Information
Journal Policies
In Patients with Newly Diagnosed Membranous Nephropathy in Advanced Age, for the Differential Diagnosis of Cancer-Related MN, Should Anti-PLA2R be Routinely Considered?: Case Report
Sultan Ozkurt1*, Mustafa Fuat Acikalin2
2.Department of Pathology, Eskisehir Osmangazi University Medical Faculty, Eskisehir, Turkey.
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Membranous nephropathy (MN) is one of the most common presentations of nephrotic syndrome in adults. MN related cancer incidance increases with age and it is known that cancer frequency above age 60 is around %20-25. Malignancy research in newly diagnosed MN has become a standard application. However there is no consensus among clinicians about when to search aggressively for malignencies. Some serological and pathological findings are known to be cancer related an done of these is the phospholipase A2 receptor (Anti-PLA2R) antibody absence. According to latest literature information, MN is most frequently accompanied by lung, prostate and hematological malignencies. Newly diagnosed elderly patients with the absence of Anti-PLA2R antibodies in their circulation, must be evaluated thoroughly for occult malignancy. We are reporting a anti-PLA2R negative 65 years old male nephrotic sydrome patient who was diagnosed with prostate adenocarcinoma while being scanned for maligencies and achieved complete nephrotic syndrome remission upon surgical procedure of said malignancy.
Membranous nephropathy, prostate carcinoma, phospholipase A2 receptor antibody,Nephrology
1. Introduction
Membranous nephropathy (MN) is one of the most common nephrotic syndrome causes and it is characterized by glomerular basal membrane thickening under light microscopy[1]. %75 of the cases are idiopathic and the other causes related to MN are infections, malignancy, autoimmun diseases and drug toxicity [2]. The relation between MN and cancer has been known since 1996 and in a recent study this relationship’s prevelance has been reported as %10[3]. The cancer incidence related with MN increases with age and it is reported that cancer frequency is %20-25 after 60 years of age [5]. Before having diagnosis of MN, only %20 of the patients have cancer before and at rest of them cancer is detected during evaluation of MN or following years [4]. It has been standard to search for malignancy at elderly patients when diagnosed MN and no secondary cause is found. However there has been no consensus about when and how to search for occult malignancy.
2. Case
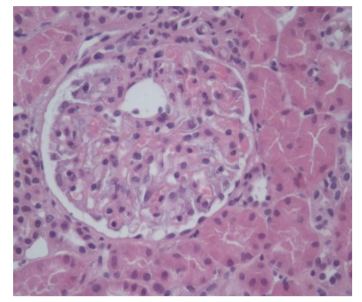
65 years of man who has no chronic illness history, was admitted to family medicine for pretibial oedema for 2 months at November 2017. Protienuria (+++) was detected and he was directed to our hospital. At the admission, blood pressure was 120/80 mmHg , respiratory sounds were normal, at abdomen examination no organomegaly was detected and pretibial ++/++ oedema was present. At history no coughing, loss of weight, night sweating, prostatism symptoms, constipation, change of defecation were present. At laboratory tests; hemoglobin14.4g/dl, leucocyte 6.7 103/ul, platelet 285 103/ul, erythrocyte sedimentation rate : 78mm/h,C reactive protein:0.334 mg/dl,Na:141 mEq/L, K:4.86mEq/L, glucose 85 mg/dl, blood urea nitrogen :14 mg/dl, creatinin 0.83mg/dl, total protein 4.7 g/dl, albumin 2.1 g/dl, triglyserid: 220 mg/dl, LDL: 297 mg/dl, liver function tests were normal,at urine analyses: protein(+4), erythrocyte 1/HPF, leucocyte 1/HPF, at spot urine protein/kreatinin ratio: 6157 mg/day, hepatitis B surface antigen:negatif, hepatitis C antibody negatif, HIV antibody :negatif, anti nuclear antibody:negatif, Anti-DoubleStranded DNA (Anti-dsDNA) :negatif, complemant C3 and C4 normal, serum protein electrophoresis: no monoclolonal peak,tiroid function tests were normal, chest X-ray and abdomen ultrasonography were nromal. Renal biopsy was performed with diagnosis of nephrotic syndrome, at biopsy 25 glomerules was deteceted and three of them had obselacance appearance. At other glomerules, capillary wall thickening and mesengial matrix increase were detected (Figure 1). Crystal violet and Congo red dye were negative. No additional finding was detected with PAS, metanamin, silver and trichrome dyes. In immun florecence investigation at glomerular capillary walls; strong with IgG, moderate strong with C3c, light granular positivity with C1q, kappa and lambda, negative IgA, Ig M ve fibrinogen were reported. Due to patient who has membranous nephropathy is elderly, to distinguish primary and secondary disease Anti-PLA 2R was studied and it was negative. Cancer scanning was started after exclusion of other secondary causes like drug, infection and autoimmun diseases.
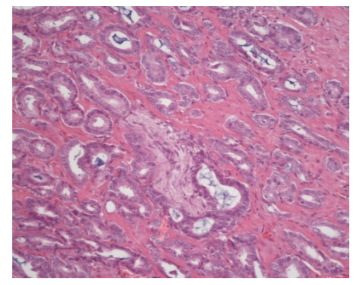
Tumor indicators; prostate-specific antigen(PSA):5.68 ng/ml (0.4-1), free PSA: 0.921, carcinoembryonic antigen (CEA): 2.37ng/ml(0-5), Alfa-fetoprotein (AFP):2.31 IU/ml(0.5-5,8), CA 19.9: 1.09(0-27). For increased PSA levels, urology suggested to perform prostat biopsy. Pathology of biopsy was prostatic adenocarcinoma. No metastasis was detected at abdomen-thorax tomography and positron emission tomography (PET) scanning. Radical prostatectomy was performed by urology and at pathology report; surgical borders were intact, there was no lymphatic invasion but perineural invasion was present (Figure 2). At laboratory findings 3 months after surgery; PSA< 0.003, serum creatinin 0.8 mg/dl, serum albumin 4.1 g/dl, spot urine protein/creatinine ratio: 135 mg and the patient was evaluated as complete remission.
3. Discussion
At case reports, while carcinoms were the most common tumors related with MN, prostat cancer and MN relation was rarely reported [6]. Firstly, Lefaucheur et al. reported at 2006, that lung and prostat cancers are the most MN related cancers [5]. These findings were confirmed at systematic review and metaanalyses by Leeaphornve et al[4]. This situation was explained with prostat cancer was not able to be detected in the past due to lack of serologic markers and recently PSA has been controlled systematically at elderly men. At the same study, it was found that half of the patients who have MN diagnosis, have no tumor symptoms like cough or urine retention ; risk of cancer is still present after 5 years of diagnosis [5]. Thus; as our case, elderly patients who have MN diagnosis are not be able to have cancer symptoms at the time of diagnosis and occult cancers should be investigated or patients should be followed up. Cancers incidence increases with age and similarly MN related cancer incidence increases with age too [4]. Thus to suggest a direct relation between cancer and renal diseases is not always true. The classical clinical criteria to support this relation is dissapperance of renal disease when tumor is removed and reccurence of MN when tumor relapses. In our case, total resolution of nephrotic syndrome after curative resection of cancer supports the idea of MN is related to cancer. We cannot make any comment about cancer recurrence and MN progression since we do not know anything long term of cancer course yet. It has become standart to search for malignancy in newly diagnosed MN patients when secondary causes are excluded. But there is no consensus about in which cases, agrressive investigation of occult malignancy should be performed. Some serologic and pathologic findings can give a hint. First of them is precence of antibodies against transmembrane glycoprotein M type Phospholipase A2 (PLA 2R) described as major target podocyte antigen receptor and which are related to adult idiopathic MN. These antibodies can be helpful to distinguish idiopathic or secondary MN. When Anti-PLA 2R is detected there no risk of malignancy but lack of Anti- PLA 2 R increases cancer relation risk of MN and in this cases cancer investigation should be perform carefully [7]. Secondly, Lefaucher et al. reported that presence of more than eight inflammatory cells infiltrating glomerules increase possibility of cancer [5]. The third finding that suggests the risk of cancer is strong immuneflorecence staining of glomerular PLA2R IgG1 and IgG2. This situation is seen in MN related to cancer however IgG4 deposits support idiopathic MN. In our patient, lack of Anti- PLA2R directed us to search for cancer. Thus we suggest Anti- PLA 2R study to make distinction of primary and secondary MN when no enough histological finding is get in elderly patients.
In conclusion, it is necessary to make more investigation to find the real cancer incidence in MN cases who have similar serologic and glomerular morphological findings above. It is logical to perform agrresive cancer scanning in patients who have these findings until these knowledge is get. Based on the studies that show increased incidence of prostate and lung cancer among MN patients, firstly systemic investigation for prostate and lung cancer should be performed.
References
- Swaminathan S, Leung N, Lager DJ, Melton LJ 3rd, Bergstralh EJ, Rohlinger A, Fervenza FC: Changingincidence of glomerulardisease in OlmstedCounty, Minnesota: a 30-year renal biopsystudy. Clin J Am SocNephrol 2006; 1: 483-487.
- Ponticelli C, Glassock RJ: Glomerular diseases: membranous nephropathy - a modern view. Clin J Am SocNephrol 2014;9:609-616.
- Lee JC, Yamauchi H, Hopper J Jr: Theassociation of cancer and the nephrotic syndrome. AnnInternMed 1966;64:41-51.
- Leeaphorn N, Kue-A-Pai P, Thamcharoen N, Ungprasert P, Stokes MB, Knight EL. Prevalence of cancer in membranous nephropathy: a systematic review and meta-analysis of observational studies. Am J Nephrol. 2014;40(1):29-35. doi: 10.1159/0003 64782.
- Lefaucheur C, Stengel B, Nochy D, Martel P, Hill GS, Jacquot C, Rossert J, GN-PROGRESS StudyGroup: Membranous nephropathy and cancer: epidemiologic evidence and determinants of high-risk cancer association. KidneyInt 2006;70:1510-1517.
- Eagen JW. Glomerulopathies of neoplasia. KidneyInt 1977; 11: 297–303.
- Timmermans SA, Ayalon R, vanPaassenP,Beck LH Jr, vanRie H, Wirtz JJ, Verseput GH,Frenken LA, Salant DJ, CohenTervaert JW, Limburg Renal R: Anti-phospholipase A2 receptor antibodies and malignancy in membranous nephropathy. Am J KidneyDis 2013;62: 1223–1225.