diagnosis although light microscopy remains the gold standard. Given the stains are not specific for site of tumour origin, metastatic spread from other sites must always be excluded.
Untreated the 5 survival is less than 10% [1]. Limited stage shows a better prognosis than extensive stage [7]. Surgery, even for limited disease, may be inadequate [8,9]. It has been reported that cis platin based chemotherapy is the only factor predicting survival [10] although others have not found this to be the case [11] yet neoadjuvant regimes were effective. There is no standardised regime, etoposide, cyclophosphamide, doxorubicin, gemcitabine and vincristine all have been employed. Nevertheless oncological surgery is almost certainly the principal treatment for successful eradication of this disease [12]. Lymph node disease is common despite neoadjuvant treatment [13].
Multimodal TURBT, chemotherapy and radiation noted a higher relapse rate [14]. Chemotherapy alone gives a clearly inferior result [15] as does radiotherapy alone.
The treatment and survival varies among groups. A 15 year review of the Anglia Cancer Network revealed only 20 patients and only 3 had surgery. The median survival overall was 33 months for those receiving chemotherapy and 3 months for those not receiving chemotherapy [16]. The median survival for the Mayo group, who had 44 patients, was 1.7 years. They had a cure rate of 6/8 for stage 2 SCBC illustrating further that long term survival can be achieved with localised disease. Other institutions report small case series with a poor median survival of 7 months [17] or 34 months [18]. The MD Anderson cancer centre with 25 patients treated with cystectomy only yielded a 5 year survival of 36% [11], those 21 patients who had neoadjuvant chemotherapy had a 78% cancer specific survival.
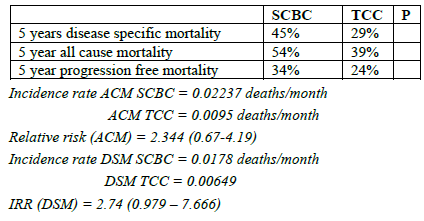
We had a majority of 5 female patients in our SCBC population which is unusual for this bladder tumour (P=0.02) which represented 3.4% of all the 258 radical cystectomies performed at our institution from 1999 to may 2013. The patients were not significantly older from the bulk of patients with transitional cell cancers of the bladder. All the tumours were high grade and larger than the TCC although not reaching statistical significance. All patients had muscle invasive disease and the majority, 6/9 cases, had locally advanced disease. There was no difference in the positive surgical margin rate. There was no significant difference in the carcinoma in situ or coincidental prostate cancer rates. Only 3 cases had nodal involvement but this was not significantly different from the TCC rate. Only 2 patients received adjuvant chemotherapy in the SCBC group compared to 36 in the TCC group (P = 0.6). Both patients who had adjuvant chemotherapy with gemcitabine and carboplatin have died. A total of 5 of 9 pts have died.
Three developed distant metastasis rather than local recurrence. The sites were in the bone and lung. All three showed progression at about a year with death occurring 3 months later in 2 cases. The patient with lung metastasis survived 32 months after progression was detected.
1. bone metastasis at 10/12 rip 15/12.
2. bone and node metastasis 13/12 rip 16/12
3. lung metastasis 10/12 rip 42/12 IHC at least one marker is usually positive for these tumours [19].
7. Conclusions
Outcomes for SCBC may be improving with the use of neoadjuvant chemotherapy, although in our series none received this and the two patients who received adjuvant chemotherapy both died. Four of our patients are alive and two have shown long term survival at 75 and 58 months post surgery, neither of whom received chemotherapy of any sort. Two of our patients have missing records.
References
- Abbas Small cell cancer of bladder and prostate Urology 1995 46:617
- Galanis Extrapulmonary small cell cancer.Cancer 1997;79:1729-36
- Ismaili Outcome of recurrent and metastatic small cell carcinoma of the bladder BMC Urol.2009;9:4
- Peterson Small cell lung cancer is characterised by a high incidence of deletions on chromosomes 3p, 4q, 5q, 10q, 13q and 17p. Br J Cancer. 1997;75:79-86
- Abrahams Small cell carcinoma of the bladder: a contemporary clinicopathological study of 51 cases. Histopathology. 2005; 46:57-63
- Cheng Oat cell carcinoma of urinary bladder. Urology .1992;39:504-7
- Kalaiah Small cell carcinoma of the bladder among patients in the Veterans Affaris Health System. ASCO Genitourinary Cancer Symposium .2010;abstr 303
- Holmang Primary small cell cancer of the bladder: a report of 25 cases J Urol 1995; 153:1820-2
- Choong Small cell carcinoma of the urinary bladder. The Mayo clinic experience. Cancer.2005;103:1172-8
- Mackey Genitourinary small cell cancer: determination of clinical and therapeutic factors associated with survival. J Urol 1998; 159:1624
- Siefker Evidence supporting preoperative chemotherapy for small cell carcinoma of the bladder: a retrospective review of the M.D Anderson cancer experience. J Urol. 2004; 172:481-4
- Fahed Small cell bladder cancer: Biology and management. Seminars in oncology, vol 39, No5, October 2012,pp615-8
- Alva outcomes following neoadjuvant chemotherapy and cystectomy in localised small cell bladder cancer: the university of Michigan experience (abstract) ASCO Genitourinary Cancer Symposium 2010;287
- Lohrisch Small cell carcinoma of the bladder.Cancer.1999;86:2346-52
- Sved Small cell carcinoma of the bladder. BJU int.2004;94:12-7
- Mukesh Small cell carcinoma of the urinary bladder: a 15 year retrospective review of treatment and survival in the Anglian Cancer Network BJU int mar;103(6):747-52
- Ruoppolo Neuroendocrine small cell bladder cancer: our experience Urologia 2010 oct- dec;77 Suppl 17:64-71
- Analysis of treatment for small cell cancer of the bladdr and report of three cases Karpman Urology 2004 sep;64 (3):494-8
- Trias Small cell carcinoma of the urinary bladder Eur Urol 2001;39:85-90