Information
Journal Policies
Bilateral Renal Lymphangiectasia Associated with Pleural Effusion in an Egyptian Patient: A Case Presentation & Literature Review
Alaa Sabry*, Rasha Samir, YaraMoheb
Copyright : © 2018 . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Renal lymphangiectasia is a very rare disorder where there is dilatation of perirenal, peripelvic and intrarenal lymphatics. This condition, congenital or acquired, is probably caused by an alteration of renal lymphatic drainage to retroperitoneal lymph ducts. Although the exact etiology remains unknown, an obstructive process resulting from several causes, including infection, inflammation or malignant infiltration, has been suggested to be responsible for the acquired form. Symptoms and radiologic findings are well defined.
1. Introduction
Present case describes a 28-year-old Egyptian male, with unremarkable medical history and there is none with respect to the family. The patient was hospitalised for evaluation of loin pain which was more on the right side, discovered to have bilateral renal lymphangiectasis and pleural effusion to have right sided pleyral effusion. Percutaneous drainage and sclerotherapy with a 10F catheter was carried out for 21 days. Daily povidoneiodine washing was performed for 20 days. The clinical result was excellent and follow up Ct revealed no recurrence.
2. Case Report
This case report describes a 28-year-old Egyptian man. His medical history was unremarkable, and there was no pertinent family history. In December 2015, he was admitted to the hospital for evaluation of loin pain which was more marked on the right side with no specific precipitant or radiation. The patient also complained of easy fatigability with dyspnea on exertion. Physical examination showed a blood pressure, respiratory rate, body temperature, heart rate and SaO2 of 120/80 mmHg, 15 breaths/minute, 37°C, 82 bpm and 96%, respectively. Adistended abdomen with diminished intensity of breath sounds on both lung bases more on the left side was the only abnormality discovered.
The patient was subjected to investigations. Urine analysis was done with no reported abnormalities. Blood tests showed high creatinine level reaching 1.55 mg/dl, estimated glomerular filtration rate (eGFR) was 68 ml/min/1.73 m².
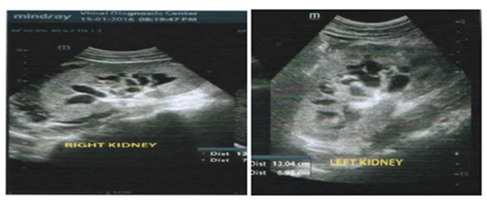
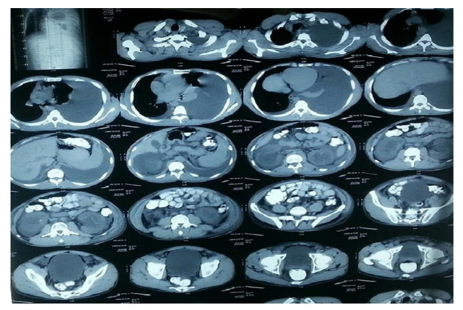
Chest x ray revealed mild to moderate left sided pleural effusion (Figure1). Abdominal ultrasonography (Figure2) revealed Right perinephric collection of fluid density totally encasing the kidney. This radiographic finding was then confirmed by a subsequent CT scan (Figure3) showing the previously reported right sided perinephric collection extending into surrounding pararenal space, pericaval and para aortic space, and also insinuating in the hepato renal pouch and encasing the related small bowel loops, associated with intra renal, peripelvic cystic like lesion. The intrarenal excretory systems were distorted by the peripelvic cystic structures. Ascites was also found making a provisional diagnosis of bilateral renal lymphangiectasia. History of trauma was denied.
3. Statistical Analysis
Continuous variables are expressed as mean and 95% CI, or as median and interquartile range, depending on the distribution of the data. For the description of categorical variables, the number and percentage of patients per response category have been used.
We compared variables between groups using ANOVA tests in continuous variables or the equivalent for non-parametric variables, depending on the inherent characteristics for each study variable, and McNemar tests for analysing categorical variables from related samples.
Recipient, graft survival, and patients on m-TOR monotherapy were studied using Kaplan-Meier survival curves. All statistical analyses were carried out using SPSS statistical software, version 19.0. In all statistical tests applied to the study variables, a statistical significance (α) of 0.05 was considered.
Mild to moderate left sided pleural effusion with underlying atelectatic band.
- Bilateral intrarenal peri pelvic non communicating cystic lesion, Increase parenchymal echogenicity at both sides with poorcortico-medullary differentiation.
- Bilateral peri-nephric fluid collection of altered echogenicity, more at right side.
- Marked left sided pleural effusion with underlying lung collapse & mediastinal shift to the right side.
- Minimal right sided pleural effusion.
- Right perinephric collection of fluid density totally encasing the kidney, it is extending into surrounding pararenal space, pericaval& para aortic space.
- It is also insinuating in the hepato renal pouch & encasing the related small bowel loops.
- It is also associated with intra renal, peri-pelvic cystic like lesion.
- Similar changes are seen at left renal fossa.
Other laboratory investigations includes Immunologic markers as anti-nuclear antibody (ANA), rheumatoid factor (RF) and anti-neutrophil cytoplasmic antibody (ANCA) were negative with normal levels of the complement components. Serum protein electrophoresis was done and it was also normal. Follow up Urine analysis was persistently normal with serum creatinine of 1.6 mg/dl.
Perinephric fluid aspiration was done showing the following characteristics:
- Gross appearance: Clear fluid, Chemical Examination: Creatinine: 1.2 mg/dl, Protein: 2.4 mg/dl, Glucose: 91mg/dl, TG: 420 mg/dl, LDH: 200 IU/l, No organism was isolated from aspirated fluid. It was unremarkable for Gram stain and cultures.
- Cytological examination showed few small sized lymphocytes, few methoselial cells. No atypical or malignant cells.
The aspirated fluid analysis confirmed the radiographic suggestion of bilateral renal lymphangiectasis. On the basis of clinical, imaging and laboratory investigations, the diagnosis of renal lymphangiectasia was made.
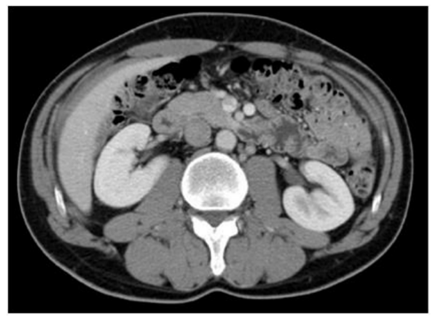
Surgical treatment was not possible because of the patient’s general condition, after getting a Patient consent, percutaneous drainage and sclerotherapy with a 10F catheter was carried out for 21 days. Daily povidoneiodine washing was performed for 20 days. The clinical result was excellent after the evacuation of 4 L of fluid. No complication was noted during the hospital stay and at follow-up 2 months later; a CT-scan (Figure 4) revealed no recurrence with good renal function.
The patient was advised to undergo serial kidney function tests and imaging follow-up.
3. Discussion
Lymphangiectasia is a pathologic dilation of lymph vessels which may be congenital or acquired caused by granulomas or cancer causing lymphatic obstruction, or increased central venous pressure (CVP) causing abnormal lymph drainage [1]. It has with no gender or age predilection.
The nomenclature of this disorder is confusing and has evolved in recent years. Other names haveincluded “renal lymphangiomatosis”, “renal lymphangioma”, “peripelviclymphangiectasia”, and “renal peripelvic multicysticlymphangiecta sia”. “Renal lymphangiectasia” is the preferred name, given that the disorder is characterized by ectaticperirenal, peripelvic, and intrarenal lymphatic vessels [2].
Renal Lymphangiectasia (or renal lymphangioma), is very rare benign lymphatic malformation, where there is dilatation of intrarenal, perirenal and peripelviclymphatics.
The lymphatic drainage of the kidney, renal capsule, and perinephric tissues intercommunicate through several large lymphatic trunks within the renal sinus. These renal lymphatic trunks drain into the paraaortic, paracaval, and interaortocaval lymph nodes [3].
Renal Lymphangiectasia It is due to the failure of the perirenal lymphatic tissue to form normal communications with the remainder of the lymphatic system.
This leads to the dilation of lymphatic vessels and to the formation of unilocular or multilocular cystic masses in the perirenal area.
A total of 56 cases were reported between 1890 and 2015 in the literature Familial association has been reported in some cases [4], Two of them had pleural effusion [5,6]. Another two pediatric cases have been reported in 2016; a 9-year-old girl presented with RLM, gradually worsening kidney function and hyperparathyroidism [7] and an 11-year-old male patient presented with the history of fatigue, progressively increasing abdominal distension and bilateral flank pain and had a diagnosis of Renal Lymphangiectasia [8].
A third reported case in the same year of a 40-year-old female operated for uterine fibroid and endometriosis 2 years back presented with bilateral flank and lower abdominal pain, she had a previous ultrasound which suggested bilateral hydronephrosis due to mass effect of bulky uterus. Repeated Ultrasound examination of the abdomen revealed bilateral, multicystic fluid collections in the peripelvic spaces insinuating into the renal sinuses and displaying the bilateral pelvicalyceal system and no evidence of hydronephrosis on either side suggesting a diagnosis of RLM [9]. In 2017, Choudhury et al reported a case of bilateral renallymphangiectasia managed with percutaneous drainage together with sclerotherapy with favorable outcome [10].
The underlying pathogenesis involves non-communication between peri-renal and peri-pelvic lymphatic channels with the main lymphatics [11]. Pathologically, renal lymphangiectasia is characterised by cortical dilated endothelial-lined spaces, without glomerular or tubular abnormalities. The medulla is usually spared [12].
The diagnosis can be suggested by imaging, and chylous fluid aspiration is usually needed for confirmation. Some authors use the term (RLM) as a synonym for the commonly presenting peripelvic cysts (also termed renal sinus cysts) [13], instead the term should be restricted to patients with transrenalchylous cysts (which may comprise peripelvic cysts) which is much rarer and mostly seen in children [12].
Renal lymphangiectasia can be unilateral or bilateral-as in our case-, focal or diffuse [14]. Clinical manifestations include flank pain, hematuria and abdominal pain [15]. Other clinical presentations may include ascites, pyelonephritis and renal mass. Renal insufficiency has also been reported. The accumulated sub capsular fluid can compress the renal parenchyma resulting in high renin hypertension due to relative ischaemia, and secondary hypertension and this may explain the high serum creatinine and low eGFR in our case [12].
Renal lymphangiectasia can be misdiagnosed for other cystic renal masses, most commonly polycystic kidneys and cystic renal dysplasia. The major categories of cystic renal disease are which should considered in the diagnosis of renal lymphangiecsia [17]: (1) Genetic including autosomal dominant (ADPKD), and autosomal recessive polycystic kidney disease (ARPKD), juvenile nephronophthisis (JNPHP), medullary cystic kidney disease (MCKD), glomerulocystic kidney disease (GCKD) [17], (2) Developmental as Multicystic dysplastic kidney (MCDK), (3) The common acquired – Simple cysts, including medullary sponge kidney (MSK), (4) Cysts associated with systemic disease as tuberous sclerosis and Von Hippel-Lindau syndrome (VHLS), (5) Malignant cysts in part of renal cell carcinoma ,(6)Familial renal lymphangiomatosis which usually present by multiorgan involvement (including osseous) tissue and carries poorer prognosis. Other causes of bilateral renal enlargement should also be considered in the differential diagnosis including lymphoma [12].
The diagnostic imaging techniques mainly involve ultrasonography and CT. Ultrasonographic findings are usually variable including perirenal collection and peripelvic cysts, retroperitoneal fluid collection, ascites or features of fibrosis in the form of poor corticomedullary differentiation and diffuse echogenic renal parenchyma [12,15]. CT may show a perinephric fluid attenuation and peripelvic cysts in few cases. No other renal pathology is usually detected. Fluid collection in peritoneal or retroperitoneal compartments may also be noted.
There have been reports of two cases exacerbated by pregnancy [16] Aspiration of the cystic fluid is mandatory for diagnosis. The aspirated fluid is sterile, chylous fluid containing majority of lymphocytes, small amount of fat [4]. High levels of renin in the aspirated fluid confirms the origin to be renal [17]. Kidney biopsy is not easily used in diagnosis making as it can be complicated by persistent lymphatic leakage [12].
The natural history of this benign anomaly is not known [3]. However, like other lymphatic lesions, renal lymphangiectasia can appear suddenly, grow rapidly, cease growth, or even regress spontaneously [18].
Treatment is usually symptomatic and depends on whether or not the condition is bilateral. In the absence of symptoms conservative management is considered the best treatment; open or preferentially laparoscopic surgery is recommended to avoid recurrence in symptomatic patients[19].
Often renal impairment is mild, and treatment with antihypertensives is often sufficient in hypertensive patients. If there are significant mass symptoms, and the condition is unilateral, then nephrectomy may be indicated [20]. Percutaneous cystic drainage along with sclerotherapy showed favorable outcome in our case and also in a number of reported cases [10].
References
- Kull, P.A., et al., Clinical, clinicopathologic, radiographic, and ultrasonographic characteristics of intestinal lymphangiectasia in dogs: 17 cases (1996–1998). Journal of the American Veterinary Medical Association, 2001. 219(2): p. 197-202.
- Lorenz T and Ramseyer .Renal Lymphangiectasia1, Radiology 2001; 219:442–444
- Kabalin JN. Surgical anatomy of the genitourinary tract. In: Wals PC, Retik AB, Stamey TA, et al., eds. Campbell’s urology, 6th ed.Philadelphia: WB Saunders, 1992:31
- Nassiri, A.A., et al., Renal Lymphangiectasia: A Curious Cause of Pleural Effusion. Tanaffos, 2015. 14(3): p. 213-216.
- Bazari, H., et al., Case 23-2010. New England Journal of Medicine, 2010. 363(5): p. 463-475.
- Al-Dofri, S.A.A., Renal lymphangiectasia presented by pleural effusion and ascites. Journal of radiology case reports, 2009. 3(10): p. 5.
- Leite, A.F.d.M., et al., Renal lymphangiectasia: know it in order to diagnose it. Radiologia Brasileira, 2016. 49(6): p. 408-409.
- Arora, R., Bilateral renal lymphangiectasia — an unusual cause of abdominal distension and flank pain in a child. Quantitative Imaging in Medicine and Surgery, 2016. 6(4): p. 466-469.
- Bansal, K., et al., Renal lymphangiectasia: One disease, many names! Indian Journal of Nephrology, 2016. 26(1): p. 57-58.
- Choudhury, S., K. Sridhar, and K. Pal Dilip, Renal lymphangiectasia treated with percutaneous drainage and sclerotherapy, in International Journal of Adolescent Medicine and Health. 2017.
- Meredith, W.T., et al., Exacerbation of familial renal lymphangiomatosis during pregnancy. American Journal of Roentgenology, 1988. 151(5): p. 965-966.
- Stevenson, R.E. and J.G. Hall, Human malformations and related anomalies. 2005: Oxford University Press.
- Cohan, R. and E. Caoili, CT urography techniques. CT urography: an atlas. Lippincott, Williams & Wilkins, Philadelphia, 2006: p. 11-21.
- Merguerian, P.A., S.K. Sargent, and J.L. Dunn, Unilateral lymphangiectasis of the kidney: an unusual cause of renal enlargement in an infant. The Journal of urology, 1995. 153(2): p. 447-449.
- Ramseyer,L.T.,Case34:renal lymphangiectasia. Radiology, 2001. 219(2): p. 442-444.
- Meredith WT, Levine E, Ahlstrom NG, et al. Exacerbation of familiar renal lymphangiomatosis during pregnancy. AJR 1988; 151:965–966
- Pandya, V.K., et al., Bilateral Renal Lymphangiectasia. Journal of Clinical and Diagnostic Research : JCDR, 2016. 10(9): p. TD01-TD02.
- Leonidas JC, Brill PW, Bhan I, et al. Cystic retroperitoneal lymphangiomain infants and children. Radiology 1978; 127:203–208
- Tornero Ruiz JI, OjadosCastejon F, Nicolas Torralba J, e tal. [Bilateral renal lymphan giomatosis: conservative management]. xArch EspUrol2007; 60:812-4.
- Torres VE, Harris PC. Cystic Diseases of the Kidney. In: Skorecki K, Chertow GM, Marsden PA, Tool MW, Yu ASL, eds. Brenner and Rector's The Kidney. 10th ed. Philadelphia, Pa: Elsevier; 2015. 1475-1520.